Hysterectomy: Purpose, Procedure, Benefits and Side Effects
Last Updated: Jul 06, 2023
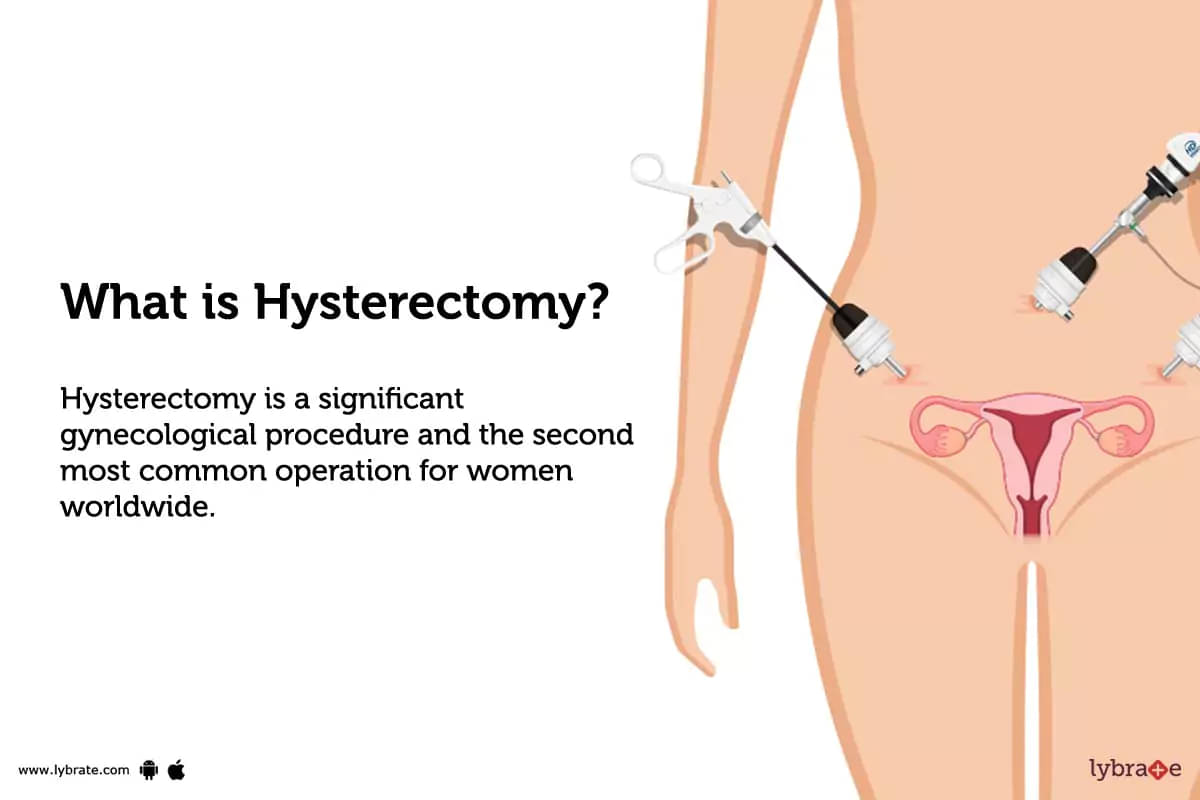
What is hysterectomy?
Hysterectomy is a significant gynecological procedure and the second most common operation for women worldwide. During a hysterectomy, the uterus is surgically removed simply due to the fact that the uterus tends to acquire a number of uterine-related health concerns as a woman ages and approaches menopause, including heavy vaginal bleeding, excruciating stomach pain, blackouts, nausea, persistent exhaustion, and weakness.
The most frequent cause is the growth of uterine fibroids, however in unusual circumstances, the uterus's size or form may alter.
Some women experience frequent urinary tract infections as well as difficulties urinating and defecating due to uterus prolapse- which is the term for uterus shifting from its normal position. A hysterectomy is required in either of these situations. It guarantees rapid relief and offers a complete and irrevocable remedy to uterine issues.
Hysterectomy, which is a rather routine and secure procedure, is also carried out as a last resort for endometriosis. But it always puts an end to your ability to have children biologically.
Types of hysterectomy
There are numerous hysterectomy procedures. Depending on why you require the procedure and how much of your womb and associated reproductive system can be safely preserved, you may have one of many types of available hysterectomy procedures;
Total hysterectomy
The most oftenly done procedure is a complete hysterectomy, which involves removing both the womb and the cervix.
Subtotal hysterectomy
In this the cervix is left intact while the uterus is removed. Some women believe that the cervix serves a role during penetrative intercourse, despite the fact that removal is typically advocated due to it being a potential cancer location.
Total hysterectomy with bilateral salpingo-oophorectomy
It involves the removal of the womb, cervix, fallopian tubes, and ovaries. This procedure is carried out if the patient has uterine or ovarian cancer, persistent discomfort brought on by recurring pelvic infections, or recurrent endometriosis.
Radical hysterectomy
During a radical hysterectomy, the uterus and its surrounding tissues are removed, along with the ovaries, fallopian tubes, part of the vagina, long with any accompanying pelvic ligaments and lymph nodes and fatty tissue.Hysterectomy with prophylactic bilateral salpingectomy
Hysterectomy with prophylactic bilateral salpingectomy
Most doctors now advise removing the fallopian tubes at the time of hysterectomy due to evidence suggesting that early 'ovarian' malignancies start in the tubes. This is done if the lady has cancer of the cervix, ovaries, fallopian tubes, or uterus.
Three Different Methods of Hysterectomy
Based on how the hysterectomy has been performed the procedure could be further segregated into three methods:
- Laparoscopic hysterectomy: Also known as keyhole surgery, it involves a series of small incisions in the abdomen to remove the uterus.
- Abdominal hysterectomy: The womb is removed by a larger cut in the lower abdomen that gives the surgeon a complete and finest view of all your abdominal organs.
- Vaginal hysterectomy: The removal of the womb through a cut in the upper part of the vagina.
Benefits of hysterectomy:
Every surgical operation aims to treat or avoid issues. Any type of hysterectomy that is performed to remove organs, include following benefits:
- Stopping excessive, unusual bleeding
- Relieving persistent pain
- Reestablishing painless sex
- Avoiding cancer
- Getting rid of malignant tissue
- Raising the standard of living
Why is hysterectomy done?
The uterus is removed during a hysterectomy. There are several reasons to have this procedure, including:
- Uterine fibroids that hurt, bleed, or present other issues
- Uterine prolapse, which refers to the uterus moving from its usual position into the vaginal canal
- Ovarian, uterine, or cervical cancer
- Endometriosis
- Unexpected vaginal bleeding
- Persistent pelvic discomfort
- Unsuccessfully treated pelvic inflammatory disease (PID) that is caused by bacterial infection of the female reproductive system
- Adenomyosis, or uterine thickening
When all other treatment options have failed, hysterectomy for non-cancerous causes is typically the last resort.
What are the risks of hysterectomy?
Some of the possible complications are:
- Bladder or bowel damage
- Vaginal bleeding
- Blood clots under the sutures/haematoma
- Internal scar tissue in the abdomen
- Early menopause
- Infection
- Ovary failure
- Ureter damage
- Vaginal problems
- Pelvic floor prolapse
- Fistula, a rare irregular gap between internal organs like the bowel and the vagina
- General anesthetic complications
- Internal hemorrhage or bleeding
If you weren't properly counseled before the hysterectomy, you can also have emotional trouble.
How do I prepare for hysterectomy?
When you are scheduled for a hysterectomy surgery, you can be requested to do the following:
- Your doctor may advise a bowel cleanse prior to any abdominal surgery
- It's crucial to take proper rest before the surgery, and if you're feeling particularly nervous, try deep breathing
- You are not supposed to eat or drink anything prior to your surgery. Do not even drink the water. Just sip it or gulp with your saliva if you are taking any suggested medicine
- You should take off any jewelry before surgery
- Take a bath before reaching hospital with preferably with an antibiotic soap
- Shave your lower abdominal area to prepare yourself for surgery
- Prefer wearing loose gowns or something that doesn't fit on your waist
- Tell your doctor the medication or any supplements you are on
- Stop taking blood thinning medicines
- Arrange someone to take you home back from the hospital and help you around the house
How is hysterectomy done?
A six to eight-inch surgical incision is made to remove the uterus from the abdomen. The most frequent signs and symptoms for this treatment include the removal of the ovaries and fallopian tubes, an enlarged uterus, huge fibroids in women, or a condition that has progressed to the pelvic cavity, such as endometriosis or malignancy. The primary surgical incision can be done either horizontally along the top of the pubic hairline or vertically from the navel to the pubic bone.
It could be essential to create a vertical incision in the lower abdomen if the uterus is particularly big or if there is a scar from a previous procedure.
Before the procedure
- A consent document will be signed by you
- You will be changed into hospital gown
- You will be laid down on a operation table on your back
- All your vitals will be checked and monitored throughout the procedure
- The area around the abdomen and vagina is cleansed with an antibiotic solution to keep the infection at bay
- You might be connected with breathing pipe attached to a ventilator
- General anesthesia will be administered either via chemical vapors or intravenously
During the procedure
The surgical procedures may differ as a result of the process's various ways. Here is the detailed procedure of some of the hysterectomy methods that are available to excise the uterus;
- Open Surgery Hysterectomy: The uterus is removed during surgery on the lower abdomen by making a vertical or flat incision of 5-7 inches from the surrounding tissue. The skin is then closed with stitches or staples once the tissue has been sutured together, creating a visible scar. Typically, 2 to 4 days are spent in the hospital after this procedure.
- Vaginal hysterectomy: A cut is made through the incision in the vagina where the uterus was removed during a vaginal hysterectomy. Because the cutting is subsequently completed with dissolvable sutures, there is no visible scar left behind.
- Laparoscopic hysterectomy: A minor incision from the abdomen or a single cut from the belly button is used to employ a tube with a fitted tiny camera, light, and surgical tools. The procedure can be seen live on a screen which is taken as a reference for the surgeons to know what they are doing.
- Laparoscopic-assisted vaginal hysterectomy: The uterus is removed through an incision made from the vagina using laparoscopic surgical tools.
- Robotic-assisted Laparoscopic Hysterectomy: Using cutting-edge robotic surgical equipment, the physician conducts the procedure away from the patient while observing it in three dimensions using just natural wrist motion. In challenging situations, such as dissection near the ureters, bladder, or blood arteries, this procedure is very beneficial.
After the procedure
- You can feel worn out and in some pain and discomfort when you wake up in the recovery room after a hysterectomy. This is typical following this kind of surgery and can be managed with painkillers
- Your nurse can administer medication to help you feel better if you have nausea following the anesthetic
- Dressings will be applied on your wounds
- Catheter, a tiny tube will be used to drain urine from your bladder into a collecting bag within 24 hours of surgery, unless your bladder was traumatized during surgery, in which case it will remain in longer.
- A drip will be inserted in your arm to give you medicines intravenously. Have the intravenous (IV) tube removed from your arm sometime during the first few days, depending on the procedure and your condition
- A drainage tube in your belly to remove any blood from your wound's (if you underwent an abdominal hysterectomy) - Typically, these tubes are left in place for one to two days
- If you've had a vaginal hysterectomy, a gauze pack may be put into your vagina to reduce the chance of bleeding; this pack typically remains in place for 24 hours
- Additionally, you could feel a little uneasy and like you need to poop
- A physiotherapist could demonstrate some mobility-enhancing exercises for you
- To aid with your recovery, they could also demonstrate some exercises for your pelvic floor muscles
- Your ability to pass pee normally should return once the catheter has been taken out
- After your procedure, any sutures that need to be removed will be done so after 5 to 7 days.
How much does hysterectomy cost?
In India, hysterectomy surgery typically costs between Rs. 55,000 and 75,000. However, the costs may range based on the hospitals in other cities.
Laparoscopic hysterectomy costs in India typically fall between INR 55,000 and INR 75,000. However, as with any operation, the precise cost may vary a bit based on the method used for your hysterectomy, the components removed, your choice of gynecologist, their level of experience, the location of the hospital, as well as additional medical and non-medical costs.
However, the following is a summary of the approximate costs for laparoscopic uterus removal in several Indian metropolises:
- A lot of variables may affect the cost of surgery. Along with tier-1 or tier-2 cities; hospital or clinic brand names, the fees of the treating consultant, admission fee, type of the surgery, post-surgical complications that are involved, admission room that you opted for, may have an influence on hospital billing expenses.
- The total cost of the procedure may also be impacted by the number of diagnostic tests performed. The entire cost of the surgery may decrease based on the patient's insurance plan.
What to do after hysterectomy?
Be directed by your doctor, but here are some basic recommendations during the first four to six weeks following surgery:
- For at least two weeks, try to get as much rest as you can. Driving is not recommended at this period.
- Practice the exercises you were demonstrated in the hospital and prefer doing when lying down. Also, take a small walk every day around the house.
- In the initial days following surgery, try to avoid standing for longer than a few minutes at a time. Increase your standing time as your recovery progresses.
- Take care of your surgical incisions and keep them dry.
- Four to five days following surgery, you should have your first bowel movement.
- After surgery, your bowel requires some time to heal. You ought to be passing 'gas,' also known as flatus, by the time you are released. You could feel 'gas' pain. Walking and consuming hot drinks will both help you feel better.
- To prevent constipation, drink lots of fluids and consume fresh fruits and vegetables.
- For the first few days, you might be advised to use stool softeners.
- Up to eight weeks of vaginal discharge is possible.
- Some women have an increase in vaginal bleeding for 24 hours two weeks following surgery. That is typical. Call your doctor, though, if it persists or is quite heavy.
- Avoid hard lifting and stretching.
- Avoid intercourse until after the post-operative check (approximately four to six weeks after the procedure), to ensure the vagina is properly healed.
- If antibiotics have been recommended, make sure to take the whole course, even if you feel OK.
- It could be beneficial to use a lubricant, sweet almond oil, or olive oil if vaginal dryness is an issue.
What to eat after hysterectomy?
Consume a balanced diet that includes protein, fruits, and vegetables to aid in the healing process following surgery. To keep your body well hydrated, consume 8 to 10 glasses of fluids daily, preferably water. Increase your fiber consumption if you are prone to constipation. By including following foods in your diet plan many issues can be solved post-hysterectomy surgery;
- Fruits
- Vegetables
- Legumes
- Onions
- Garlic
- Leeks
- Chicory
- Jerusalem artichoke
- Root vegetables
- Rice
- Yogurt
- Fermented drinks
- Cereals
- Fibre supplements
- Water
- If you want assistance with your nutrition, please consult a dietitian.
Is hysterectomy safe?
Hysterectomy surgery is highly safe with very few risks and complications involved that can be managed either by medication or therapies. One of the main advantages of hysterectomy is that it can successfully manage life-threatening conditions like cancer and can also give the patient quality life.
Is hysterectomy painful?
Hysterectomy surgery in itself isn’t a painful procedure as it is performed under general anesthesia and the patient only feels just the sting of the needle before slipping into deep sleep. Later, depending upon the procedure carried out, pain can vary, which is manageable with painkillers and right after care.
How long does it take to recover from hysterectomy?
Factors like age, general state of health of the patient and type of hysterectomy determine how long it takes for the patient to feel well enough to leave the hospital. Most women spend 2-3 nights in the hospital following surgery, followed by 4-6 weeks of decreased activity. It often takes up to five days before someone who has had an abdominal hysterectomy is released from the hospital.
In 4 to 6 weeks, you could be asked to visit your general practitioner, but unless there are issues, you won't typically need to schedule follow-up hospital visits.
After an abdominal hysterectomy, recovery takes between 6 and 8 weeks. Whereas, recovery periods following less invasive surgical methods like a vaginal or laparoscopic hysterectomy are frequently shorter.
What are the side effects of hysterectomy?
- Vaginal discharge
- Surgical wound infections
- Thrombosis
- Ureter harm
- Urinary tract disease or constipation
- Emotional imbalance
Hysterectomy Aftercare:
Follow the instructions provided by your doctor.
- It's crucial to keep the incision clean and dry after you get home. Your doctor will give you detailed bathing instructions, frequently advising you to hold off on using a bathtub for at least 4 weeks. Depending on the specifics of your operation, doctors may have different views on washing.
- You can take a shower right away, but make sure the water runs over the incision rather than directly on it. Dry tissue near the wound can be carefully washed away. Instead of rubbing, be sure to gently pat the surface dry entirely.Most likely, you'll bring staples or steri-strips home (thin, white Band-Aids). They'll aid in the healing of your wound. In addition to sutures, staples are metal clips that are used to assist seal the wound.
- Around the stitches or staples, your incision may appear a little red. That is typical. Following surgery, the staples are removed 10–14 days later. Steri-strips can be used after the staples have been removed. With the staples or steri-strips in place, you can take a shower. You may peel off the steri-strips as they start to curl up. Your incision's color will progressively lighten and disappear over time. This will take six to twelve months.
- Every day, look for signs of inflammation, edema, drainage, or a wound opening around your incision.
- If you have drains, you can wash by having a sponge bath or a shower. Just be sure to thoroughly dry the area around the drain and the incision.
- Wear comfortable, loose-fitting clothes that won't irritate or rub the incision region. To avoid discomfort from your clothing, you can cover the incision with a fresh piece of gauze.
- You should try to take a walk every day, this promotes healthy blood flow and lowers the possibility of issues like leg blood clots (deep vein thrombosis).
- Try to avoid standing for longer than a few minutes at a time. As your rehabilitation develops, you can increase your standing time. Avoid hard lifting and stretching.
- Eat fresh fruits and vegetables and drink lots of water to prevent constipation.
- If you have been prescribed antibiotics, make sure you finish the entire course of treatment, even if you feel fine.
- Nothing should be inserted into your vagina. Tampons, douching, and having sexual contact all fall under this category. As soon as the injury has sufficiently healed, your doctor will let you know. Normally, this takes place in eight weeks.
- Avoid exposing the incision area to direct sunlight. Additionally, unless otherwise directed, avoid applying any creams or lotions directly on the incision.
- It could be beneficial to use a lubricant, sweet almond oil, or olive oil if vaginal dryness is an issue.
Conclusion:
Although a hysterectomy may be the most efficient course of action for patients suffering from a number of complicated conditions of the reproductive system, gynecological experts view it as a last resort due to its invasive nature, higher risk of complications and potential risk of permanent infertility due to uterus extraction.
References
- Hysterectomy- Medline Plus, Health Topics, NIH, U.S. National Library of Medicine [Internet]. medlineplus.gov 2019 [Cited 03 August 2019]. Available from:
- Hysterectomy- Medline Plus, Medical Encyclopedia, NIH, U.S. National Library of Medicine [Internet]. medlineplus.gov 2019 [Cited 03 August 2019]. Available from:
- Hysterectomy- Office on Women's Health, U.S. Department of Health & Human Services [Internet]. womenshealth.gov 2018 [Cited 03 August 2019]. Available from:
Table of content
15+ Years of Surgical Experience
All Insurances Accepted
EMI Facility Available at 0% Rate
Find Gynaecologist near me
Ask a free question
Get FREE multiple opinions from Doctors