Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTips
Meckel'S Diverticulum Tips
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
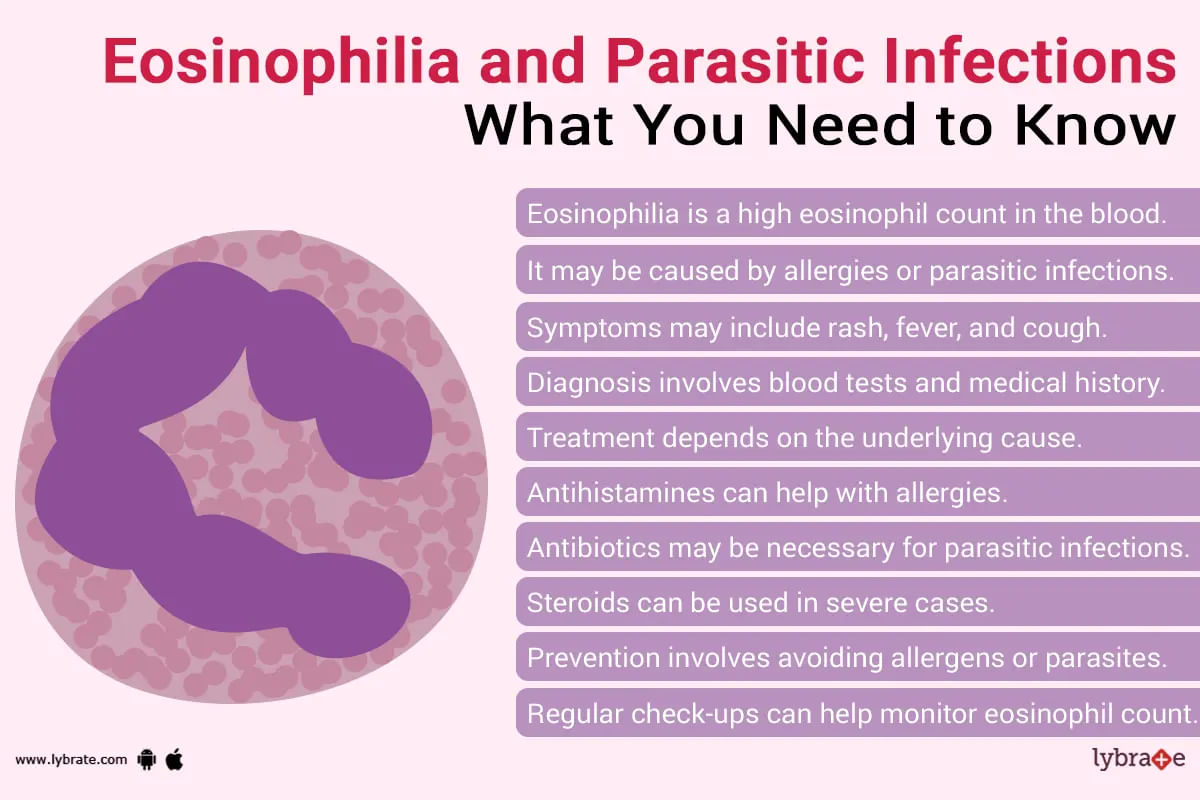
Eosinophilia is when the level of eosinophils is higher than normal level in blood. Eosinophils are a type of WBC (white blood cells). These cells are the immune system of our body which helps to fight diseases. When there is parasitic infection, bacterial infection or any type of allergic reaction, these cells help us to fight it. It is also useful in defeating cancer.
If there is an attack of foreign substance/lives there is an increase at levels of eosinophils in blood or if attack i...more
If there is an attack of foreign substance/lives there is an increase at levels of eosinophils in blood or if attack i...more
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
ईओसिनोफिलिया तब होता है जब आपका शरीर असामान्य रूप से ईओसिनोफिल पैदा करता है। ईओसिनोफिल कई श्वेत रक्त कोशिकाओं में से एक हैं जो आपकी प्रतिरक्षा प्रणाली का सहयोग करती हैं।
कभी-कभी, कुछ चिकित्सीय स्थितियां और दवाएं ईओसिनोफिल के उच्च स्तर का कारण बनती हैं।
ईओसिनोफिलिया क्या है?
ईओसिनोफिल श्वेत रक्त कोशिकाओं में से एक हैं जो आपकी प्रतिरक्षा प्रणाली को सपोर्ट करती हैं। वे एलर्जी के खिलाफ आपके शरीर की रक्षा प्रणाली का हिस्सा हैं और आपके शरीर को फंगल और परजीवी संक्रमण से बचाने में ...more
कभी-कभी, कुछ चिकित्सीय स्थितियां और दवाएं ईओसिनोफिल के उच्च स्तर का कारण बनती हैं।
ईओसिनोफिलिया क्या है?
ईओसिनोफिल श्वेत रक्त कोशिकाओं में से एक हैं जो आपकी प्रतिरक्षा प्रणाली को सपोर्ट करती हैं। वे एलर्जी के खिलाफ आपके शरीर की रक्षा प्रणाली का हिस्सा हैं और आपके शरीर को फंगल और परजीवी संक्रमण से बचाने में ...more
79 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
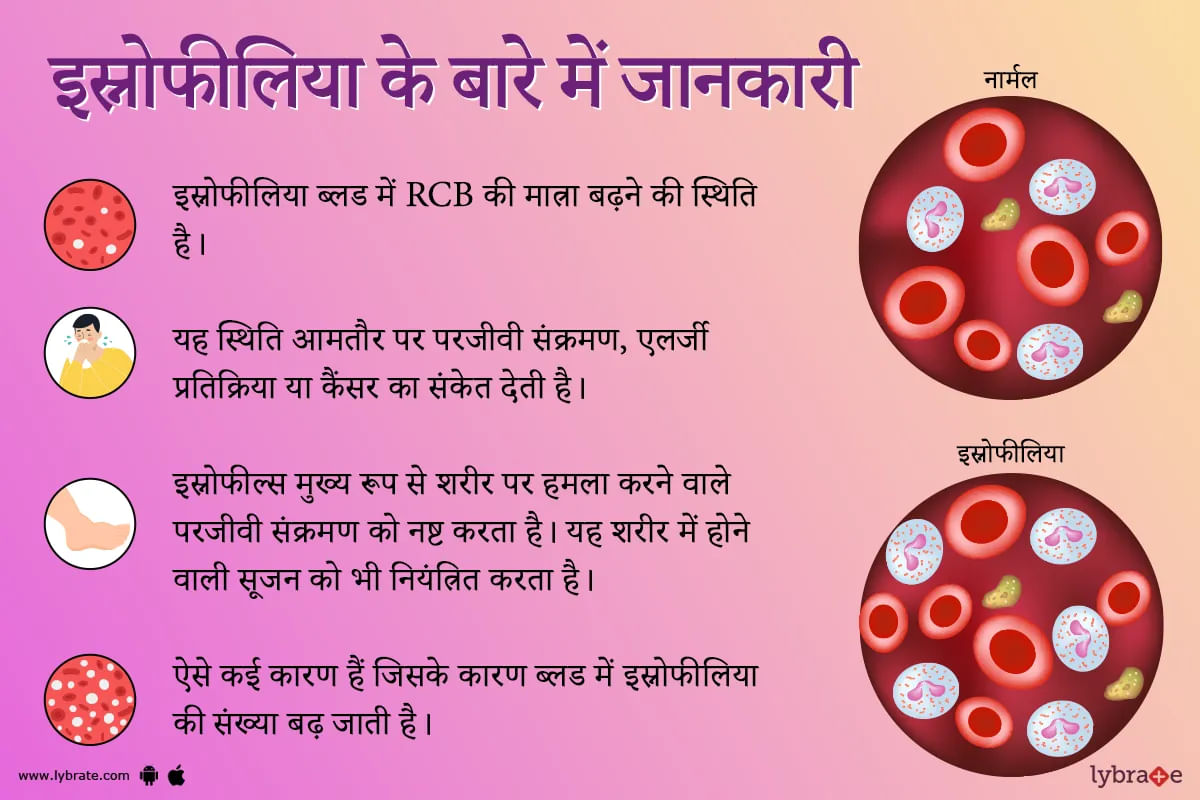
इओसिनोफिलिया एक ऐसी स्थिति है जब आपके रक्त में इओसिनोफिल के सामान्य स्तर से अधिक पाया जाता है। इओसिनोफिल्स एक प्रकार की बीमारी से लड़ने वाली श्वेत रक्त कोशिका हैं। इसे कई बार सामान्य भाषा में स्नोफीलिया कहा जाता है। यह स्थिति अक्सर परजीवी संक्रमण, एलर्जी प्रतिक्रिया या कैंसर का संकेत देती है।
आपके रक्त में उच्च स्तर के इओसिनोफिल्स कई जगहों पर पाए जा सकते हैं खून में (रक्त इओसिनोफिलिया) या संक्रमण या सूजन (ऊतक इओसिनोफिलिया) के स्थान पर ऊतकों में भी हो सकते हैं।
ऊतक इओसिनोफिलिया ...more
आपके रक्त में उच्च स्तर के इओसिनोफिल्स कई जगहों पर पाए जा सकते हैं खून में (रक्त इओसिनोफिलिया) या संक्रमण या सूजन (ऊतक इओसिनोफिलिया) के स्थान पर ऊतकों में भी हो सकते हैं।
ऊतक इओसिनोफिलिया ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
1. Esophagitis: Prolonged acid or bile reflux (Gastroesophageal reflux disease GERD) from the stomach can cause injury to the lower esophagus and causing esophagitis. It can be either Erosive esophagitis or Non-erosive reflux disease (NERD). Gastroscopy is usually recommended to document the extent of the injury. Prolonged untreated GERD can cause Barret s esophagitis, upper GI bleeding or Cancer of the food pipe. Diagnosis usually involves Gastroscopy, 24 hours Phmetry and Esophageal manometry....more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The surgical procedure to remove the oesophagus (the tube between your stomach and mouth), partially or completely, and reconstruct it by using a section of the large intestine or stomach is called esophagectomy.
Esophagectomy is commonly used to treat oesophageal cancer.
Uses:
Early-stage oesophageal cancer is frequently treated with an esophagectomy. Other than that, esophagectomy is also performed to treat oesophageal dysplasia (a condition in which cells in the oes...more
Esophagectomy is commonly used to treat oesophageal cancer.
Uses:
Early-stage oesophageal cancer is frequently treated with an esophagectomy. Other than that, esophagectomy is also performed to treat oesophageal dysplasia (a condition in which cells in the oes...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The Eosinophilic disorders are one of the major hematological diseases, which deal with the white blood cells in the human body. The Eosinophils or the white blood cells play an important role in the human body while responding to asthma, allergic reactions, and infections that are caused due to parasites. Eosinophils not only play an important role in protective immunity against parasites but also contribute a lot to inflammation which occurs during allergic disorders.
Different disord...more
Different disord...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Kidney stones are often small enough and pass through urine without much bother. Most kidney stones are smaller than 4 mm in diameter. Having said this, even the smallest of kidney stones can be really painful until they pass through urine. It typically takes a couple of days for the body to get rid of it. While medication and self-care are the foremost options, there are a range of other options as well available for treating kidney stones.
Admission to a Hospital-
You must ge...more
Admission to a Hospital-
You must ge...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Percutaneous Nephrolithotomy (PCNL) is an invasive surgical procedure in which a large (more than 2cm), irregularly shaped, or very dense kidney stone/stones are removed through a small incision in the skin, when other non-invasive procedures are not feasible anymore. Stones are extracted, plucked, or vacuumed by using surgical instruments through a small cut in the back. It is performed under general anesthesia and is considered one of the most efficient approaches to stone removal.
Ri...more
Ri...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Hepatitis C is a viral infection that causes liver inflammation, sometimes leading to serious liver damage. The hepatitis C virus (HCV) spreads through contaminated blood.
Signs and Symptoms :
Bleeding easily
Bruising easily
Fatigue
Poor appetite
Yellow discoloration of the skin and eyes (jaundice)
Dark-colored urine
Itchy skin
Fluid buildup in your abdomen (ascites)
Swelling in your legs
Weight loss
Confusion, drowsiness and slurred spee...more
Signs and Symptoms :
Bleeding easily
Bruising easily
Fatigue
Poor appetite
Yellow discoloration of the skin and eyes (jaundice)
Dark-colored urine
Itchy skin
Fluid buildup in your abdomen (ascites)
Swelling in your legs
Weight loss
Confusion, drowsiness and slurred spee...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Hepatitis C is a viral infection that causes liver inflammation, sometimes leading to serious liver damage. The hepatitis C virus (HCV) spreads through contaminated blood.
Signs and Symptoms :
Bleeding easily
Bruising easily
Fatigue
Poor appetite
Yellow discoloration of the skin and eyes (jaundice)
Dark-colored urine
Itchy skin
Fluid buildup in your abdomen (ascites)
Swelling in your legs
Weight loss
Confusion, drowsiness and slurred spee...more
Signs and Symptoms :
Bleeding easily
Bruising easily
Fatigue
Poor appetite
Yellow discoloration of the skin and eyes (jaundice)
Dark-colored urine
Itchy skin
Fluid buildup in your abdomen (ascites)
Swelling in your legs
Weight loss
Confusion, drowsiness and slurred spee...more
Book appointment with top doctors for Meckel'S Diverticulum treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously