Get the App
For Doctors
Login/Sign-up
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Post Surgery Rehabilitation Tips
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The word 'surgery' is often dreaded by most patients. Be it an invasive oral surgery or a keyhole gallbladder surgery, it does not evoke a ready "yes" in most patients. There are too many patients who are ready to be on long-term medications if they could avoid the surgery and its complications. While there could be swelling, bruising, tingling, and many other symptoms, the one feared by most is the postoperative pain. What happens after the effect of the anesthetic wears off can leave many pati...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Fellow of Faculty of Pain Medicine (FFPM...read more
Pain Management Specialist•Delhi
Post surgical pain is common after any surgery. It usually abates as one recovers and healing occurs. Pain persisting beyond the period of healing is termed as persisting postsurgical pain or Chronic Postsurgical Pain (CPSP). Generally a period of 3 months is considered adequate for healing and is used when defining CPSP.
Some use up to 6 months period post surgery, prior to labelling the pain as CPSP. To diagnose pain as CPSP:
It should not have been present before surgery or ...more
Some use up to 6 months period post surgery, prior to labelling the pain as CPSP. To diagnose pain as CPSP:
It should not have been present before surgery or ...more
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
Knee replacement surgery, also known as arthroplasty, is a medical procedure that entails replacing a damaged, worn, or diseased knee joint with an artificial joint. This type of surgery is frequently performed to address knee pain caused by arthritis and has become a routine operation.
Tests for Knee Replacement Surgery:
Before undergoing knee replacement surgery, there are several tests that must be conducted to ensure that you are a suitable candidate for the procedure. These tes...more
Tests for Knee Replacement Surgery:
Before undergoing knee replacement surgery, there are several tests that must be conducted to ensure that you are a suitable candidate for the procedure. These tes...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
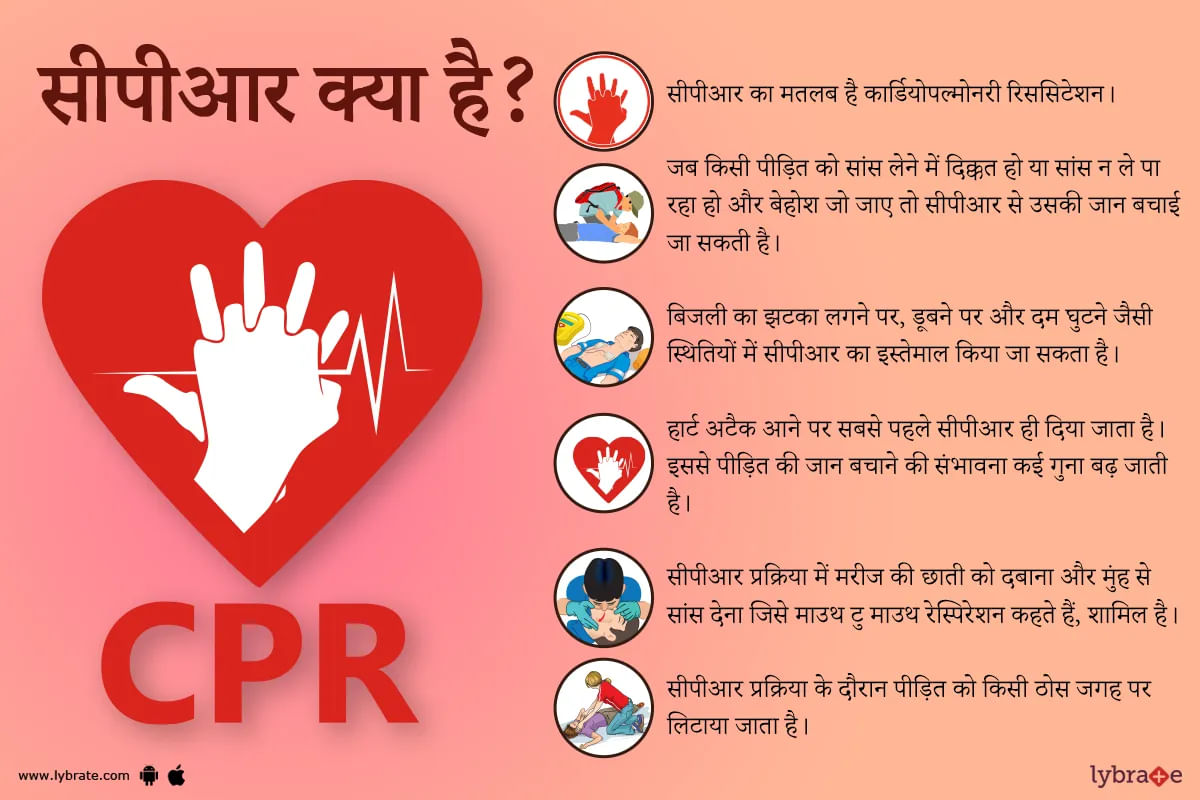
सीपीआर का मतलब है कार्डियोपल्मोनरी रिससिटेशन। यह भी एक तरह की प्राथमिक चिकित्सा यानी फर्स्ट एड है। जब किसी पीड़ित को सांस लेने में दिक्कत हो या फिर वो सांस न ले पा रहा हो और बेहोश जो जाए तो सीपीआर से उसकी जान बचाई जा सकती है। बिजली का झटका लगने पर, पानी में डूबने पर और दम घुटने पर सीपीआर से पीड़ित को आराम पहुंचाया जा सकता है। हार्ट अटैक यानी दिल का दौरा पड़ने पर तो सबसे पहले और समय पर सीपीआर दे दिया जाय तो पीड़ित की जान बचाने की संभावना कई गुना बढ़ जाती है।
अगर किसी...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Orthopedic Doctor•Delhi
1. Dr. Hemant gaur
Https://www. Lybrate. Com/delhi/doctor/dr-hemant-gaur-physiotherapist
Mpt, mphill
11 years experience 200 at clinic 300 online
;
He is a physiotherapist who is well-known for treating people with complicated conditions. He also works as a homecare physiotherapist. He obtained his outstanding education and clinical experience as an mpt at manav rachna international university and as a mphill at opjs university. His...more
309 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
General Surgeon•
1. Dr. Muthuraju k r
Https://www. Lybrate. Com/bangalore/doctor/dr-muthuraju-k-r-general-surgeon
;
Mbbs, ms, gastro-intestinal, bariatric and metabolic surgery
21 years experience 0 at clinic
As an experienced and skilled surgeon, he has assisted a great number of patients and is currently working with vulnerable patients who have suffered from myocardial infarction, systemic hypertension, and illnesses such as arteriosclerosis and oth...more
Https://www. Lybrate. Com/bangalore/doctor/dr-muthuraju-k-r-general-surgeon
;
Mbbs, ms, gastro-intestinal, bariatric and metabolic surgery
21 years experience 0 at clinic
As an experienced and skilled surgeon, he has assisted a great number of patients and is currently working with vulnerable patients who have suffered from myocardial infarction, systemic hypertension, and illnesses such as arteriosclerosis and oth...more
12 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
1. Dr. S d I ranjit
Https://www. Lybrate. Com/bangalore/doctor/dr-s-d-i-ranjit-orthopedist? lpt=ps-srp
Mbbs, dnb-orthopedics/orthopedic surgery
18 years of experience 0 550 at the clinic.
He is a specialist in orthopaedic medicine and works in the medical field as a joint replacement surgeon and an orthopedist hand surgeon. In addition, he is a board-certified paediatric orthopedist, an expert in laser therapy, a skilled arthroscopist and knee replacement surg...more
Https://www. Lybrate. Com/bangalore/doctor/dr-s-d-i-ranjit-orthopedist? lpt=ps-srp
Mbbs, dnb-orthopedics/orthopedic surgery
18 years of experience 0 550 at the clinic.
He is a specialist in orthopaedic medicine and works in the medical field as a joint replacement surgeon and an orthopedist hand surgeon. In addition, he is a board-certified paediatric orthopedist, an expert in laser therapy, a skilled arthroscopist and knee replacement surg...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
1. Dr. Jitender pal singh
Https://www. Lybrate. Com/delhi/doctor/dr-jitender-pal-singh-orthopedist
Mbbs, Ms. - (orthopedics)
12 years of experience, rs. 600 in clinic, rs. 400 online
Dr. Jitendra pal singh is a renowned orthopedist who treats patients suffering from chronic pain, injuries to the hip, ankle, and knee, as well as a number of other disorders. At the moment, he is employed at the bone and joint clinic, which is located in the punjabi bagh neighbou...more
Https://www. Lybrate. Com/delhi/doctor/dr-jitender-pal-singh-orthopedist
Mbbs, Ms. - (orthopedics)
12 years of experience, rs. 600 in clinic, rs. 400 online
Dr. Jitendra pal singh is a renowned orthopedist who treats patients suffering from chronic pain, injuries to the hip, ankle, and knee, as well as a number of other disorders. At the moment, he is employed at the bone and joint clinic, which is located in the punjabi bagh neighbou...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Laparoscopy surgery is a very vital component of the hernia repair. Studies have shown that many patients have a better outcome when they opt for laparoscopic surgery. Candidates eligible for this mode of surgery include those with bilateral inguinal hernias, ventral hernias, and recurrent hernia. People associated with athletics and other outdoor sports prefer to go for a laparoscopic hernia surgery as it ensures a speedy recovery and minimal tissue invasion (due to small incisions).
L...more
L...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Esophagectomy is a procedure of removing a part of the esophagus and reconstructing the same using another organ of the body. The oesophagus is the tube that connects the stomach and the mouth. This procedure is often performed in an advanced stage of esophageal cancer and Barrett s esophagus. This procedure removes the cancer cells from the esophagus and gives relief from the symptoms. The organs from where the reconstructing tissues are taken are generally large intestine and stomach.
more
more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Dialysis is a very important and life-saving procedure. It is performed to replace kidney function in case of renal failure. Wastes and extra fluids in the blood are filtered out during this process. To be able to perform Dialysis, the connection between the patient s bloodstream and the equipment for performing Dialysis (dialyzer) outside the body is established. This connection is created through Dialysis Access Surgery. It is a type of Vascular Surgery which forms the vascular opening for acc...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
You may have reached a ripe age with all the worldly knowledge at your disposal to share with the world. You may have reached a stage where you no longer feel like a learner in important areas of life and could easily be someone who has the experiences and the expertise to help people out in times of their trouble.
However, you may also be at a juncture where your knees in particular may not be your best friends anymore. You may be facing a lot of joint issues and the knees may be a pai...more
However, you may also be at a juncture where your knees in particular may not be your best friends anymore. You may be facing a lot of joint issues and the knees may be a pai...more
Book appointment with top doctors for Post Surgery Rehabilitation treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously