Endometriosis: Symptoms, Causes, Treatment
Last Updated: Feb 29, 2024
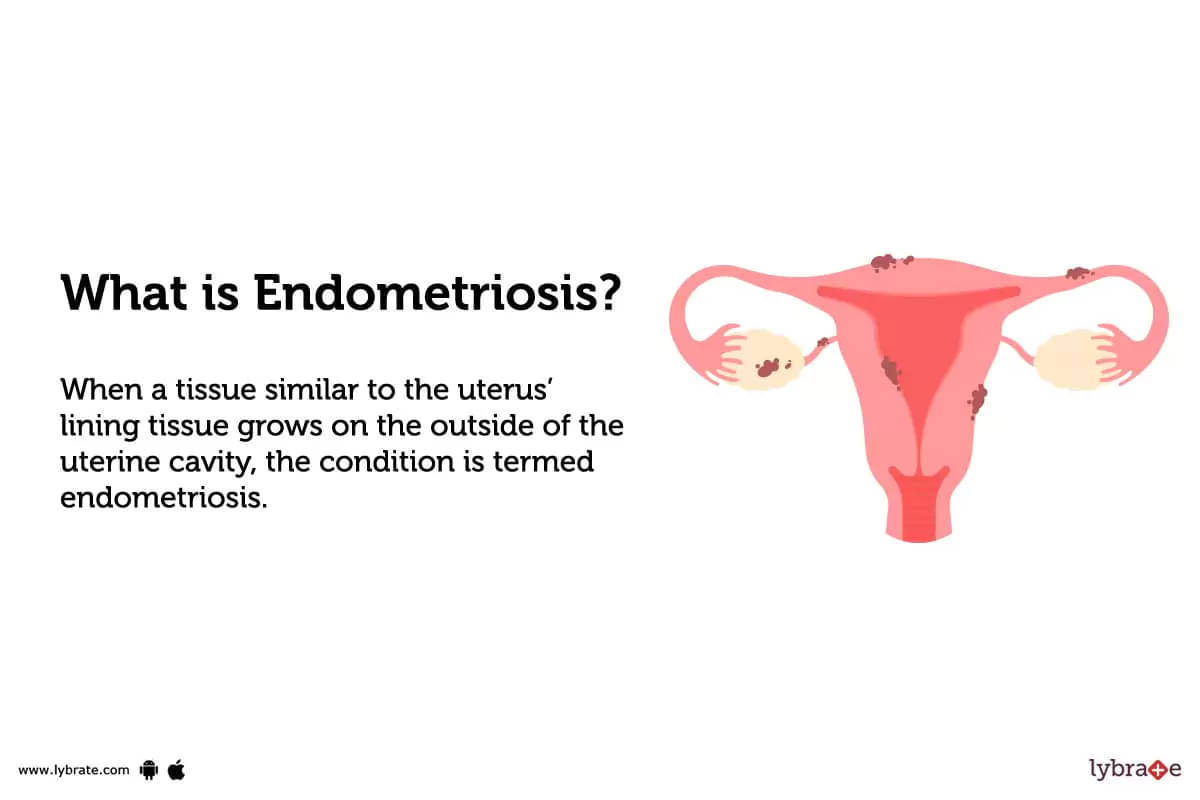
What is Endometriosis?
When a tissue similar to the uterus’ lining tissue grows on the outside of the uterine cavity, the condition is termed endometriosis. Similar to uterine tissues during periods, this tissue ruptures and you bleed when your menstrual cycle comes to an end. However, the blood is trapped and leads to the swelling of the surrounding tissues.
What are the types of Endometriosis?
There are mainly four types of endometriosis based on the abdominal area they affect:-
- Superficial peritoneal lesion: Most cases of endometriosis are of this type. Peritoneum, the thin film lining the pelvic cavity, will have lesions. Thus, it is also known as pelvic endometriosis.
- Endometrioma: Also known as an ovarian lesion, dark cysts filled with liquid (termed chocolate cysts) are present deep in an ovary (or both). In this case, the person runs the risk of damage to surrounding tissues that are in good shape.
- Deeply infiltrating endometriosis: Nearly 1-5% of endometriosis cases in women are of this type. The tissue grows under the peritoneum and might affect organs close to the uterus (such as bowels or the bladder).
- Abdominal wall endometriosis: In this case, the endometrial tissue develops due to a surgical incision and wound caused during a Caesarean section. Thus, the uterus lining-like tissue grows on the abdominal wall.
What are the symptoms of Endometriosis?
The signs and symptoms of endometriosis may vary from case to case. If you feel that you are at risk and show signs of endometriosis, look out for the following symptoms:-
- Pelvic pain (the most common symptom)
- Painful periods and back pain during it
- Severe menstrual cramps around 1-2 weeks of menstruation
- Unusual or heavy menstrual bleeding during/between your periods
- Blood in fecal matter or urine and painful bowel movement
- Pain during intercourse
- Tiredness and Fatigue that won’t go away
Regular gynecological exams can help recognize endometriosis while one is showing mild endometriosis symptoms.
What are the Stages of Endometriosis?
Endometriosis stages are designated based on the tissue spread, depth, and the areas of the body affected. Based on the results, the case is assigned one of these endometriosis stages:-
- Stage 1 endometriosis (Minimal) - Very few small wounds or lesions or implants might be found on the organs or the pelvic/abdominal lining. In the case of stage 1 endometriosis, no scar tissue can be found.
- Stage 2 endometriosis (Mild) - There are more wounds/lesions/implants located deeper in the tissue. There might also be some scar tissue.
- Stage 3 endometriosis (Moderate) - The number of deep tissue implants is high and you might also have minor cysts on your ovary(s). Moreover, there might also be thick bands of scar tissues known as adhesions.
- Stage 4 endometriosis (Severe) - Most cases of endometriosis belong to Stage 4 endometriosis. Your doctor will find several implants that are deep in the tissue and numerous wide adhesions. Unlike stage 3 endometriosis, the cysts on one or both ovaries in this case are quite large.
One might not go from one endometriosis stage to another, but leaving it untreated can worsen the patient’s condition.
What are the causes of Endometriosis?
Doctors are not clear on the exact cause of endometriosis, but some common endometriosis causes include:-
- Menstrual blood that contains endometrial cells moves into the pelvic region through the Fallopian tubes (retrograde menstruation). These cells might stick to the pelvic cavity’s organs and cause endometriosis.
- If one’s mother or sister has endometriosis, they are more likely to be diagnosed with the condition. Studies suggest that the condition worsens from generation to generation, which is why regular gynecological examinations are necessary.
Some women with endometriosis suffer from immune response conditions and have an altered system, impairing the body’s function to perceive ectopic endometrial tissue. Doctors, however, have not established the validity of this claim.
Does endometriosis cause infertility?
It has been observed that endometriotic women face issues while trying to get pregnant. Nearly 30-50% of these women might experience infertility. However, it is estimated that around 70% of women with mild or moderate endometriosis might conceive within three years without treatment.
Endometriosis causes physical and hormonal changes, which can impair the body’s reproductive capability in several ways. Some of these changes that might cause infertility include:-
- Distorted pelvic anatomy
- Adhesions
- Scars on Fallopian Tubes
- Inflammed pelvic structure
- Immune system changes
- Impaired pregnancy implantation
- Changed hormonal environment and quality of the eggs
Stage 4 endometriosis causes considerable scarring, blocks the fallopian tubes, and damages the ovaries, causing difficulty in getting pregnant.
How can you prevent endometriosis?
As of now, researchers and doctors do not know about any way to prevent endometriosis, but you can try to manage your body’s estrogen levels to reduce the probability of being affected. Additionally, you can manage the symptoms and decrease the discomfort to some extent. Certain measures you can adopt to reduce your estrogen levels include:-
- Use hormonal birth control methods with lower doses of estrogen - Birth control pills, patches, and vaginal rings with low estrogen levels are available. You could opt for hormone therapy, but the effects will cease as soon as you stop taking the hormones.
- Exercising regularly for a lower body fat percentage - A study suggests that exercise helps boost estrogen metabolites, the compound that breaks down estrogen, and might help lower the risk of endometriosis.
- Avoiding alcohol - Drinking alcohol can raise the body’s estrogen levels, increasing the chances of endometriosis. Doctors recommend that women who choose to drink should not consume more than one alcoholic drink each day.
- Avoid caffeinated drinks like sodas - This specific point is disputed among researchers and doctors. A study found that people who consume caffeinated drinks like green tea and soda in moderation had higher estrogen levels. However, nearly eight studies disapproved of this and found no direct link between endometriosis and caffeine.
Do’s in Endometriosis
- Track your symptoms and condition throughout the day to provide your doctor with a compact report
- Regular exercises, meditation, and yoga can help manage endometriosis better
- Take your medications as advised by healthcare experts and professionals
- Maintain your diet and eat fresh fruits and vegetables after thoroughly washing them
- Consume water and decaf drinks in place of caffeinated drinks to stay hydrated
Don’ts in Endometriosis
Endometriosis - Diagnosis and Tests
If your doctor suspects that you display endometriosis symptoms, they will perform some tests on you to confirm your condition. These might include:-
- Pelvic Exam - The doctor will be able to feel the cysts/scars (if any) behind your uterus
- Imaging Tests - A CT scan, an MRI, or an ultrasound provides a detailed view of the organs to check whether the endometrial tissue has caused any damage or not
- Laparoscopy - The doctor makes a small cut in the belly and a laparoscope (a thin tube with a camera on one end) is inserted to check the size of the lesions. Laparoscopy is the only definite procedure to check if one has endometriosis or not
- Biopsy - During laparoscopy, the doctor takes a simple tissue and checks it under the microscope to confirm whether you have endometriosis
Are there any complications that can be expected due to Endometriosis?
Stage 4 endometriosis or severe endometriosis can hamper your lifestyle quality. The hormonal changes can lead to a struggle with anxiety or depression, making it imperative to seek mental health care. Endometriosis leads to an increased risk of ovarian cancer or another type of cancer known as endometriosis-associated adenocarcinoma.
Fertility issues are another serious endometriosis complication, mostly seen in people with stage 4 endometriosis. Cases that are a milder form of endometriosis can conceive within a few years and may carry the baby to term. The medications used to treat endometriosis show no improvement in fertility. However, some women were able to reproduce without any difficulty after endometriosis surgery .
We suggest you talk to your doctor to understand whether you are at risk of these side effects and how you can cope with them. Rest assured, medical experts at Pristyn Care will try their best to avoid any complications.
Home Remedies of Endometriosis
Medical surgery is the only effective treatment for endometriosis, but there are several home remedies that you can adopt to get temporary relief from the symptoms. Follow these until you are due for the surgery:-
- Heating Pads - Heat helps relax the pelvic and abdominal muscles providing relief from cramps and pain. Hot water bottles and warm baths along with heating pads can prove to be useful.
- Over-the-counter Anti-Inflammatory Drugs - Nonsteroidal OTC anti-inflammatory drugs offer quick relief from cramps caused due to endometriosis. Some of these popular drugs are ibuprofen and naproxen. Ensure that you do not take these on an empty stomach and stay hydrated to prevent indigestion or stomach ulcers.
- Castor Oil - Massaging castor oil onto your abdomen along with a few drops of calming essential oils like lavender/peppermint can help relax the pelvic muscles.
- Turmeric - Its strong anti-inflammatory properties can help manage endometriosis symptoms. Some studies also suggest that turmeric has the ability to inhibit the growth of endometrial tissues.
- Modify Your Diet - Avoiding foods that cause inflammation and consuming foods with anti-inflammatory properties can help manage long-term endometriosis, but this will not provide fast relief.
- Pelvic Massages - Endometriosis can cause pelvic and abdominal pain. Pelvic Massages can be effective in reducing inflammation, relaxing the pelvic muscles, and reducing abdominal cramps. Do not perform pelvic massages during your treatment and use them only before your menstrual cycle.
- Ginger Tea - Nausea and indigestion are common side effects of endometriosis. Ginger tea is a safe and effective home remedy to manage nausea.
What to Eat in Endometriosis?
Consuming a nutrient-dense, well-balanced diet is important to manage the inflammation and pain due to endometriosis. Increase the consumption of these foods for further relief and pain management:-
- Fiber-rich like lentils, fruits, vegetables, chia seeds, and baked beans
- Foods rich in iron like broccoli, beans, nuts, seeds, and dark leafy greens
- Foods consisting of essential fatty acids like walnuts, chia seeds, flax seeds, salmons, and sardines
- Antioxidant-rich foods like dark chocolates, spinach, oranges, and berries
You could seek the advice of a registered dietitian and your primary healthcare provider to plan meals that work the best for you.
What Not to Eat in Endometriosis?
Particular habits and choices can increase your endometriosis condition and several other severe ones. However, concrete and adequate studies correlating certain foods/lifestyle habits with endometriosis are lacking. The following foods and factors might have a negative impact on endometriosis:-
- Foods high in trans fat such as fried, processed, and junk foods
- Red meat or Processed meat
- Gluten in bread and pasta
- High FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) foods
Endometriosis Treatment
The side effects and pain associated with endometriosis hampers a person’s regular lifestyle and can lead to further potential complications. Some common endometriosis treatment options include:-
- OTC Pain Medications - OTC medications can help provide relief from endometriosis pain but are not effective in all cases
- Hormone Therapy - Hormone therapy is effective in reducing the body’s estrogen levels, which might relieve the pain and stop the progression of endometriosis.
- Contraceptives - Some hormonal contraceptives reduce the chances of pregnancy by preventing the growth of endometrial-like tissues. Thus, birth control pills, patches, and vaginal pains might help reduce or eliminate the pain in stages 1 and 2 of endometriosis.
- Surgical Treatment - Surgical treatment for endometriosis helps treat even severe cases, such as stage 4 endometriosis. These can be further broken down into two types-
- Laparoscopic Surgery - Endometriosis Laparoscopic Surgery is used to visualize and diagnose endometriosis. Moreover, it is minimally invasive and does not have any severe side effects. The displaced or abnormal tissues that are similar to the endometrial ones are removed by making small incisions in the abdomen.
- Hysterectomy Surgery - In the case of severe cases where other treatments have failed, your doctor will suggest a hysterectomy. In this last-resort surgery, the surgeon will remove your uterus or cervix, visible implant lesions, and ovaries (in some cases).
Endometriosis Treatment Without Surgery
As discussed, the non-surgical methods of endometriosis treatment include hormone therapy and pain medications. It is important to note that these might not be too effective in severe endometriosis cases, which is why your healthcare provider might suggest you opt for surgical treatment for endometriosis.
Which are the Best Medicines for Endometriosis?
Some medicines that can be used to ease endometriosis pain and allow you to feel better include:
Endometriosis Surgery
Your overall health, medical complications, and age determine whether endometriosis surgery is the best treatment for you or not. You need to talk to your doctor about choosing surgery if you experience severe pelvic pain, have difficulty getting pregnant, or if your medications do not work. Based on your conditions, your doctor will either advise you to have laparoscopic surgery or a hysterectomy.
How Long Does It Take To Recover From Endometriosis?
After an endometriosis laparoscopic surgery, you might feel fatigued in the following days and are advised to go without driving for 2 weeks. The doctor will advise you to hold off activities like swimming, bathing in a bathtub, and having sexual intercourse for about 2 weeks to allow you to recover from the procedure.
Recovering from laparotomy surgery is relatively slower and is more painful. Several everyday activities will be off the charts while you recover at home.
If you have a hysterectomy, your periods will stop as the cervix/uterus has been removed. In case the surgeon has also removed your ovaries, you will go into menopause and might experience symptoms like hot flashes and bone density loss. Your healthcare provider will try their best to ensure that you do not face these side effects and will help you recover from them.
What is the price of Endometriosis treatments in India?
Endometriosis is a condition that causes great discomfort and cramps, which is why endometriosis treatment is important. The average cost of endometriosis surgery in India is between 60,000 to 80,000.
Are the results of the treatment permanent?
Unfortunately, there is no cure for endometriosis, but one can expect a reduction in discomfort with the help of endometriosis treatment . Even if you choose the surgical treatment for endometriosis, the condition can return in the future.
Who is eligible for the Endometriosis treatment?
As of now, anyone can get endometriosis treatment. However, the statement might not stand true as every case is not the same. Hence, it is advised you talk to your doctor and seek their opinion before choosing one of the available treatments. Your doctor needs to check your case and take into account any complications before they proceed with the treatment.
Who is not eligible for the Endometriosis treatment?
As discussed, a particular treatment might not be suitable for you. For example, if you are thinking of starting a family, a hysterectomy might not be the correct option for you. We recommend talking to your doctor to understand the effects and complications (if any).
What are the post-treatment guidelines for Endometriosis treatment?
You need proper care to fully recover from an endometriosis treatment procedure . After the surgery, you might experience -
- Grogginess and nausea due to the anesthesia
- Discomfort due to improper bowel movement
- Mild pain at the incision site and a sore abdomen
- Vaginal bleeding and mood swings
To reduce the discomfort and make a full recovery, you will need to avoid certain activities like exercising, lifting, stretching, swimming, and sexual intercourse. You might need a week or more before you can perform regular activities and get back to an active lifestyle. Some tips to further ease the recovery process include -
- Adequate rest and a nutritious diet
- Stay hydrated and perform small movements to avoid indigestion
- Wear loose clothes to avoid rubbing the incision site
- Contact your doctor if you notice something unusual or experience complications
Which specialization doctor treats endometriosis?
Treating endometriosis might need an entire team of healthcare experts to ensure you get the care and diligence you need. Some common specialists for endometriosis treatment include, but are not limited to, are:
- Obstetrician-gynecologist
- Reproductive endocrinologist
- Gastroenterologist
- Pain Management Specialist
- Mental Health Professionals
What are the side effects of Endometriosis treatments?
Some common side effects of endometriosis treatments include:-
- Hot flashes and tiredness
- Insomnia and headaches
- Joint and Muscle Stiffness
- Bone Density Loss
- Vaginal Dryness
- Mental Health Problems
Endometriosis - Outlook / Prognosis
Endometriosis is a chronic condition and researchers have not yet figured out the exact causes. As of now, there is no fix for the disorder, but researchers and scientists have found effective treatments like hormone therapy and surgery. Managing the side effects and complications like fertility issues is somewhat possible. Additionally, research suggests that the symptoms of endometriosis improve after menopause. In case you notice any symptoms and suspect that you might have endometriosis, you need to consult your doctor as soon as possible to create a treatment plan.
Frequently Asked Questions (FAQs)
Why does endometriosis cause brown discharge?
Why does endometriosis cause nausea?
Why is my endometriosis pain worse at night?
What causes endometriosis flare-ups?
Is there any difference between adenomyosis and endometriosis?
Can a colposcopy detect endometriosis?
Can a woman with endometriosis become pregnant?
References
- Uterine Cancer- Medline Plus, Health Topics, NIH, U.S. National Library of Medicine [Internet]. medlineplus.gov 2019 [Cited 27 July 2019]. Available from:
- Living with endometriosis- Medline Plus, Medical Encyclopedia, NIH, U.S. National Library of Medicine [Internet]. medlineplus.gov 2019 [Cited 27 July 2019]. Available from:
- Endometriosis- Medline Plus, Medical Encyclopedia, NIH, U.S. National Library of Medicine [Internet]. medlineplus.gov 2019 [Cited 27 July 2019]. Available from:
Table of content
15+ Years of Surgical Experience
All Insurances Accepted
EMI Facility Available at 0% Rate
Find Gynaecologist near me
Ask a free question
Get FREE multiple opinions from Doctors