Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Leg Pain Tips
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Orthopedic Doctor•Pune
1. Dr. Shubhangi patil
Https://www. Lybrate. Com/pune/doctor/dr-shubhangi-patil-ayurveda-3 ;
Bachelor of ayurveda, medicine and surgery (bams), pg diploma in emergency medical services
36 years experience 500 at clinic
Dr. Shubhangi patil is an ayurvedic doctor and physiotherapist who graduated from tilak ayurveda mahavidalya & postgraduate institute, pune university, with a bams degree. She also holds a pg diploma in eme...more
93 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
1. Dr. Adithya hande
Https://www. Lybrate. Com/bangalore/doctor/dr-adithya-hande-acupuncturist ;
Bachelor of naturopathy & yogic sciences (bnys), msc psychiatry
7 years experience 300 at clinic 150 online
As a physiotherapist and specialist in yoga and naturopathy, he gives incredible client care. He listens to people's problems with great patience. As an orthopedist, he provides services of the highest calibre. He has...more
154 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Orthopedic Doctor•
Top 10 Doctors for Foot Pain in bangalore
1. Dr. Rohini Bv
https://www.lybrate.com/bangalore/doctor/dr-rohini-bv-ayurveda
BAMS, YIC, DEC Ayurvedic Doctors Electronic City, Bangalore
13 Years Experience 500 at clinic
She is a respected doctor who has dealt with many patients who had complicated problems. She is an expert Ayurvedic physician. She is a fantastic health expert and helps with pain management.
75 people found this helpful
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
In such lockdown time we are seeing more and more cases of leg pain and cramps later diagnosed to have clots in veins of leg which happens due to inactivity and sedentary lifestyle plus dehydration due to summer. We tend to not exercise during lockdown time. So be careful. Keep doing stretching exercises for legs and drink lots of water
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Physiotherapist•Hyderabad
An occasional tingling sensation in the hands or feet is normal and probably happens to everybody. But if this happens at a higher intensity or frequency than the normal amount and if it is accompanied by pain, it needs attention.
Commonly called the pins and needles feeling, it is irritating and distracting. Sometimes, this is a symptom of more complicated underlying issues. For this reason, this problem should not be ignored, even if it doesn t seem like much of a problem.
...more
Commonly called the pins and needles feeling, it is irritating and distracting. Sometimes, this is a symptom of more complicated underlying issues. For this reason, this problem should not be ignored, even if it doesn t seem like much of a problem.
...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
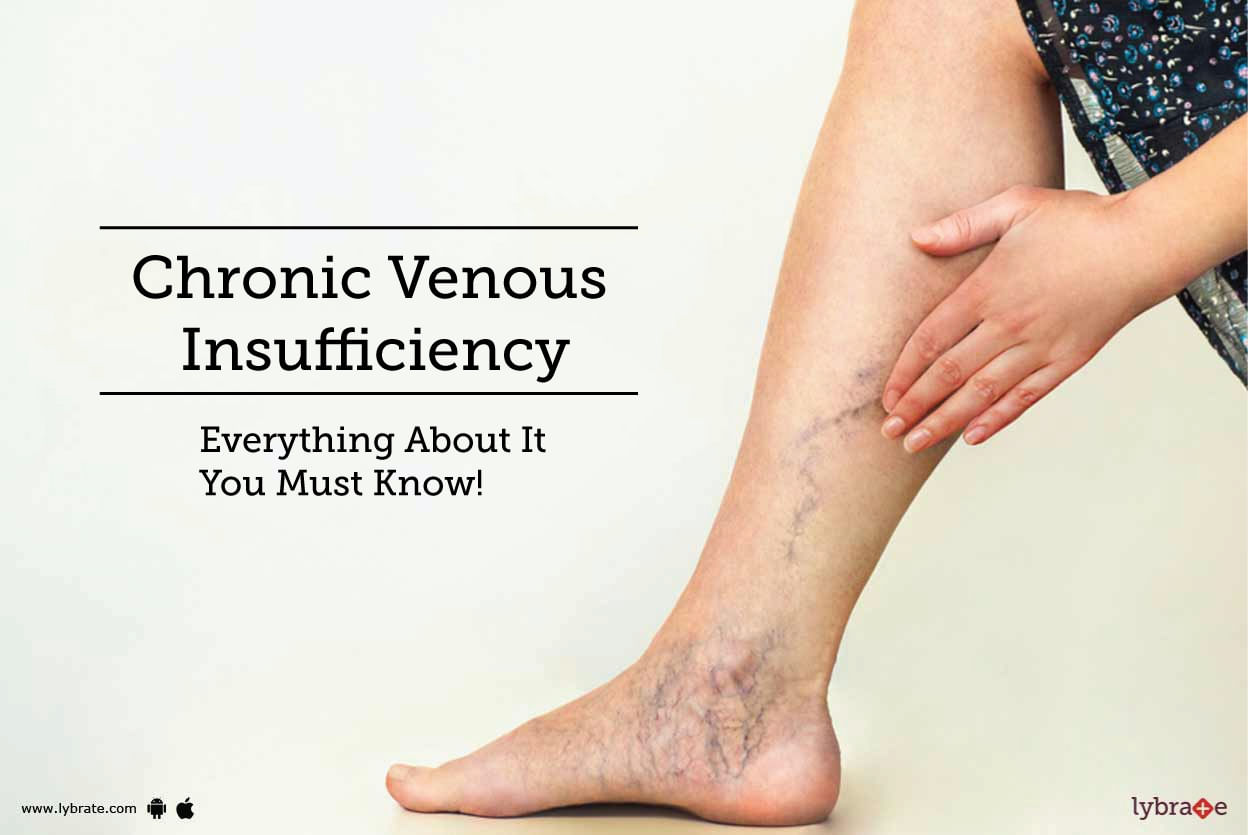
Chronic Venous Insufficiency is an abnormal condition of the leg veins. It occurs when either the walls or the one-way valves of the veins cannot work effectively. This
makes it difficult for the veins to send the impure blood from the legs to the heart. This results in impure flowing backward and collecting at places in the veins. It can
cause swelling, pain, and changes in skin and over time may lead to ulcers in legs.
Causes of Chronic Venous Insufficiency
Veins retu...more
makes it difficult for the veins to send the impure blood from the legs to the heart. This results in impure flowing backward and collecting at places in the veins. It can
cause swelling, pain, and changes in skin and over time may lead to ulcers in legs.
Causes of Chronic Venous Insufficiency
Veins retu...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
MBBS Bachelor of Medicine and Bachelor o...read more
Orthopedic Doctor•Bhubaneswar
Shin splints' is a condition, which is characterized by pain in the shin bone, the bone that is present in front of the leg. Shin splints tend to occur quite frequently in runners and dancers as their activities tend to stress the shin bone.
Causes: When excess force is applied to the shinbone, it may result in swelling of the muscles, causing pain and inflammation. It may also occur from stress reactions to fractures in the bone. Cracks tend to develop due to constant application of fo...more
Causes: When excess force is applied to the shinbone, it may result in swelling of the muscles, causing pain and inflammation. It may also occur from stress reactions to fractures in the bone. Cracks tend to develop due to constant application of fo...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Leg cramps is a very common condition which is characterized by tight and painful leg muscles. The calf muscles are the most commonly affected; it can spread further down to your thighs and feet. Once the cramping gets better, you might experience a tender leg coupled with a numbing feeling for a few minutes.
The causes of leg cramps are varied. If it is caused due to an underlying condition, it is known as secondary leg cramps. The causes of secondary leg cramps include vigorous exerci...more
The causes of leg cramps are varied. If it is caused due to an underlying condition, it is known as secondary leg cramps. The causes of secondary leg cramps include vigorous exerci...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
MBBS, MS - General Surgery, FRCSED, Surg...read more
Vascular Surgeon•Hyderabad
Leg bypass surgery is needed when the patient suffers from peripheral artery disease. PAD is a very common condition in elderly people, where the rate of flow of blood to the limbs (in this case, the legs) is reduced due to narrowing of the blood vessels.
Causes and risk factors-
The narrowing of the blood vessels occurs due to excess calcium accumulation and fat deposits in the walls of the arteries. The following are the risk factors of PAD-
Age (60 years and above...more
Causes and risk factors-
The narrowing of the blood vessels occurs due to excess calcium accumulation and fat deposits in the walls of the arteries. The following are the risk factors of PAD-
Age (60 years and above...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
BPTh/BPT, Weight Management Specialist, ...read more
Dietitian/Nutritionist•Kolkata
The sciatic nerve is one of the largest nerves in the body. It goes from the lower back all the way down to the base of the leg. When there is a disorder associated with the sciatic nerve, it is known as Sciatica.
Sciatica, however, does not necessarily need a surgery or a very elaborate procedure to fix the problem. Most commonly, it is treated simply by practicing a number of simple exercises. Here are some of the most common exercises prescribed to treat Sciatica:
more
Sciatica, however, does not necessarily need a surgery or a very elaborate procedure to fix the problem. Most commonly, it is treated simply by practicing a number of simple exercises. Here are some of the most common exercises prescribed to treat Sciatica:
more
Book appointment with top doctors for Leg Pain treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously