Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Menopause Tips
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Menopause is a very important phase of a women's life but before this transition phase begins there are some events that occur before the onset of the menopause and these events are said to be premenopausal events. These events are an indication that your body has started to produce less amount of estrogen than the required amount. This diminished production of this estrogen hormone leads the women to experience irregularity in their periods, further she will notice that she ...more
615 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
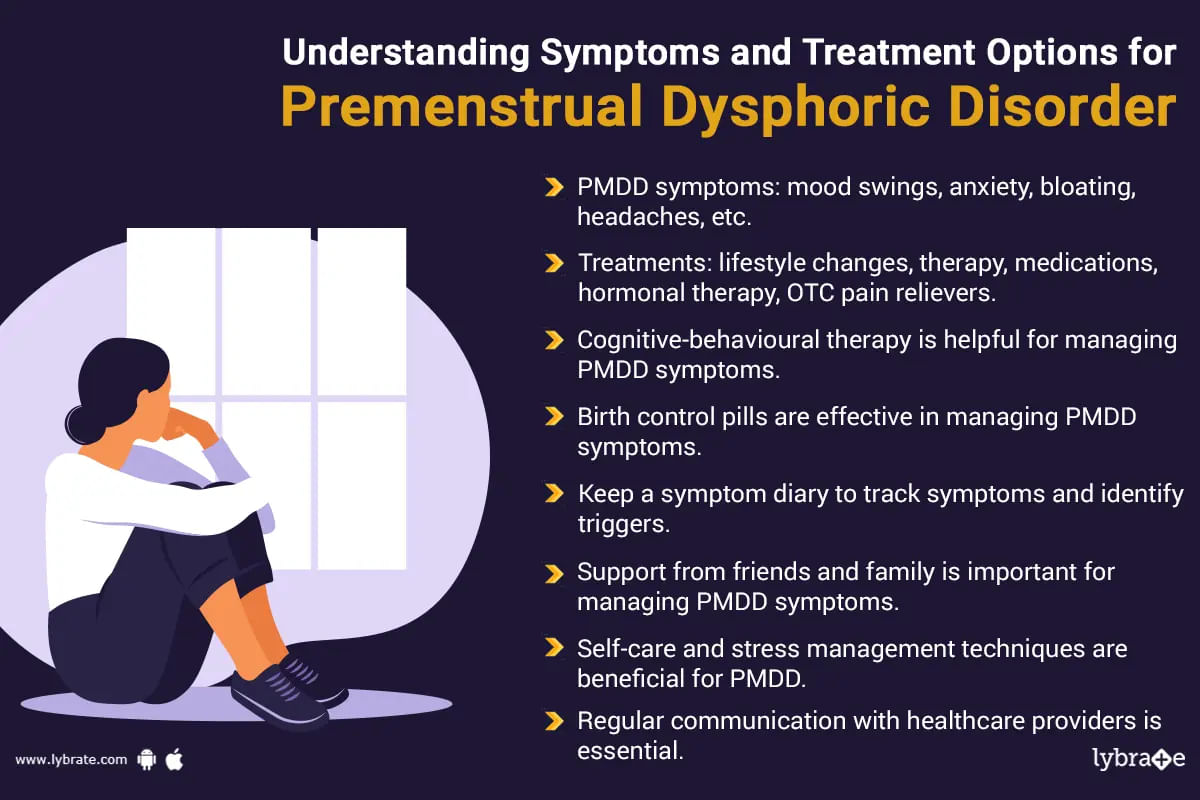
Premenstrual dysphoric disorder (pmdd) is a form of the premenstrual syndrome (pms) which occurs as a result of the disturbance of the level of hormones. Around 2 to 5 percent of the women who are about to experience the condition of menopause. The symptoms of this syndrome is somewhat similar to that of pms which means the woman will suffer from problems like fatigue, food cravings and irritability but in this case the woman will experience these symptoms in an amplified man...more
476 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
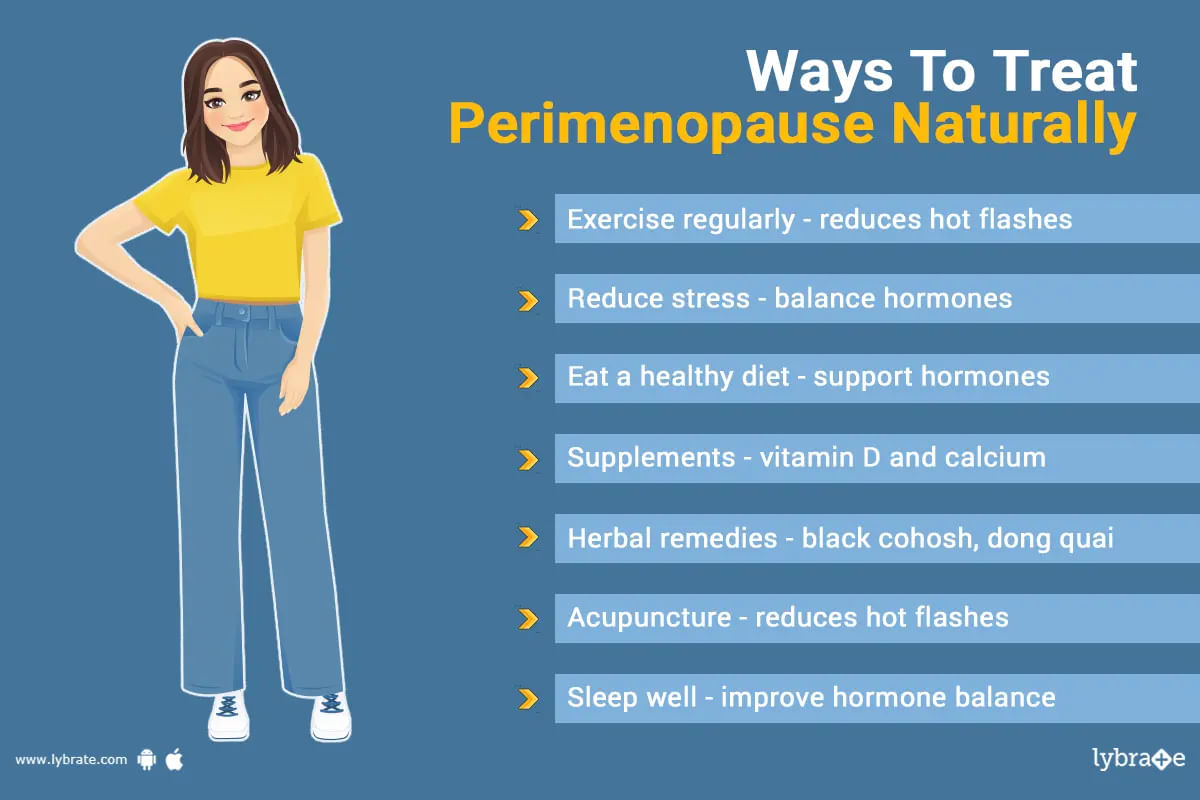
पेरिमेनोपॉज़ वह समय है जो रजोनिवृत्ति यानी मीनोपॉज के पहले से लेकर मीनोपॉज तक का होता है। इस समय के दौरान है कि लोग सबसे पहले लक्षणों का अनुभव करना शुरू करते हैं। ये लक्षण प्रोजेस्टेरोन और एस्ट्रोजन के स्तर में असंतुलन के परिणामस्वरूप होते हैं।
हालांकि हार्मोन रिप्लेसमेंट थेरेपी (एचआरटी) इन लक्षणों का इलाज करने में मदद कर सकती है, पर इस समय के लिए कोई भी महिला प्राकृतिक उपचार भी आजमा सकती है। इस लेख में कुछ प्राकृतिक उपचारों पर चर्चा होगी जो लोगों को पेरिमेनोपॉज़ के लक्षणों को प्राकृत...more
हालांकि हार्मोन रिप्लेसमेंट थेरेपी (एचआरटी) इन लक्षणों का इलाज करने में मदद कर सकती है, पर इस समय के लिए कोई भी महिला प्राकृतिक उपचार भी आजमा सकती है। इस लेख में कुछ प्राकृतिक उपचारों पर चर्चा होगी जो लोगों को पेरिमेनोपॉज़ के लक्षणों को प्राकृत...more
1430 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Menopause is defined as stoppage of woman's menstrual cycles because of age or removal of ovaries or uterus (in few cases). This generally happens between the ages of 45-55 (mostly recorded at the age of 51). This lasts for a few years before the bleeding during the menstruation completely stops. When a woman doesn't have period for a full year (twelve months) then you can say that she has reached her full menopause.
Some women can experience perimenopause first before reaching full me...more
Some women can experience perimenopause first before reaching full me...more
365 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
मीनोपॉज यानी रजोनिवृत्ति किसी भी महिला के जीवन में एक महत्वपूर्ण चरण है। मीनोपॉज उस स्थिति को कहते हैं जब किसी महिला का मासिक चक्र (पीरियड्स) स्थायी रूप से आने बंद हो जाते हैं। यह स्थिति महिलाओं के शरीर में गंभीर हार्मोनल परिवर्तन का कारण बनती है। इस स्थिति में महिला का शरीर एस्ट्रोजन और प्रोजेस्टेरोन जैसे हार्मोन का उत्पादन बंद कर देती हैं। मीनोपॉज या रजोनिवृत्ति आमतौर पर 45 से 55 वर्ष की आयु के बीच होती है, लेकिन वर्तमान जीवनशैली और तनाव के कारण, यह देखा गया है कि महिलाएं 4...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Menopause is the time in your life when you naturally stop having menstrual periods. Menopause happens when the ovaries stop making hormones. Menopause marks the end of the reproductive years. The average age that women go through menopause is 51 years.
The years leading up to menopause are called perimenopause. Cycles may become longer than usual for you or become shorter. You may begin to skip periods. The amount of flow may become lighter or heavier. Although changes in menstrual ble...more
The years leading up to menopause are called perimenopause. Cycles may become longer than usual for you or become shorter. You may begin to skip periods. The amount of flow may become lighter or heavier. Although changes in menstrual ble...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
The menopause can take three very different routes for women. There are those who sail through it with very few symptoms or problems and don't even notice that their ovaries have stopped producing the hormone. Then there are those for whom it is a matter of a few hot flushes and a couple of night sweats, doesn't last long and not really a bother. This usually marks a relief from the periods. But for some, it is abject misery accompanied by crippling fatigue, absolute exhaustion, hot flushes, vag...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
During the natural course of events, a women's body starts its reproductive phase with menarche and at about 50 years of age, attains menopause. This is when the reproductive function ceases and the ovaries stop producing the hormone estrogen and progesterone. In some cases, for various reasons including medical, the ovaries stop functioning earlier, and this is medically termed early or premature menopause. Menopause that occurs before 40 years of age is termed premature menopause; it is due to...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The disruption of the normal female cycles of menstruation and ovulation after the age of 45 and the loss of her ability to conceive naturally is known as menopause. The associated symptoms of menopause are heat flushes, insomnia, weight gain, depression, nausea and fatigue. While hormone replacement therapy is the most common procedure to provide relief from menopausal symptoms, natural homeopathic remedies can also be used for the same. These remedies are completely safe as opposed to hormone ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
There are three stages of menopause: Pre-menopause, Menopause, and Post-menopause. This article discusses the symptoms and care after menopause or post-menopause.
Post-menopause is referred to life after menopause. It is a stage when women have not had periods for more than 12 months. During this stage, the annoying signs and symptoms that women experience before and during menopause may gradually decrease. However, due to the low level of estrogen after menopause, women are at higher r...more
Post-menopause is referred to life after menopause. It is a stage when women have not had periods for more than 12 months. During this stage, the annoying signs and symptoms that women experience before and during menopause may gradually decrease. However, due to the low level of estrogen after menopause, women are at higher r...more
Book appointment with top doctors for Menopause treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously