Chondromalacia Patella: Causes, Symptoms, Treatment and Cost
Last Updated: Feb 25, 2023
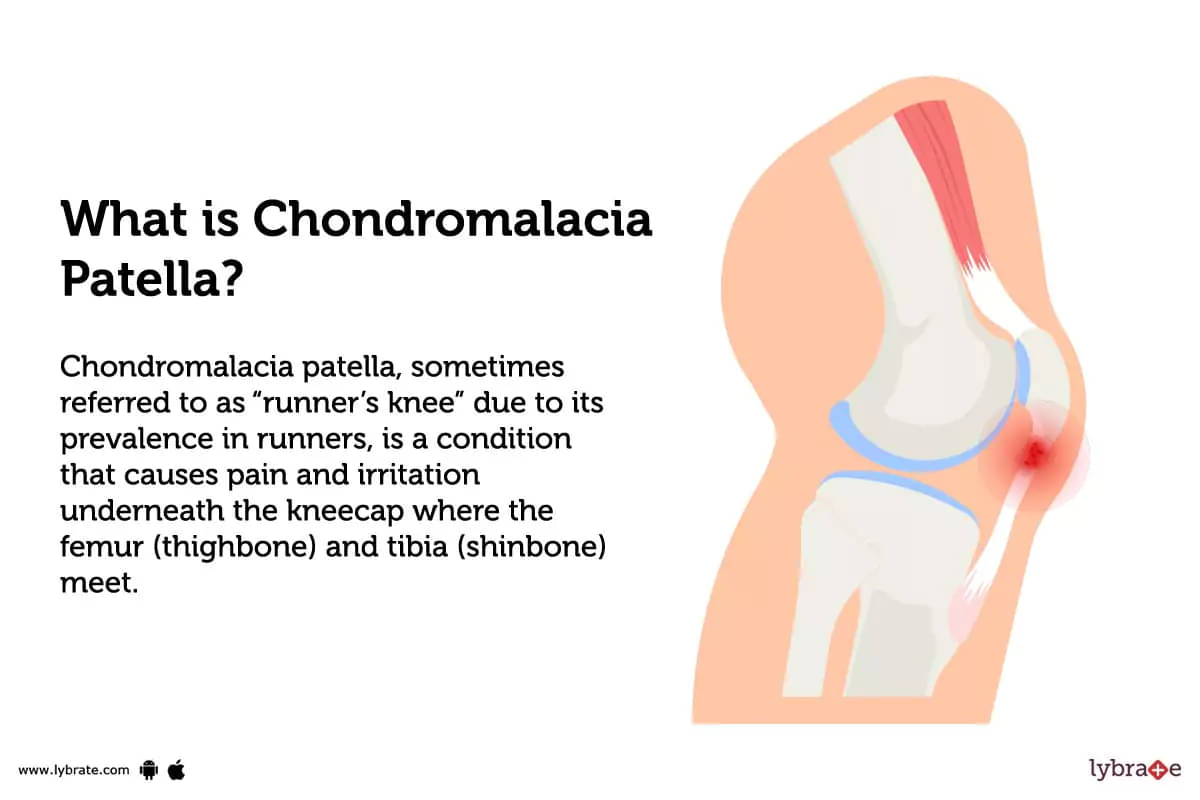
What is Chondromalacia Patella?
Chondromalacia patella, sometimes referred to as 'runner’s knee' due to its prevalence in runners, is a condition that causes pain and irritation underneath the kneecap where the femur (thighbone) and tibia (shinbone) meet. It is caused by softening or weakening of the cartilage at the back of the kneecap and is usually due to repetitive movement or trauma.
Types of Chondromalacia Patella
There are three types of chondromalacia patella:
- Grade I Chondromalacia Patella: This is considered to be the mildest form of the condition. Symptoms may include mild pain or discomfort in the kneecap when bending or running. It usually resolves without treatment in most cases.
- Grade II Chondromalacia Patella: This is a more severe form of the condition that may require treatment such as physical therapy, bracing, or surgery depending on a patient’s individual case. Symptoms may include increased pain with activity, visible swelling of the knee joint, and difficulty straightening the leg completely due to knee cap misalignment (called patellofemoral maltracking).
- Grade III Chondromalacia Patella: This is considered to be advanced chondromalacia patella and requires specialised treatment options such as corrective surgery to resolve symptoms including severe pain with activity and impaired mobility due to instability caused by misaligned kneecap positioning (patellar dislocation).
What causes Chondromalacia Patella?
- Chondromalacia Patella is primarily caused by a misalignment of the patella (kneecap) as it moves up and down the knee joint while walking, running etc.
- Weak Quadriceps muscles, meaning not correctly engaging the thigh muscles when walking can contribute to causing Chondromalacia patella.
- Tight or imbalanced hamstring or iliotibial band muscles can contribute to creating abnormal levels of stress on the patella and cause pain or inflammation in the kneecap joint area.
- Excess weight gain, structural abnormalities in leg like a knock-kneed alignment (where one leg appears to be bowed out from other) have also been linked as possible causes for chondromalacia patella.
What are the symptoms of Chondromalacia Patella?
- Kneecap pain, particularly while bending the knee or climbing stairs.
- Swelling and tenderness of knee joint.
- Popping and grinding sensation on the moving knee joint.
- Muscle weakness in the region that is impacted.
- Trouble climbing stairs or standing for lengthy periods.
How can you prevent Chondromalacia Patella?
- Strengthen quadriceps: Pressure on the kneecap may be relieved by strengthening the quadriceps muscles, which run down the front of the thigh.
- Stretch your hamstrings and ITB: Stretching tight hamstrings, hip flexors, and the iliotibial band can also help reduce tension on the knee joint and its structures.
- Replace high-impact activities: Movements like running, jumping and lunging can worsen chondromalacia patella due to higher forces created at the knee joint. Substitute them with low impact activities like swimming or cycling.
- Improve posture: Maintaining good posture throughout daily activities can help reduce stress placed on your knees and other joints throughout your body by keeping them in a neutral alignment.
- Incorporate foam rolling: Foam rolling or massage over tight or painful areas near or around your knee can also be beneficial in limiting pain associated with chondromalacia patella symptoms.
Chondromalacia Patella - Diagnosis and Tests
- Physical examination: The range of motion and condition of your knees will be evaluated during the physical examination by your doctor. He or she may also palpate (feel) the joint for tenderness, pain and swelling as well as look for other signs such as crepitus (a crunching or grinding sound/feeling), effusion (fluid accumulation) and certain ligament tests.
- X-ray: X-rays can be used to diagnose chondromalacia patella, as the condition causes changes in the alignment and shape of the kneecap that are visible on an X-ray. X-rays can also rule out other potential causes of knee pain or discomfort such as a fracture or arthritis.
- MRI: MRI of the knee is typically used to diagnose CMP, as it can detect changes in the cartilage and soft tissue structures that can be caused by the condition. MRI images of CMP usually show evidence of cartilage degeneration, including fraying and softening of the cartilage around the underside of the kneecap.
- Ultrasound: Ultrasound can be used to diagnose chondromalacia patella by looking at the integrity of the cartilage underneath the kneecap. The ultrasound will show areas of fraying or thinning of the cartilage, which can indicate that chondromalacia patella is present.
What are possible complications of Chondromalacia Patella?
- Pain and swelling under or around the knee joint.
- Loss of full range of motion and difficulty bending the knee.
- Difficulty walking, running or climbing stairs.
- Limited ability to participate in activities.
- Muscle wasting in the legs leading to instability.
- Patella Femoral Syndrome: A condition of constant pain in the knee joint due to misalignment or overuse.
- Osteoarthritis: The wearing down of cartilage around the kneecap.
Home Remedies for Chondromalacia Patella?
- Massage the affected area gently with warm sesame oil or Mahanarayan oil.
- Use a poultice of moist heat to the knee containing analgesic and anti-inflammatory herbs such as Ginger, Turmeric, Guggul and Shunthi powder.
- Consume 1 teaspoon of triphala churna mix with lukewarm water once daily before bedtime for 4-6 weeks to reduce inflammation and stiffness.
- Drink a cup of warm cow's milk mixed with a pinch of carom seeds, Jaggery and a pinch each of Cardamom, Cinnamon and Black Pepper powders for relief from pain & inflammation in the joint.
What to eat in Chondromalacia Patella?
- Maintain a diet rich in fruits and vegetables, lean proteins, healthy grains, and dairy items low in fat by adhering to a healthy eating plan.
- In order to minimise inflammation, you should increase your consumption of foods rich in omega-3 fatty acids, such as salmon and flaxseed oil.
- Choose foods rich in vitamin C and bioflavonoids for cartilage protection and repair.
- Reduce decreased levels of Vitamin D with Vitamin D rich foods like milk, egg yolks and salmons.
What not to eat in Chondromalacia Patella?
- Foods high in fat, sugar and sodium such as cakes, cookies, fried foods and processed meats.
- Energy drinks and other caffeinated liquids.
- High-calorie foods such as ice cream, cheese and processed snacks.
- Refined grains, including white bread and spaghetti.
- Foods high in oxalates like spinach, rhubarb and chocolate.
Chondromalacia Patella Treatment
- Physical Therapy: A physical therapist may provide strength and flexibility exercises to help reduce pain and enhance joint function.
- Medication: Prescription medications such as non-steroidal anti-inflammatory drugs (NSAIDs) may be taken to manage pain and inflammation. In some cases, doctors may suggest injections or surgery if symptoms are severe and do not respond to conservative treatments.
- Bracing: A patellar tendon or kneecap strap can provide support and reduce the pressure placed on your kneecap while you move your leg.
- Arthroscopic Debridement: A minimally invasive surgical procedure in which the tissues around and underneath the kneecap are trimmed to reduce pain, while preserving healthy tissue.
- Osteotomy: Involves cutting and realigning the femur or tibia bones to relieve knee pressure that can be causing pain from chondromalacia patella.
- Lateral Release Surgery: Removes part of the iliotibial band tissue and releases the tightness that can cause friction on the back of your kneecap, resulting in chondromalacia patella pain.
- Patellar Realignment Surgery: During this procedure, a plastic surgeon will manipulate and reshape ligaments on either side of your kneecap along with realigning it to decrease pressure from other joints and reduce pain from chondromalacia patella.
Which doctor to consult for Chondromalacia Patella?
To treat or diagnose chondromalacia patella, consulting an Orthopaedic doctor is recommended as they are specialised in providing treatment for bones and joints related problems.
Which are the best medicines for Chondromalacia Patella?
- Non-steroidal anti-inflammatory drugs (NSAIDs): The most typically given NSAIDs for chondromalacia patella are ibuprofen, aspirin, and naproxen. These medications work by reducing inflammation and pain in the affected joints.
- Corticosteroids: These medications can be taken in tablet form or injected directly into the knee joint to reduce inflammation, swelling, and pain caused by chondromalacia patella.
- Hyaluronic Acid Injections: Hyaluronic acid injections are often used to treat joint pain associated with chondromalacia patella. This treatment works by restoring the natural cushioning that your body provides between joints and cartilage in order to reduce joint pain and improve mobility in affected areas.
How long does it take to recover from Chondromalacia Patella?
Recovery time can vary depending on the severity of the condition, but typically it takes three to six months to regain strength and mobility after implementing a physical therapy program. After this period, further improvements may be made with additional treatment or exercises if necessary.
Are the results of the treatment permanent?
No, the effects of chondromalacia patella treatment are not permanent. Over time, these treatments can help reduce symptoms and allow individuals to continue participating in activities that can impact their overall quality of life. However, it is important to note that treatment does not cure chondromalacia patella and does not provide a permanent solution.
What are post-treatment guidelines?
- Immediately after the treatment, rest is recommended with the leg elevated to reduce swelling and pain. Crutches may be used to avoid putting weight on the affected knee.
- A physical therapist can provide instructions for exercises to strengthen the muscles around the knee joint such as leg extensions and hamstring curls to improve range of motion.
- An exercise program might include stretching and proprioceptive activities (such as balance exercise) for tissue healing and scar tissue mobilisation.
- Wearing a compression sleeve or stockings until swelling has decreased helps reduce pain and support circulation in the area after surgery.
- Ice or warm water therapy may also aid in reducing swelling and pain sensations.
- During recovery, it is important to avoid activities that load excessive force onto your patella, such as running or heavy lifting, until cleared by a doctor.
What is the cost of Chondromalacia Patella treatments in India?
The cost of treatments for Chondromalacia Patella in India can vary depending on the treatment required and the severity of the condition. Generally, conservative treatments such as physical therapy exercises, strengthening exercises, and braces may cost around ₹2,000 to ₹3,000.
Whereas more severe cases require surgery which could cost anywhere between ₹15,000 to ₹50,000 or more. In addition to this, other associated costs such as hospital stay charges must also be considered.
What are side-effects of Chondromalacia Patella treatments?
- Common side effects from treatments of Chondromalacia Patella include knee pain, stiffness and limited mobility.
- Other possible side-effects can occur when non-steroid anti-inflammatory drugs (NSAIDs) or corticosteroids are used for treatment, such as stomach discomfort, bleeding or ulcers, kidney problems and decreased immunity.
- Surgery for some cases of Chondromalacia Patella can bring about additional risks such as infection, blood clots and injuries to the nerve or artery near the kneecap.
Chondromalacia Patella - Outlook/ Prognosis
If you experience chondromalacia patella symptoms, you should see a doctor as soon as possible because they can cause complications such as 'difficulty walking, patella femoral syndrome, osteoarthritis' and the treatment course can range from a few months to years according to the severity of the situation.
Table of content
15+ Years of Surgical Experience
All Insurances Accepted
EMI Facility Available at 0% Rate
Find Orthopedic Doctor near me
Ask a free question
Get FREE multiple opinions from Doctors