Diaphragm (Human Anatomy): Image, Function, Diseases, And Treatments
Last Updated: Mar 17, 2023
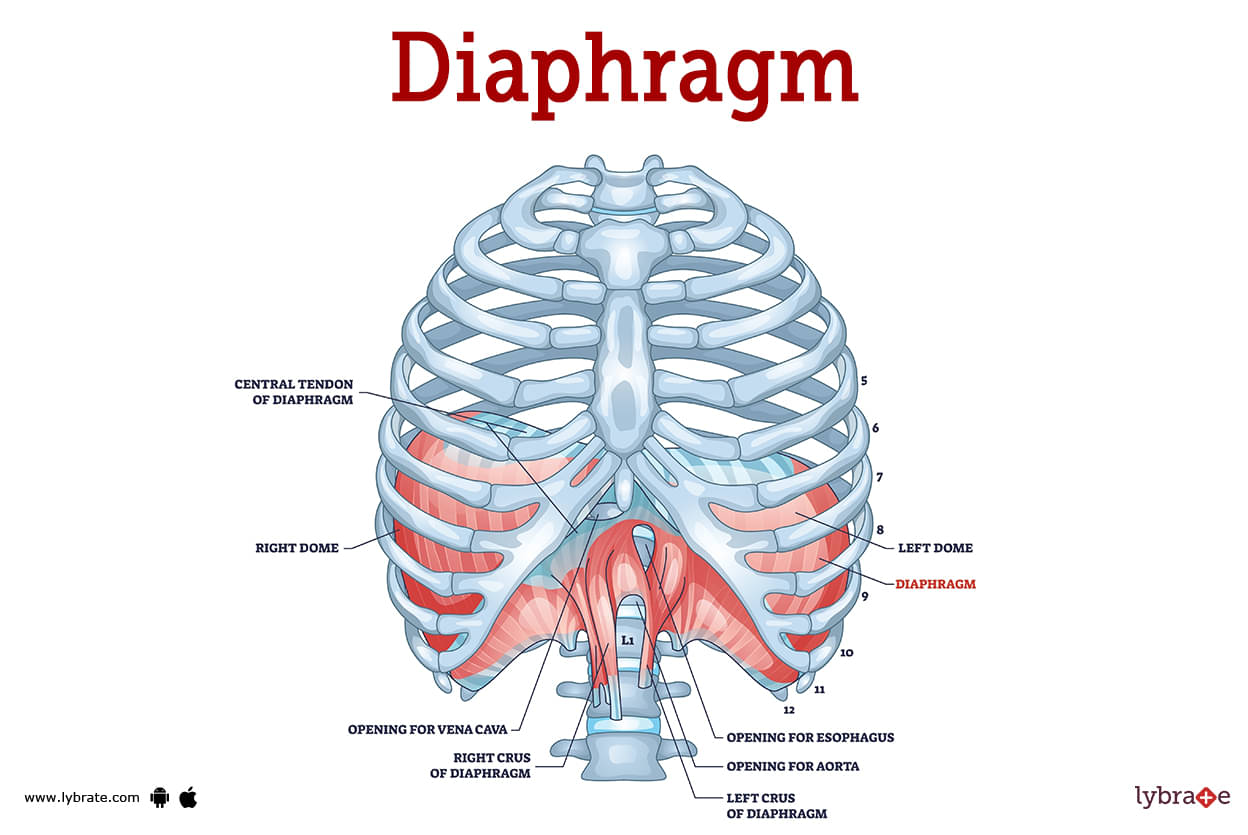
Diaphragm Image
The diaphragm is one of the most essential muscles in our body that is involved in breathing. It is a huge, dome-shaped structure that is found right behind the lungs, around the lower to middle of the rib cage, and has an upwardly curving, C-shaped appearance when the body is in a normal state.
It may be found near the very bottom of the chest and divides the abdominal cavity from the chest cavity. The action of the diaphragm is governed by the phrenic nerve, which travels from the neck to the organ in question and governs its movement.
Diaphragm Functions
Assisting in the process of breathing is the diaphragm's primary and most significant role. When you inhale, the diaphragm moves downward, assisting the expansion of the lungs, and allowing air to enter the lungs.
Exhalation causes the diaphragm to move back up. When we exhale, the diaphragm returns to its starting position, so completing the cycle of respiration that began when we breathed in.
It does this by increasing abdominal pressure, which in turn assists the body in expelling waste products such as vomit, urine, and faeces. In addition to this, it exerts pressure on the oesophagus in order to stop acid reflux.
Diaphragm Conditions
- Hiatal Hernia: A hiatal hernia occurs when the uppermost portion of the stomach protrudes beyond the diaphragm's esophageal aperture. Although the cause of this is unknown, it might be caused by congenital abnormalities, ageing related changes in the diaphragm injury, or persistent coughing-related strain on nearby muscles.
- Diaphragmatic Hernia: When at least one organ from the abdomen protrudes into the chest via a hole in the diaphragm, this condition is known as a diaphragmatic hernia. Symptoms like difficulty breathing, tachypnea, blue discoloration of the skin, tachycardia, diminished or absent breath sounds and bowel sounds in the chest area can be seen.
- Congenital Diaphragmatic Hernia: A hole in the diaphragm, the thin muscular sheet separating the chest from the belly, causes CDH. The colon, stomach, or even the liver may travel into the chest cavity when this opening develops during a foetus's growth in the womb. These abdominal organs' presence in the chest reduces the amount of room for the lungs and may cause respiratory issues.
- Acquired Diaphragmatic Hernia: A hernia of the diaphragm may also be caused by trauma sustained in an accident or during surgery. In this particular instance, the condition is known as acquired diaphragmatic hernia (ADH). It is possible to see symptoms such as trouble breathing, quick breathing, high heart rate, skin that is blue in colour, and the sound of bowel movements in the chest.
- Diaphragmatic Cramp: Diaphragmatic spasm is another name for it, and it may induce symptoms like chest discomfort and shortness of breath that are similar to those of a heart attack. In addition to this, some individuals may suffer perspiration, anxiousness, and a sense that they are unable to fully exhale during a spasm. The diaphragm does not lift back up once an exhale occurs during a spasm. This causes the lungs to expand, which tightens the diaphragm. This might therefore result in chest cramps as well. Exercise that is strenuous may cause the diaphragm to spasm, which often causes what is known as a side stitch.
- Diaphragmatic Flutter: This is an uncommon ailment that's sometimes misdiagnosed as a spasm. An individual may experience the fluttering as a pulsating feeling in the abdomen wall during an episode. In such circumstances, symptoms including stomach discomfort, chest pain, shortness of breath, and tightness in the chest may be present.
- Phrenic Nerve Damage: Damage to the phrenic nerve may result from trauma, surgery, cancer of the lungs or lymph nodes nearby, problems of the spinal cord, autoimmune diseases, neuromuscular disorders, such as multiple sclerosis, and certain viral infections, which can further result in diaphragm dysfunction or paralysis.
- Hiccups: The diaphragm may frequently contract involuntarily when it is inflamed, such as while eating or drinking fast. When the diaphragm contracts and air is expelled at the same moment, hiccups sound. Hiccups often go away on their own, but there are remedies for instances that continue.
- COPD: Diaphragm weakening may result from lung diseases, particularly Chronic Obstructive Pulmonary Disease (COPD). This occurs as a result of an ongoing process that has many contributing elements. Hyperinflated lungs brought on by COPD exert physical pressure on the diaphragm. The whole muscle flattens, and its mobility is reduced. The diaphragm's cells gradually change over time as a result of extreme tension, which impairs their capacity to perform at their peak. These cells suffer damage from chronic oxygen deprivation brought on by COPD.
- Cancer: Tumours may physically push on the diaphragm and impair its capacity to function by spreading to the organ or by occupying space in the chest or abdominal cavity. Mesothelioma, a cancer of the pleura, the outer lining of the lungs, lung cancer, lymphoma, and stomach cancer are among the several cancers that may affect the diaphragm. Shortness of breath, breathing-related discomfort, and loss of consciousness are just a few of the symptoms that might be present.
- Diaphragmatic Palsy: A number of systemic disorders may cause inflammation of the phrenic nerve or the diaphragm, which results in this condition. Diaphragmatic weakness has been connected to bacterial infections like Lyme disease, viral infections including HIV, West Nile virus, and poliomyelitis virus, noninfectious causes like sarcoidosis, and amyloidosis.
- Diaphragmatic Eventration: Where muscle has been replaced by fibroelastic tissue, the diaphragm may thin down partially or completely. breathing problems, particularly after activity or while laying down, coughing, chest discomfort, repeated pneumonias, and cardiac arrhythmias are a few symptoms.
- Diaphram Paralysis: The loss of control of one or both sides of the diaphragm is known as diaphragm paralysis. Lung capacity is reduced as a result. Shortness of breath, headaches, bluish lips and fingers, weariness, sleeplessness, and general trouble breathing are all possible signs of diaphragm paralysis.
- Chilaiditi's Sign: In older people, this accidental discovery of a section of the colon positioned between the liver and diaphragm often occurs without any symptoms or as an asymptomatic condition. This clinical finding is referred to as Chilaiditi's sign when no symptoms are present. Although individual symptoms might vary, frequent bouts of persistent stomach discomfort are a typical finding.
Diaphragm Tests
- Chest X-ray: A chest X-ray may determine whether or not there are blockages or fluids that are causing pressure.
- CT scan: A computed tomography, often known as a CT scan, is a kind of imaging test that combines X-ray and computer technology to create comprehensive cross-sectional pictures of the chest cavity. These images are used to examine the diaphragm for any abnormal signs.
- Magnetic Resonance Imaging: MRI is a technique that uses powerful magnetic rays, a computer, and radio frequencies to generate detailed pictures of organs and other structures in the body. In contrast to CAT scans and X-rays, magnetic resonance imaging (MRI) does not use the utilisation of radiation.
- Ultrasound: It is a method of imaging that may identify any anomalies in the operation of the diaphragm by capturing movement.
- Spirometry: spirometry is a test that estimates the degree to which inflammation and narrowing of the bronchial tubes have occurred by measuring the amount of air and the speed with which a person is able to exhale.
- Peak Flow Meter: A peak flow metre is a device that determines how strongly an individual is able to exhale. Patients' conditions may be monitored remotely using peak flow metres placed in their homes.
- Exercise Oximetry: The sensor for exercise oximetry is clipped onto the patient's finger, and it measures the amount of oxygen that is present in the patient's blood while they are engaging in physical activity.
- Arterial Blood Gas: This kind of blood test evaluates the acidity of the blood in addition to determining the levels of oxygen and carbon dioxide that are present in the arterial blood.
- Phrenic Nerve Stimulation Test: The phrenic nerve stimulation test involves applying electric or magnetic stimulation to the patient's neck in order to evaluate the reaction of the phrenic nerve and, by extension, the diaphragm's capacity to perform its intended role.
- Electromyography: It is often known as an EMG test, is a diagnostic procedure that analyses the electrical potential of muscle fibres after being activated by electrical impulses.
- Fluoroscopy Examination: The fluoroscopy examination is analogous to seeing an X-ray movie in that it involves the observation of moving anatomical components. The area of the patient's body that is being examined is traversed by a continuous X-ray beam. The beam is sent to a monitor that resembles a television, which allows the body part and its movements to be seen in finer detail.
- Sniff Test: The sniff test is a kind of examination that compares the movement of the diaphragm during normal breathing to that which occurs after rapid inhalation. The examination makes use of a fluoroscope, which is a specialised kind of X-ray equipment that provides the expert with real-time views of the patient's inside organs. It demonstrates an elevation of the paralysed hemidiaphragm with inspiration, in contrast to the quick drop of the normal hemidiaphragm during inspiration.
Diaphragm Treatment
- Breathing Pacemaker: The diaphragm is the body's major breathing muscle, and its activity can be regulated by a breathing pacemaker. An inhalation (inspiration) occurs when electrodes are inserted either around the phrenic nerves that supply the diaphragm or into the muscle itself.
- Laparoscopy For Hiatal Hernia: Nissen Fundoplication, a minimally invasive laparoscopic procedure used to treat hiatal hernia and acid reflux, has a high success rate. The surgeon will also make the opening in your diaphragm smaller and may reconstruct an esophageal sphincter to hold the stomach in proper position.
- Open Surgery: The stomach and any surrounding tissue are dragged down from the chest cavity and back into the abdomen during surgery to treat a hiatal hernia, which is often accomplished through small incisions.
- Phrenic Nerve Treatment: Phrenic nerve reconstruction may involve neurolysis, interposition nerve grafting, and/or neurotization, depending on the extent of the injury.
- Chemotherapy: A cancer treatment drug or drug cocktail. Diaphragm-invading tumours (T3 in the staging classification) are thought to be treatable with surgical excision because they have not spread beyond the muscle.
Diaphragm Medicine
- Analgesics for relieving pain in diaphragm: To alleviate the pain and inflammation of the diaphragm, analgesics such as aspirin, ibuprofen, and acetaminophen can be used. Naproxen and paracetamol are two other types of analgesics.
- Antibiotics for infection of the diaphragm and lower respiratory tract: If the doctor determines that an infection is the major cause of the patient's discomfort, antibacterial medicine will most likely be administered to treat the problem. The most prevalent antibiotics are amoxicillin, ampicillin, and penicillin.
- Muscle relaxants for diaphragm pain: A patient may be given muscle relaxants like metaxalone, methocarbamol, orphenadrine, or carisoprodol by a professional who is treating them for their condition.
- Mucopurulent drugs for respiratory tract infection: This combination drug can treat infections that cause a cough as well as a runny or stuffy nose (nosal congestion). Mucolytic medications, such as guaifenesin, can help to reduce mucus viscosity, resulting in better mucus clearance. Another medication that may induce mucopurulent side effects is pseudoephedrine. It relieves hay fever symptoms as well as other allergens that impact the respiratory tract.
Frequently Asked Questions (FAQs)
Can you live without a diaphragm?
Is the diaphragm an organ?
Can diaphragm be cured?
Can you repair a damaged diaphragm?
How can I improve my diaphragm health?
What are the symptoms of diaphragm problems?
What is the treatment for diaphragm?
- Top Cardiothoracic Vascular Surgeon in Delhi
- Top Cardiothoracic Vascular Surgeon in Mumbai
- Top Cardiothoracic Vascular Surgeon in Gurgaon
- Top Cardiothoracic Vascular Surgeon in Pune
- Top Cardiothoracic Vascular Surgeon in Kolkata
- Top Cardiothoracic Vascular Surgeon in Bangalore
- Top Cardiothoracic Vascular Surgeon in Chennai
- Top Cardiothoracic Vascular Surgeon in Hyderabad
Table of content
Find Cardiothoracic Vascular Surgery near me
Ask a free question
Get FREE multiple opinions from Doctors