Get the App
For Doctors
Login/Sign-up
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
High-Risk Pregnancy Care Tips
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
What is high-risk pregnancy?
High risk pregnancy is a pregnancy that carries an increased chance of complications and adverse outcomes for the mother, baby, or both.
Factors that can increase the risk of a high-risk pregnancy include advanced maternal age, obesity, pre-existing medical conditions (such as diabetes or hypertension), multiple foetuses, smoking, and prior history of preterm labour.
Types of high risk pregnancy:
Multiple gestat...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Multi Speciality•Gorakhpur
Pregnancy is one of the most delicate phases in the life of a woman and if she is experiencing a high-risk pregnancy then she needs to be extra cautious. It is an extra delicate phase for her and she should watch herself very minutely. She must take good care of herself and if she feels or notices any discomfort, then she must immediately consult her gynecologist. But what exactly is a high-risk pregnancy?
A high-risk pregnancy is one where the expecting mother or her fetus or both are ...more
A high-risk pregnancy is one where the expecting mother or her fetus or both are ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Pregnancy is one of the most delicate phases in the life of a woman and if she is experiencing a high-risk pregnancy then she needs to be extra cautious. It is an extra delicate phase for her and she should watch herself very minutely. She must take good care of herself and if she feels or notices any discomfort, then she must immediately consult her gynecologist. But what exactly is a high-risk pregnancy?
A high-risk pregnancy is one where the expecting mother or her fetus or both are ...more
A high-risk pregnancy is one where the expecting mother or her fetus or both are ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
If you want to have a safe pregnancy by curtailing all sorts of complications, then you have to promptly respond to warning bells. There are certain warning symptoms that should not be neglected at all as that might put your pregnancy in danger.
Bleeding
This kind of situation cannot be ignored as that often leads to serious issues like placental abruption or miscarriage. In this case, you are definitely in need of the assistance of an expert midwife.
Swollen face or hands...more
Bleeding
This kind of situation cannot be ignored as that often leads to serious issues like placental abruption or miscarriage. In this case, you are definitely in need of the assistance of an expert midwife.
Swollen face or hands...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Miscarriage is termed as the loss of the fetus in or before 20th week of pregnancy. Medically, miscarriage is known as spontaneous abortion though the word spontaneous is more of a keyword as it is not an abortion.
Symptoms of Miscarriage
Miscarriage happens due to weakness, back pain, fever, abdominal pain along with severe cramps and bleeding which starts from slow to heavy.
Cause of Miscarriage
Common cause of miscarriage is when the fetus is known to have...more
Symptoms of Miscarriage
Miscarriage happens due to weakness, back pain, fever, abdominal pain along with severe cramps and bleeding which starts from slow to heavy.
Cause of Miscarriage
Common cause of miscarriage is when the fetus is known to have...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
Travelling during pregnancy - Is it safe?
Pregnancy places some restrictions on the expectant mother, and one of them is limiting travel so much so that most women do only the required and essential commutes and skip any other travel, including vacations and business travel, completely until delivery. However, with the lifestyle changing for the woman so radically, this is being revisited. The doctor s current advice is that unless there are potential complications expected or significant co...more
Pregnancy places some restrictions on the expectant mother, and one of them is limiting travel so much so that most women do only the required and essential commutes and skip any other travel, including vacations and business travel, completely until delivery. However, with the lifestyle changing for the woman so radically, this is being revisited. The doctor s current advice is that unless there are potential complications expected or significant co...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
The complications and dangers associated with pregnancy often increase manifold in the case of a high-risk pregnancy. Extra medical attention is required for those mothers who are going through a high-risk pregnancy.
In order to avoid any complication which threatens your or your child s life, you have to be extra careful about the food you eat as well as the daily activities you do. Not taking care of yourself can put you and your child s health in danger. Given below are a few tips to...more
In order to avoid any complication which threatens your or your child s life, you have to be extra careful about the food you eat as well as the daily activities you do. Not taking care of yourself can put you and your child s health in danger. Given below are a few tips to...more
Last Updated: 8 years ago• Featured Tip
Share
Bookmark
Report
Travelling during pregnancy - Is it safe?
Pregnancy places some restrictions on the expectant mother, and one of them is limiting travel so much so that most women do only the required and essential commutes and skip any other travel, including vacations and business travel, completely until delivery. However, with the lifestyle changing for the woman so radically, this is being revisited. The doctor s current advice is that unless there are potential complications expected or significant co...more
Pregnancy places some restrictions on the expectant mother, and one of them is limiting travel so much so that most women do only the required and essential commutes and skip any other travel, including vacations and business travel, completely until delivery. However, with the lifestyle changing for the woman so radically, this is being revisited. The doctor s current advice is that unless there are potential complications expected or significant co...more
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
Certainly! here are 100 words summarizing the tips for pregnant women:
1. Regular prenatal care is vital for a healthy pregnancy.
2. Maintain a balanced diet with nutritious foods.
3. Stay hydrated by drinking plenty of water.
4. Engage in safe and moderate exercise.
5. Get enough rest and prioritize sleep.
6. Manage stress through relaxation techniques.
7. Educate yourself about pregnancy and childbirth.
8. Avoid harmful substances like alcohol and tobacco.<...more
1. Regular prenatal care is vital for a healthy pregnancy.
2. Maintain a balanced diet with nutritious foods.
3. Stay hydrated by drinking plenty of water.
4. Engage in safe and moderate exercise.
5. Get enough rest and prioritize sleep.
6. Manage stress through relaxation techniques.
7. Educate yourself about pregnancy and childbirth.
8. Avoid harmful substances like alcohol and tobacco.<...more
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
Pregnancy is a natural process that occurs when a sperm fertilizes an egg. While it is a beautiful experience for some, it can be an unwanted outcome for others. There are several ways to avoid pregnancy after sex naturally, which can be effective when followed correctly.
;
There are a variety of natural foods and supplements that are believed to have contraceptive properties. Here are 11 examples:
Papaya: papaya contains enz...more
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
What is high-risk pregnancy?
High risk pregnancy is a pregnancy that carries an increased chance of complications and adverse outcomes for the mother, baby, or both.
Factors that can increase the risk of a high-risk pregnancy include advanced maternal age, obesity, pre-existing medical conditions (such as diabetes or hypertension), multiple foetuses, smoking, and prior history of preterm labour.
Types of high risk pregnancy:
Multiple gestat...more
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
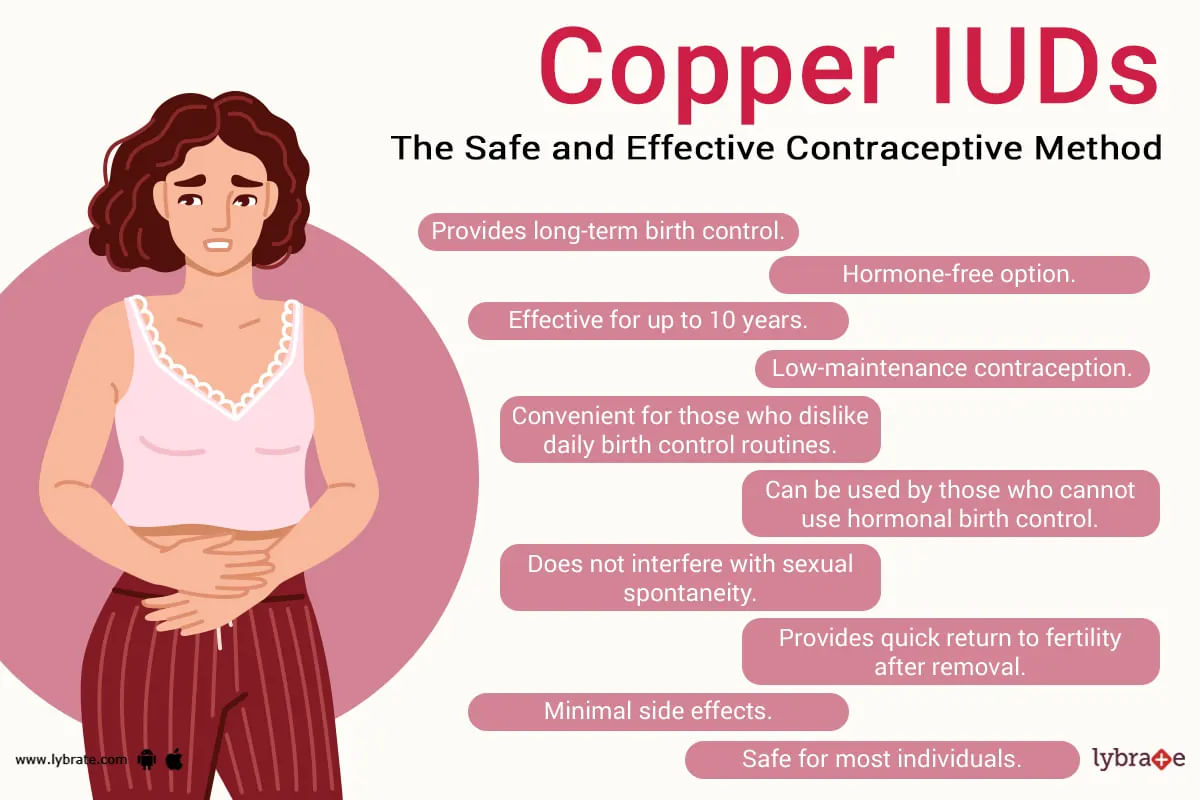
Paragard is a long-term contraceptive option that doesn't rely on hormones to be effective. In other words, it can be defined as an intrauterine device (iud), which is predominantly meant to provide long-term contraception (or birth control) without the use of hormones. It's a t-shaped device that is small in size, is inserted into the uterus of a woman, and can stay there for up to 10 years to prevent an unwanted pregnancy during all this time.
The paragard device i...more
505 people found this helpful
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
गर्भावस्था के दौरान हार्मोन्स में बदलाव के कारण गर्भवती के शरीर में बहुत सारे परिवर्तन होते हैं। स्तनों में परिवर्तन भी गर्भावस्था का एक सामान्य हिस्सा है। गर्भाधान के 1 सप्ताह बाद से ही स्तनों में परिवर्तन हो सकते हैं।
स्तनों में होने वाले परिवर्तन बच्चे के जन्म और उसके बाद तक जारी रह सकते हैं। आज हम आपको बताएंगे कि गर्भावस्था की प्रत्येक तिमाही के दौरान स्तनों में सबसे आम परिवर्तन क्या होते हैं।
यह समझना महत्वपूर्ण है कि स्तन परिवर्तन हर महिला में भिन्न प्रकार के होते हैं और ...more
स्तनों में होने वाले परिवर्तन बच्चे के जन्म और उसके बाद तक जारी रह सकते हैं। आज हम आपको बताएंगे कि गर्भावस्था की प्रत्येक तिमाही के दौरान स्तनों में सबसे आम परिवर्तन क्या होते हैं।
यह समझना महत्वपूर्ण है कि स्तन परिवर्तन हर महिला में भिन्न प्रकार के होते हैं और ...more
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
कई महिलायें संभोग सुख का आनंद तो लेना चाहती हैं लेकिन गर्भ धारण नहीं करना चाहती। ऐसी महिलाओं के लिए निरोध और गर्भ निरोधक गोली जैसे कई विकल्प होते हैं। ऐसा ही एक विकल्प है कॉपर आईयूडी, जो एक गर्भ निरोधक के रूप में कार्य करता है। यह कई महिलाओं द्वारा इस्तेमाल भी किया जाता है, क्योंकि यह पूरी तरह से सुरक्षित माना जाता है।
तो चलिए जानते हैं कि यह कॉपर आईयूडी (पैरागार्ड) क्या है और किस तरह से काम करता है। इसके साथ ही इसके फायदों और दुष्प्रभाव पर भी चर्चा करते हैं
क्या होता है कॉपर आ...more
तो चलिए जानते हैं कि यह कॉपर आईयूडी (पैरागार्ड) क्या है और किस तरह से काम करता है। इसके साथ ही इसके फायदों और दुष्प्रभाव पर भी चर्चा करते हैं
क्या होता है कॉपर आ...more
49 people found this helpful
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
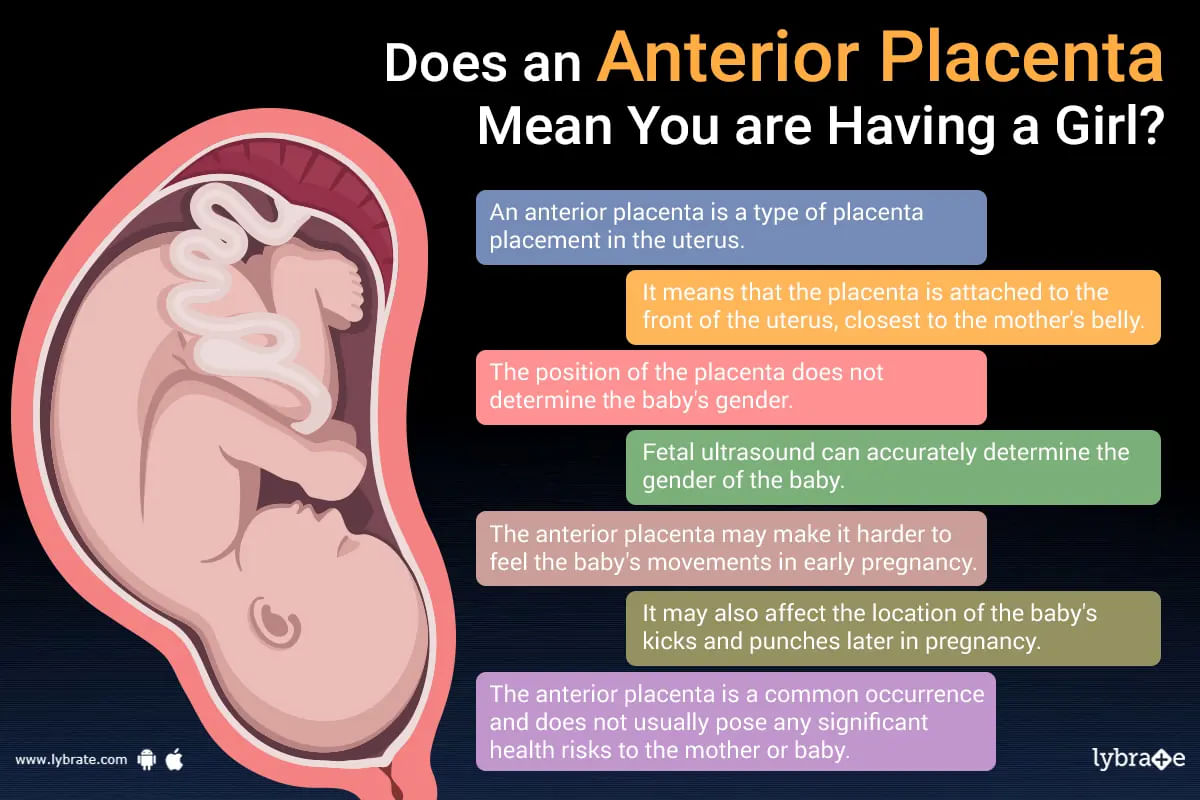
What does the term anterior placenta mean?
There are two types of cells that make up an embryo: those that develop into the baby and those that develop into the placenta. The placenta can be best defined as a pancake-shaped organ that develops in a woman's uterus when she is pregnant. It serves as a barrier between the mother and the developing fetus, providing nutrients and oxygen to the fetus and removing waste products from its blood.
It must be noted t...more
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
The pain in the abdomen during pregnancy is common. But sometimes, these pain may also lead to some serious problems. There can be various reasons for the pain in the abdomen during the pregnancy. The causes of the pain in the abdomen can be due to the pain in the lower back, pain in the ligaments, vaginal discharge, bleeding, cramping, trapped wind, cramps of the vagina, bleeding etc. The other serious causes of the pain in the abdomen can be due to some serious conditions s...more
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
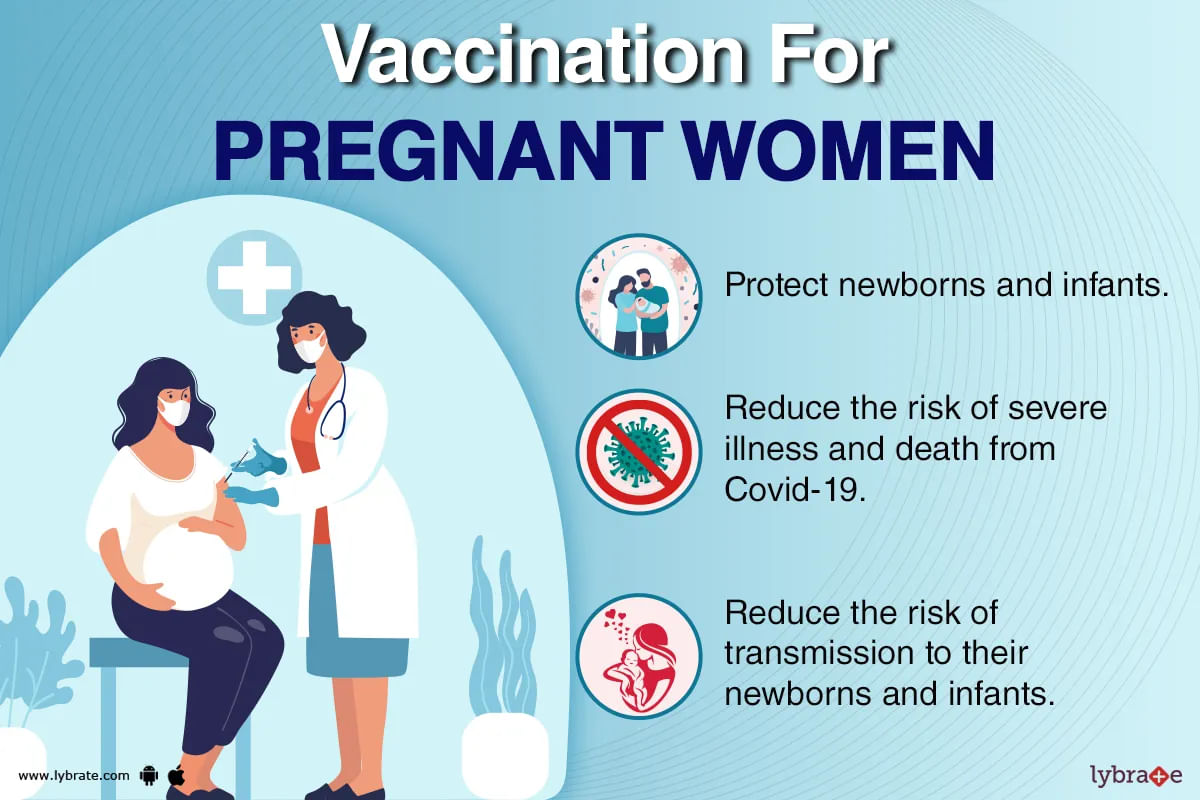
The covid-19 pandemic has affected the entire world, with the virus spreading rapidly and causing significant illness and death. In order to combat the spread of the virus, vaccines have been developed and are now being distributed globally. While the vaccines have proven to be effective at reducing the risk of severe illness and death from covid-19, many people have questions about their safety and potential side effects. Whether the covid vaccine can have an impact on subsequent preg...more
241 people found this helpful
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
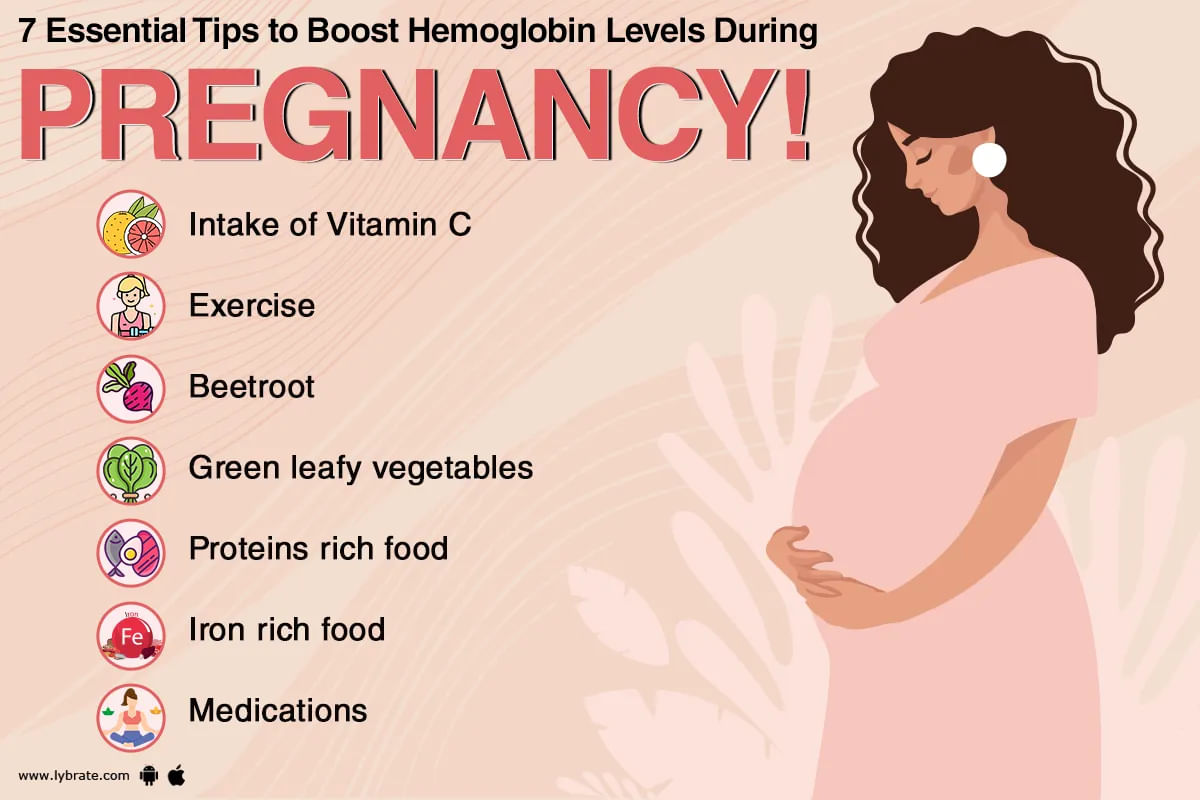
Hemoglobin is a type of protein that is found in the red blood cells of the body. It is the protein that is rich in iron. The function of hemoglobin is to transport the oxygen to the tissues and to the organs of the body. Hemoglobin carries the oxygen from the respiratory organs of the body to the tissues. The level of hemoglobin during the pregnancy should be 11.5-13.0 g/dl. When the level of hemoglobin in the pregnant woman falls below 10.0 g/dl, then it is not at all good ...more
Book appointment with top doctors for High-Risk Pregnancy Care treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously