Fallopian Tubes Block and Infertility- What's the solution
Introduction
When couples get married, they often view parenthood as the next stage in their family life. They want to have a child, they want to be “mom” and “dad”, they cannot imagine that this may be hard to achieve or may not be a natural process. When several trials to conceive fail, they are shocked. Their basic expectation about family life gets shattered. Most of the couples are desperately looking for medical therapy that will end into a misery. Clearly this is not a struggle to survive; it is a struggle to fulfill a dream, to achieve what they view as a “full life”.
What is needed for pregnancy?
In the male partner, sperms are normally produced in the testes after puberty (after attainment of characters like growth of beard, moustache etc). From the testes, they are carried through the sperm conducting ducts (epididymis, vas, seminal vesicle and prostate gland). Then during sexual stimulation, after proper erection and ejaculation, they come out through penis. During sexual intercourse, these sperms, present in semen, are deposited inside the vagina.
In female partner, the deposited sperms must travel from vagina through the cervix (the mouth of the uterus). The cervix acts as gate-keeper, a it prevents entry of dead and abnormal sperms as well as bacteria present in semen, in the uterus. From uterus,sperms reach the Fallopian tubes (the tubes that are attached to the both sides of the uterus) where the sperms must meet the egg (ovum). The eggs are produced only before birth and so, there are fixed number of eggs inside the ovary. The ovum released from the ovary, into the abdomen at the time of ovulation (rupture of the surface of ovary to release the ovum). That ovum must be taken by the tube and thus inside the tube an embryo (earliest form of the baby) is formed, by meeting of the egg and the sperm.
It should be mentioned that out of nearly 200-300 million sperms, in average, deposited in vagina, hardly 500- 800 sperms can reach near the eggs and only one will succeed to form the embryo. The embryo then travels through the tube into the uterus and the uterus attaches the embryo firmly with it and thus the pregnancy starts. So, if there is defect in any one of them there will be difficulty in achieving pregnancy.
Thus, to summarise, pregnancy requires
- Production of healthy (“Normal Morphology”) and movable (“Normal Motility”) sperms in adequate number (“Normal Count”) in the testes
- Transport of these sperms through the sperm conducting ducts from testes to penis
- Successful Erection and Ejaculation during Intercourse to deposit adequate number of these sperms in the vagina
- Transport of these sperms from vagina through cervix to the uterus and the tubes
- Presence of sufficient number of eggs inside the ovary and ability to release the eggs from the ovaries
- Pick up of the eggs by the tubes
- Approximation of eggs and the sperms to form the embryo
- Transport of embryo from the tubes into the uterus
- Acceptance of the embryo by the uterus and its growth
What is Infertility?
Literally, the word “Infertility” means inability to conceive. But in reality, there are very few couples, who have no chance of natural conception and are called “Absolutely Infertile”. In fact, in many couples who present to infertility clinics, pregnancy may be the matter of time, thus the chance factor.
It should be kept in mind that, if there is factors to question fertility of either male or female or the female is of age less than 35 years; after one cycle (one month) of regular frequent intercourse, the chance of conception in human being is only 15%. That means, out of 100 couples trying for conception, only 15 will be able to succeed after one month of trying. The word “Regular” and “Frequent” are important; because to achieve pregnancy, couples are advised to keep intimate relationships for at least 2-3 times a week and this should be increased particularly around the time of ovulation (Middle of the menstrual cycle). Thus chance of pregnancy after 6 months, 12 months and 24 months of regular trying are respectively 60%, 80% and 100%.
The word, “Subfertility” seems better and more scientific than “Infertility”, to describe the couples who have reduced chance of conception, due to any cause. However, the word “Infertility”, seems more popular, although it puts pressure on the couples. In most cases, usually we advise to investigate after one year of regular and frequent intercourse, when the couples fail to conceive. However, if there are factors to question fertility; for example female with age more than 35 years, or with previous surgery in tubes/ ovaries/ uterus or known diseases like PCOS or endometriosis; or male partner having surgery in scrotum or groin or any hormonal problems or sexual dysfunctions- the wait period is usually reduced and couples can be investigated, even soon after marriage.
What causes Infertility?
Please look at the point “Thus, to summarise, pregnancy requires” where 9 points have been mentioned.
Thus the common causes may be
- Problems in male- total absence of production of sperms, less than adequate number of sperms, problems in morphology and motility of sperms (most sperms not healthy or movable), blockage in transport of sperms and inability to deposit sperms in the vagina (sexual dysfunction- Erectile Dysfunction or less commonly, Ejaculatory Dysfunction). Examples include hormonal problems (Testosterone, thyroid, prolactin), diabetes, liver problems, causes present since birth, chromosomal abnormalities, surgery, infection, sexually transmitted diseases, smoking, exposure of scrotum to high temperature, some medicines or psychological causes.
- Problems in female- total absence of less than adequate number of eggs in the ovaries, problems in ovulation, problems in picking of eggs by the tubes, blockage of tubes, problems in conduction of sperms or embryo by the uterus, problems in accepting the embryos by the uterus. Examples include causes present since birth, chromosomal abnormalities, polycystic ovarian syndrome (PCOS), old age, increased weight, fibroid, endometriosis, pelvic inflammatory diseases (PID), tuberculosis (TB), infections, smoking, surgery, some medicines, hormonal problems (thyroid, prolactin) or excessive stress.
- Unknown causes- Despite thorough investigations, 25-30% causes of infertility remain unknown. This is called “Unexplained Infertility”. The reason may be mere chance factors or there may be some causes which, still medical science has yet to discover. But this should be kept in mind while treating infertility. That means, even with correction of the possible factors (like improving sperm counts or thyroid problems etc) or with proper treatment (IUI, IVF or ICSI), unfortunately the treatment can fail and the exact reason, why the treatment failed, is sometimes difficult to find out.
In general, what are the treatment options for infertility?
To start with, please remember there is no hard and fast rules for infertility treatment. Often medical science fails to understand why couples with very severe form of infertility conceive sooner than those who are having all tests normal. That means, whatever treatment is offered, it’s very important to continue regular sexual intercourse, as the chance of natural pregnancy is usually there in almost all couples. Your doctor will present the facts to you, without pressurizing you on a particular option. After coming to know all pros and cons of different treatment options, you can take decision. Do not hurry. It’s quite natural that you might be in stress.
In general, after the initial tests, a few periods of natural trying is allowed. After that, ovulation induction (giving medicines to release eggs from the ovaries) is offered, failing which IUI and finally IVF is offered. What will be the preferred treatment for you, will depend on your age, duration of marriage, male and female factors and of course, your age. For example, a woman with both tubes blocked or a male with very low sperm count, IVF would be the first line of treatment.
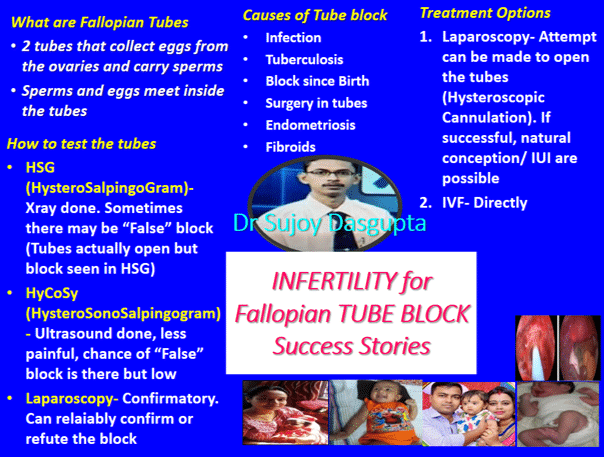
What is Fallopian Tube(s)?
Fallopian tubes (commonly called “the tubes”) are the structures that are connected to the both sides of the uterus, as mentioned above. Each tube is of 10 cm length. The part attached to the uterus is called the “cornu” and the part remaining free is called the “fimbria”. It’s the fimbria, that is present near the ovary and picks up the ovum and transports it inside the tube. The cornu received the sperms from the uterus and passes it inside. Inside the tube, the sperms and the egg meet to form the embryo, which then travels down the tubes into the uterus and then the pregnancy starts.
What happens if tubes are blocked?
If both the tubes are blocked completely, anywhere along the length (cornu, fimbria or the middle), pregnancy is not possible. This is quite obvious, because either the sperm cannot enter or the egg is not picked up or they cannot meet.
However, if any of the tubes are partially blocked, then the sperms and egg can pass and meet but the embryo cannot come down into the uterus. As a result, the pregnancy continues inside the tube, which is called “Ectopic pregnancy” that is life-threatening for the mother. It’s important to remember that ectopic pregnancy can happen even if both the tubes are open.
What are the reasons for tubal blockage?
Often, the exact cause is not known. Infection is the commonest cause. The infections may be due to sexually transmitted infection (STI), particularly Chlamydia infection or infection from bowel or appendix. Tuberculosis is very common in our country and can affect the tubes, silently, without affecting any other parts (not even the lungs) of the body. Endometriosis is also a common reason for tubal blockage. Any pelvic surgery (surgery in ovaries, tubes, uterus, even appendix) can block the tubes by “adhesion”. This means the tube may be open but attached to the bowel or rotated on itself, so that the tube cannot pick up the eggs from the ovaries. Sometimes fibroid of uterus can compress the tube and cause blockage. Women, with previous history of ectopic pregnancy, are at risk. Uncommonly, some abnormalities, present since birth can block the tubes.
What are the types of tubal blockage?
Tubal block may be one sided or both sided. It may involve only a particular part of a tube or multiple parts of a tube. The site of the block may be the cornu, the fimbria or the middle portion.
Hydrosalpinx, is a thing that you must know. In this condition, the tube is blocked but the mid-portion is dilated and contains some fluid (often infected). This tube is not functional. And the problem is even if there is pregnancy by IVF inside the uterus, this fluid from the tube may trickle down, coming in contact with the embryo and can potentially kill the embryo!
How can I understand that the tubes are blocked?
Unfortunately, very few women have signs or symptoms indicating tubal block. However, if you had previous infections in pelvis, tuberculosis in any part of the body, appendicectomy or other gynaecological surgery, there is chance of tubal block. Patients with fibroid and endometriosis are also at risk of tubal block. If you feel severe pain during periods or during intercourse, there is a chance that the tubes may be blocked.
When the tubes should be tested?
As mentioned earlier, the routine investigation of infertility includes testing for the ‘open-ness’ of the tubes- “Tubal patency tests”. That means if pregnancy does not come within 12 months of regular intercourse, then we usually advise the tests. Sometimes, tests are needed, after 6 months of trying (see above). However, in some women, with low risk of tubal block (no risk factors as mentioned above), it may be appropriate to start treatment and continue it for few cycles and if no response, then tubes should be tested.
How the tubes are tested?
The method of tubal patency test depends on your risk of having blocked tubes and also your wishes, availability of resources, other fertility factors and of course the affordability.
Routine ultrasound (like TVS) cannot detect tubal patency. However, it can detect the hydrosalpinx in most of the cases.
If you do not have any risk factors (like pain during periods, endometriosis, previous infections or surgery), you can choose either HSG or SIS. These are done in out-door basis, without any need of anesthesia.
HSG (Hystero-salingogram) is a method by which, your tubes will be seen under Xray. After visualizing your cervix (mouth of the uterus) by a speculum (instrument inserted in the vagina) a small screw will be inserted inside the cervix and a contrast material (which can be seen by the X ray) will be given through it. If tubes are open, the Xray will show that the contrast material will be going through the tubes into the abdomen.
The advantage of HSG is that, a test showing open tube has good correlation with tubal patency (if HSG shows the tubes are open, it’s likely that tubes are open). It is widely available and also cheaper.
However, the problem is that most of the women feel it painful, although they are given pain-killers for it. In addition, there is small risk of infection, for which antibiotics are prescribed. The contrast material can rarely give rise to allergy in some sensitive women and it may be life-threatening in very rare cases. Another problem is the false positive result. That means if tubes are found to be blocked in HSG, in 50% cases, they will be found to be open subsequently in laparoscopy. This is mainly because of some spasm of the muscles of the tube during the test.
SIS (Saline infusion sonography) or HyCoSy (Hystero-Contrast-Sonography) is the method by which tubal patency is checked by ultrasound (TVS) along with water like material inserted inside the uterus through a small tube. If tubes are open, the passage of water can be seen going into the abdomen through the tubes, in the ultrasound.
The advantage of HyCoSy is that it’s much less painful than HSG, although mild discomfort may be there. Pain-killers and antibiotics are prescribed usually. Additionally, problems inside the uterus can be better visualized, even better than normal TVS. In addition, the false positive result is much lower, only 7%. That means if HyCoSy suggests that the tubes are blocked, in most cases, the tubes will be found to be blocked at laparoscopy.
The problem with HyCoSy is mainly the cost and it’s not available everywhere.
An important merit of doing the tubal test is that, sometimes the water or the contrast material used in these tests can open the “mild” block. That’s why we often find patients who conceive spontaneously with pregnancy inside the uterus, after apparently “blocked” tubes in HSG or HyCoSy.
Now, laparoscopy is reserved for those, who are at high risk of tubal block. This includes women with risk factors (pain, surgery, infection etc) o women having “blocked” tube in HSG or HyCoSy. Clearly, it’s done after hospitalization under general anaesthesia inside the OT. Two or three small opening (key-hole surgery) will be put inside the abdomen and through vagina a coloured material (“dye”) will be given inside the uterus. If the tubes are open, the laparoscopic camera will show that dyes coming out of the tubes inside the abdomen.
The advantage is that it’s a definitive test, can help you to make final decision. It also provides the options of treatment. If there is corneal block in HSG, we can make attempt to open the tubes using laparoscopy (see below). In addition, if there is hydrosalpinx, where the tube serves no function, the tubes can be removed (salpingectomy) or clipped (we put clips to block the tubes) to improve the chance of pregnancy if IVF is the only option left for you. In addition, laparoscopy helps us to see whether there is any other diseases that have been missed by routine tests and that may account for infertility. We can treat the cysts of PCOS (by applying current to destroy some cysts), remove any large cysts, remove any adhesion, treat endometriosis etc.
The disadvantage of laparoscopy is of course, the need of anaesthesia and associated surgical and anaesthetic risks, although in modern era, the serious complications are uncommon.
What are my options if tubes are found to be blocked in HSG?
There are simply two options. It depends on your age, fertility factors and affordability. Number one is directly, you can go for IVF. In that case, you can save time and cost. It may be a preferred option, if you are aged or have some other fertility factors (low sperm count, endometriosis etc). The chance of pregnancy per cycle of IVF is usually 40%.
Another option is that you can confirm the block by other tests, keeping in mind that you may need IVF if the tubes are found blocked ultimately. We usually advise to have laparoscopy. However, some women want to give a trial with HyCoSy, because if HyCoSy shows the tubes are open, then you can avoid laparoscopy and you can try different fertility treatment options.
In laparoscopy, first we see if tubes are open or not. If open, there is no need of further treatment in laparoscopy. However, if tubes are found blocked, especially if the block is in cornu, we can try “hysteroscopic tubal cannulation”, where we put a small catheter through hysteroscope (a telescope, like endoscope, put inside the uterus through vagina so that we can see inside the uterus using a camera) to open the tubes. If tubes can be opened, you have all options for fertility treatment open. However, if we fail to open the tubes, the only option left is IVF. In addition, if there is fimbrial block, it can be released and new opening in the fimbria can be made. The treatment of hydrosalpinx by laparoscopy has already been discussed (see above).
Having said that, there are some group of women, who conceive while waiting for IVF or laparoscopy after a blocked tube found in HSG.
What can I do if tubes are blocked in HyCoSy?
In this case also, there is choice between the two- laparoscopy first and IVF directly.
What can I do if laparoscopy suggests tubal block?
Unfortunately, in that case, the only option left is IVF. As mentioned before, if hydrosalpinx is found it must be treated before IVF. However, sometimes we find hydrosalpinx in laparoscopy but cannot cut the tube of clip it, simply because you did not give consent to us for doing so. In that case, we can suck out (“aspirate”) the fluid from the hydrosalpinx under ultrasound guidance (no need of further laparoscopy) using the needle.
How tubal block is dealt in your particular centre by Dr Sujoy Dasgupta?
We believe in patient’s autonomy. So we want to give time on discussion and presentation of facts and figures to the couples. We encourage questions from the couples and take utmost care so that no question remains unanswered.
We do not take decisions and impose it on the couples. We advise the couples to take time before taking decision on a particular treatment. If the couple decides, we respect and support their decision.
We prefer to have SIS or HyCoSy, rather than HSG, to reduce the pain to the women. We discuss all the options if tubes are found blocked.
Conclusion
Tubal factor can account for 20-25% cases of female infertility. It’s more common in secondary infertility (women who conceived earlier- whatever be the fate of the pregnancy). Tubal test is a part of infertility investigation. The choice between HSG and HyCoCy is open to you. If tubes are found blocked, the options are IVF directly or confirming the block by laparoscopy.


+1.svg)
