Get the App
For Doctors
Login/Sign-up
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Breast Discharge Tips
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Breast pain, lumps in the breast or discharge from the nipples are some of the more common complaints seen in women. Also, it is generally observed that such women are between the ages of 40-69. While most of these cases are benign, the diagnosis or the problem should be deciphered only after a detailed analysis of the case, symptoms, and history of breast cancer if any.
Breast Pain: Breast pain can arise from a condition called mastitis. It is generally seen in new mothers where the ba...more
Breast Pain: Breast pain can arise from a condition called mastitis. It is generally seen in new mothers where the ba...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Nipple discharge is a common part of breast functioning, which normally occurs during breast-feeding or pregnancy. It is often associated with the changes of menstrual hormone. The milky discharge post breast-feeding usually continues for up to two years after stopping nursing. The condition normally gets resolved on its own but if the situation persists for a long time resort to medical assistance.
The following are some of the causes of normal nipple discharge:
Stimulation: N...more
The following are some of the causes of normal nipple discharge:
Stimulation: N...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
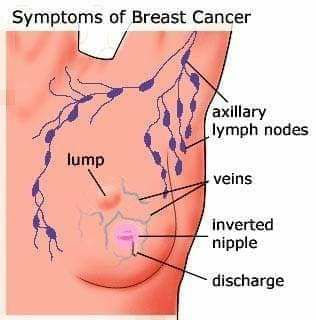
With the modernization of all economies around the world, one health hazard that has become one of the largest perils within both developed and developing nations is the incidence of cancers of the female reproductive system, especially cervical and breast cancer.
Breast cancer
Breast cancer is the formation of malignant tumors within the breast tissues of a woman. Usually, breast cancer affects women in the age range of 40 to 50, but there have been many reports of it occurrin...more
Breast cancer
Breast cancer is the formation of malignant tumors within the breast tissues of a woman. Usually, breast cancer affects women in the age range of 40 to 50, but there have been many reports of it occurrin...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Breast cancer is a disease in which malignant (cancer) cells form in the tissues of the breast. It occurs in both women and men, although breast cancer in men is rare.
Risk factors:
Lack of physical activity
Alcohol consumption
Advancing age
No childbirth or no breastfeeding
Family history of breast cancer
Early menarche (< 12 years of age) or late menopause ( > 55 years of age)
History of ovarian cancer or endometrial cancer
History of benign breast...more
Risk factors:
Lack of physical activity
Alcohol consumption
Advancing age
No childbirth or no breastfeeding
Family history of breast cancer
Early menarche (< 12 years of age) or late menopause ( > 55 years of age)
History of ovarian cancer or endometrial cancer
History of benign breast...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
Homoeopathic remedies for Breast lump.
Most lumps are not cancer, A breast lump is a growth of tissue that develops within your breast. Different types of breast lumps can vary in the way they look and feel. You may perceive a lump as a mass, growth, swelling, thickness or fullness.
You might notice:
a distinct lump with definite borders
a firm, hard area within your breast
a thickened, slightly more prominent area in your breast that's different from surroun...more
Most lumps are not cancer, A breast lump is a growth of tissue that develops within your breast. Different types of breast lumps can vary in the way they look and feel. You may perceive a lump as a mass, growth, swelling, thickness or fullness.
You might notice:
a distinct lump with definite borders
a firm, hard area within your breast
a thickened, slightly more prominent area in your breast that's different from surroun...more
Last Updated: 8 years ago• Featured Tip
Share
Bookmark
Report
Breast cancer is a malignant tumor (a collection of cancer cells) arising from the cells of the breast. Although breast cancer predominantly occurs in women, it can also effect men.
After skin cancer, breast cancer is the most common cancer diagnosed in women. Breast cancer can occur in both men and women, but it's far more common in women.
Substantial support for breast cancer awareness and research funding has helped improve the screening and diagnosis and advances in th...more
After skin cancer, breast cancer is the most common cancer diagnosed in women. Breast cancer can occur in both men and women, but it's far more common in women.
Substantial support for breast cancer awareness and research funding has helped improve the screening and diagnosis and advances in th...more
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
गर्भावस्था शुरू होने के साथ ही महिलाओं के शरीर में कई तरह के परिवर्तन होने शुरू हो जाते हैं जो बच्चे के जन्म के बाद तक जारी रहते हैं। इस दौरान महिलाओं को कई तरह की समस्याओं का सामना करना पड़ता है। ऐसी ही एक समस्या है ब्रेस्ट इंगोर्जमेंट, जिसका सामना महिलाओं को बच्चे के जन्म के बाद करना पड़ता है। तो चलिए आज हम महिलाओं की इस समस्या पर विस्तार के चर्चा करते हैं। साथ ही इसके होने के कारण और बचाव के बारे में भी बताएंगे। इसके इसके पहले यह जान लेने हैं कि ब्रेस्ट इंगोर्जमेंट है क्या।
क्या है ब्र...more
क्या है ब्र...more
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
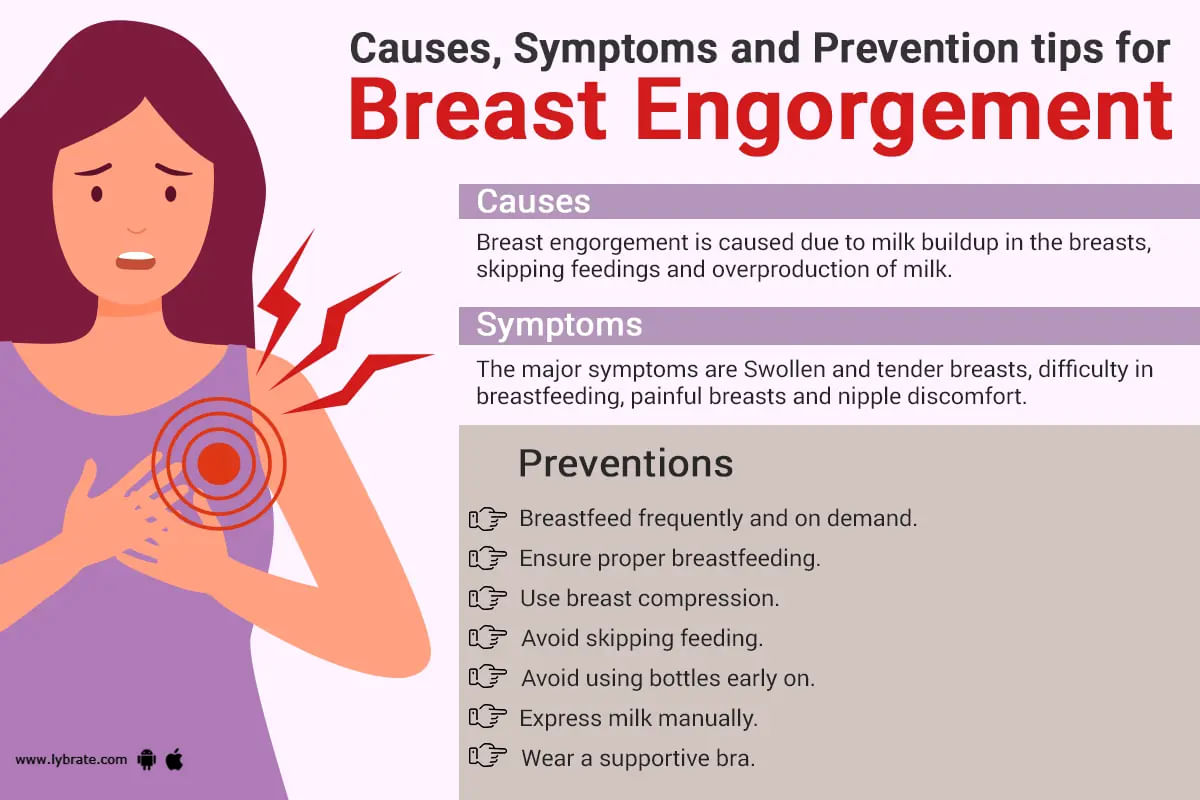
Breast engorgement is a common yet painful condition among breastfeeding mothers, characterized by swollen, hard and tender breasts due to an excessive amount of milk. ;
It can occur at any point during breastfeeding, and if left untreated, can lead to various complications such as clogged ducts and infections. In this article, we will delve into the causes, symptoms, and effective ways of managing and preventing breast engorgement.
The milk rush:...more
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
Ayurvedic Doctor•Sri Ganganagar
There is one universal golden rule when it comes to having amazing sex: the wetter, the better! this logic should make you think about lube (or lubricant), because it's essentially just there to make things wetter. And who doesn't like that?
It must be noted that lube is not just for the times when things are feeling a bit dry down there. In fact, it can actually make sex better for everyone involved by creating less friction and leaving your skin feeling smoother af...more
245 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
As a pregnant woman, maintaining good hygiene is crucial for the health and well-being of both you and your baby. Taking care of your intimate area is an important part of this. From increased vaginal discharge to the risk of infections, pregnancy can bring about many changes to your body. That's why we've put together this guide on how to clean your private parts during pregnancy. Follow these tips to keep your intimate area clean, healthy, and comfortable throughout your pr...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Gynaecologist•Mumbai
Heavy bleeding or menorrhagia is a condition that is characterized by an abnormally heavy or prolonged bleeding that requires a woman to change her sanitary pads every one to two hours during her menstruation cycle. Due to the condition a woman can lose a lot of blood in the form of huge blood clots, resulting in anemia, fatigue, weakness, breathlessness, mood swing and other health problems if continued for a longer period of time. ;
Menorrhagia can be a ...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
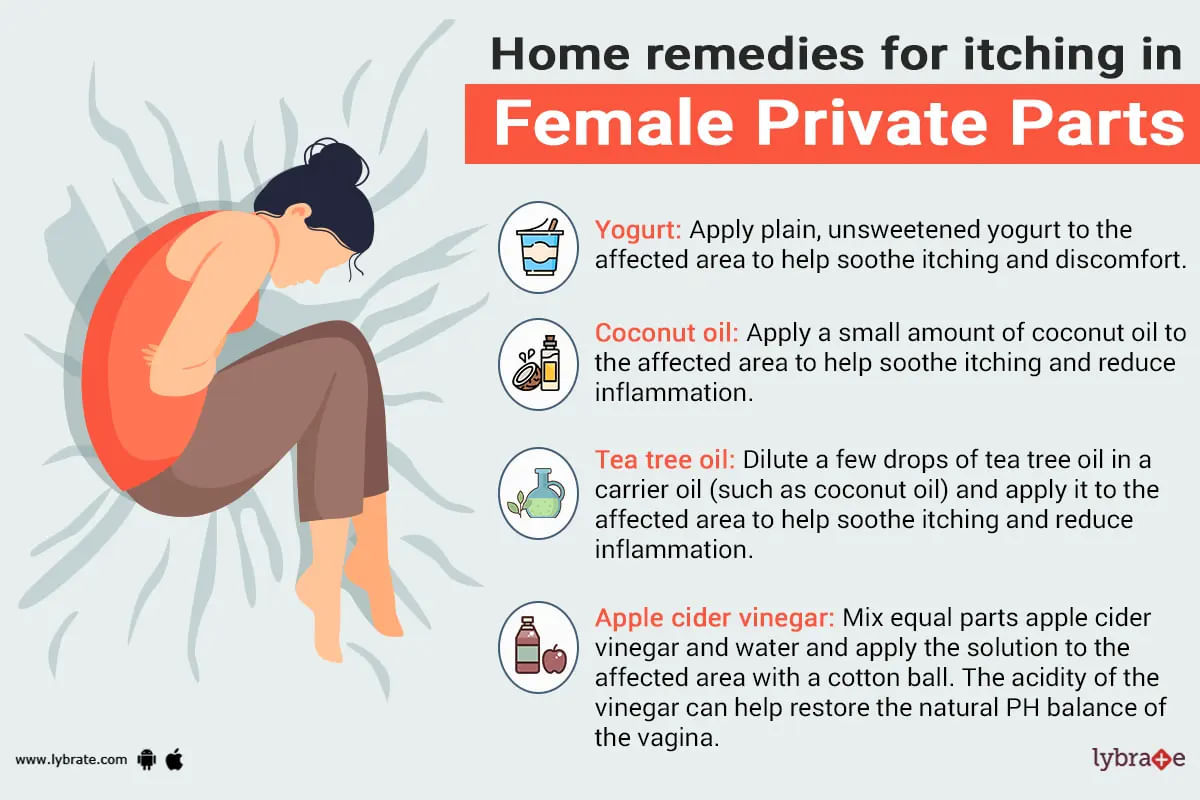
The itching in the private parts of females is an irritation that makes them feel uncomfortable. Itching in the private parts of the female is the symbol of the infection in the vagina, yeast infection, itching in the vulvar areas of the female. Mostly women feel the itching in the private parts during the menstrual cycle or during the menopausal transition due to some of the fluctuations in the estrogen level. They should visit the doctor immediately if they are having the genital red...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
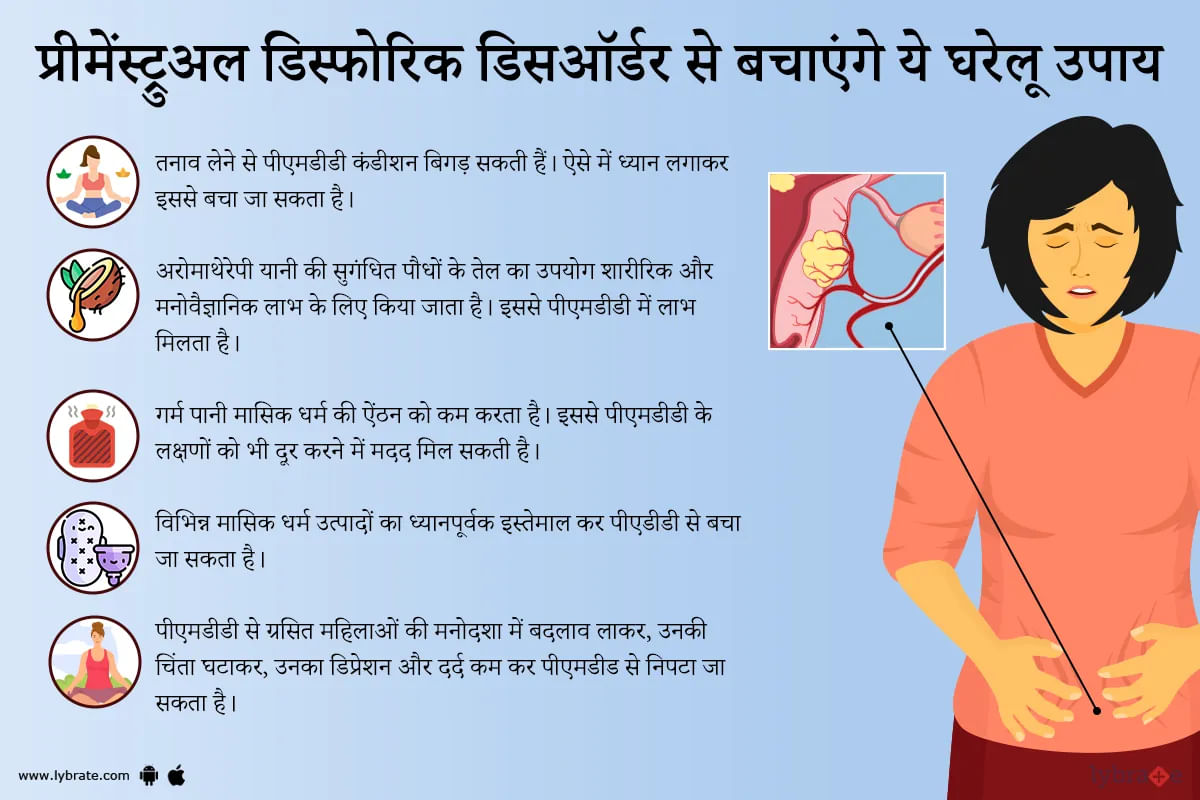
पीएमडीडी का मतलब है प्री मेनस्यूरल डायसफोरिक डिआर्डर। प्रीमेंस्ट्रुअल डिस्फोरिक डिसऑर्डर एक प्रकार का प्रीमेंस्ट्रुअल सिंड्रोम है। यह चिड़चिड़ापन, चिंता और थकान का कारण बनता है। एक अनुमान के अनुसार, करीब 3 से 8 प्रतिशत महिलाओं में प्रीमेंस्ट्रुअल डिस्फोरिक डिसऑर्डर (पीएमडीडी) होता है।
हालाँकि, वास्तविक संख्या अधिक हो सकती है। पीएमडीडी में प्रीमेंस्ट्रुअल सिंड्रोम (पीएमएस) के समान कई लक्षण हैं, लेकिन वे बहुत अधिक तीव्र होते हैं और कुछ लोगों के लिए रोजमर्रा की जिंदगी में काम करना मुश्कि...more
हालाँकि, वास्तविक संख्या अधिक हो सकती है। पीएमडीडी में प्रीमेंस्ट्रुअल सिंड्रोम (पीएमएस) के समान कई लक्षण हैं, लेकिन वे बहुत अधिक तीव्र होते हैं और कुछ लोगों के लिए रोजमर्रा की जिंदगी में काम करना मुश्कि...more
1451 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
To have a healthy vagina a woman needs to maintain a certain level of ph in the vagina. There are so many factors which can play a key role in the maintenance of the ph level and the factors can be either environmental or natural; these factors could lead a woman to experience various problems like burning, itching and change in the discharge from the vagina.
;
There are certain steps which you can follow to keep your vaginal ph level balanced and to do thi...more
453 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Dermatologist•Patna
Itching is also known as pruritus. It is a condition which causes irritating sensation and is usually uncontrollable that makes us scratch it to have some relief from it.
;
Itchy breast is quite common and usually occurs due to increase in the size of the breast which directly relates to weight gain. It can also be due to some allergies, skin infection or dry skin. Most commonly this itching will resolve on its own or by some home remedies and doesn't require any prescription...more
;
Itchy breast is quite common and usually occurs due to increase in the size of the breast which directly relates to weight gain. It can also be due to some allergies, skin infection or dry skin. Most commonly this itching will resolve on its own or by some home remedies and doesn't require any prescription...more
1344 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Gynaecologist•Hyderabad
Vagina is a part of female's genitals. This starts as an opening which is known as introitus or labia's inner part. A woman s vagina ends at the uterus' opening, known as the cervix.
The health of the vagina of a woman could be regarded as the most important part of her overall health. The vagina affects a lot of activities going on in a female's body and its good condition is responsible for a woman's total body welfare.
;
If there is any sort of problem w...more
The health of the vagina of a woman could be regarded as the most important part of her overall health. The vagina affects a lot of activities going on in a female's body and its good condition is responsible for a woman's total body welfare.
;
If there is any sort of problem w...more
409 people found this helpful
Book appointment with top doctors for Breast Discharge treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously