Get the App
For Doctors
Login/Sign-up
Health Feed
Find Doctors
Health Packages
AllQ&AsTips
Intubation Tips
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
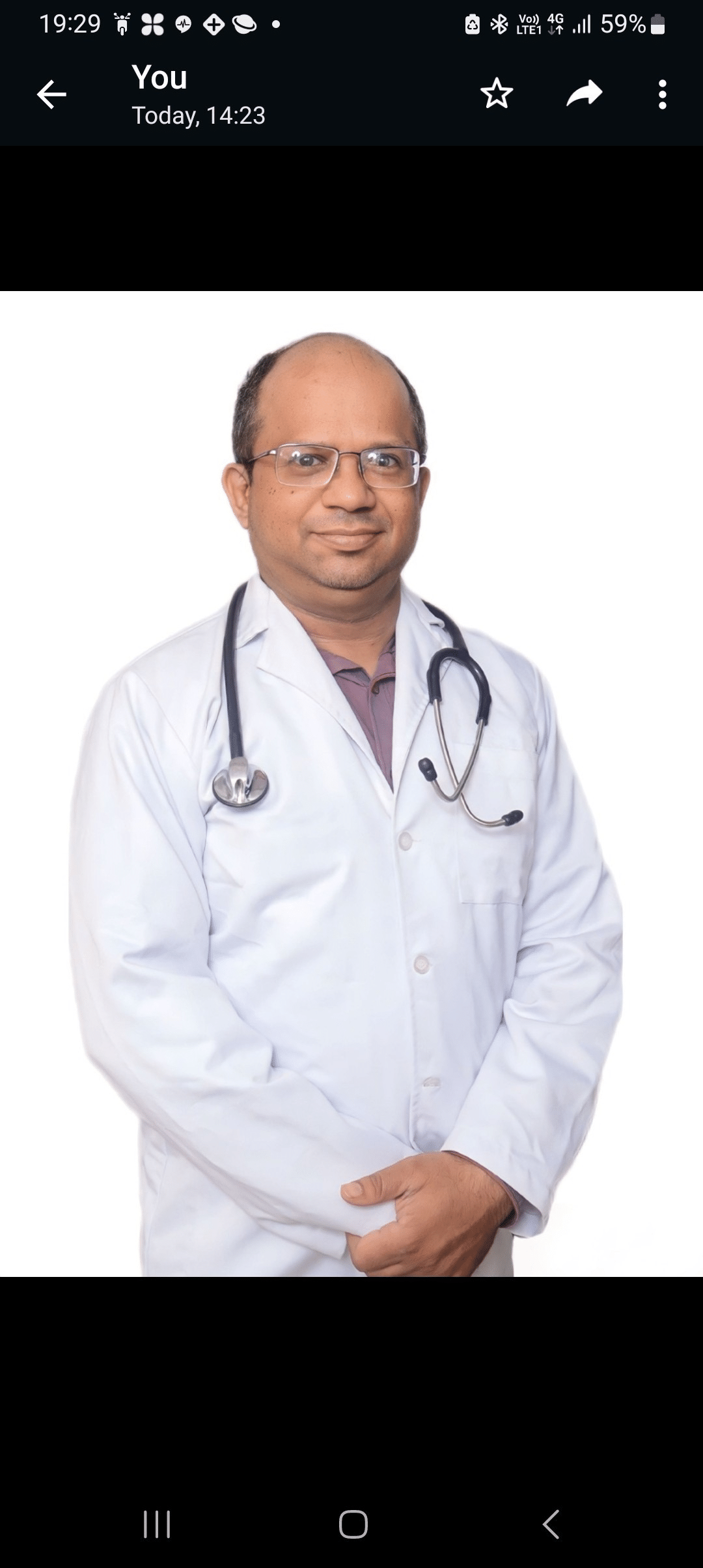
सीपीआर का मतलब है कार्डियोपल्मोनरी रिससिटेशन। यह भी एक तरह की प्राथमिक चिकित्सा यानी फर्स्ट एड है। जब किसी पीड़ित को सांस लेने में दिक्कत हो या फिर वो सांस न ले पा रहा हो और बेहोश जो जाए तो सीपीआर से उसकी जान बचाई जा सकती है। बिजली का झटका लगने पर, पानी में डूबने पर और दम घुटने पर सीपीआर से पीड़ित को आराम पहुंचाया जा सकता है। हार्ट अटैक यानी दिल का दौरा पड़ने पर तो सबसे पहले और समय पर सीपीआर दे दिया जाय तो पीड़ित की जान बचाने की संभावना कई गुना बढ़ जाती है।
अगर किसी...more
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
Orthopedic Doctor•Delhi
1. Dr. Hemant gaur
Https://www. Lybrate. Com/delhi/doctor/dr-hemant-gaur-physiotherapist
Mpt, mphill
11 years experience 200 at clinic 300 online
;
He is a physiotherapist who is well-known for treating people with complicated conditions. He also works as a homecare physiotherapist. He obtained his outstanding education and clinical experience as an mpt at manav rachna international university and as a mphill at opjs university. His...more
309 people found this helpful
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
Pulmonologist•Hyderabad
Dr. K. K. Reddy
Https://www. Lybrate. Com/hyderabad/doctor/dr-k-k-reddy-pulmonologist
Mbbs diploma in tuberculosis and chest diseases dtcd
27 years experience - 350 at clinic
He has significant medical knowledge in pulmonology and is well recognised as a leading medical expert. A name like his would be hard to forget. Professionalism was refined during his 1995 graduation from the mbbs at osmania medical college in hyderabad, from which he received high honours.
A la...more
Https://www. Lybrate. Com/hyderabad/doctor/dr-k-k-reddy-pulmonologist
Mbbs diploma in tuberculosis and chest diseases dtcd
27 years experience - 350 at clinic
He has significant medical knowledge in pulmonology and is well recognised as a leading medical expert. A name like his would be hard to forget. Professionalism was refined during his 1995 graduation from the mbbs at osmania medical college in hyderabad, from which he received high honours.
A la...more
10 people found this helpful
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Laparoscopy surgery is a very vital component of the hernia repair. Studies have shown that many patients have a better outcome when they opt for laparoscopic surgery. Candidates eligible for this mode of surgery include those with bilateral inguinal hernias, ventral hernias, and recurrent hernia. People associated with athletics and other outdoor sports prefer to go for a laparoscopic hernia surgery as it ensures a speedy recovery and minimal tissue invasion (due to small incisions).
L...more
L...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Esophagectomy is a procedure of removing a part of the esophagus and reconstructing the same using another organ of the body. The oesophagus is the tube that connects the stomach and the mouth. This procedure is often performed in an advanced stage of esophageal cancer and Barrett s esophagus. This procedure removes the cancer cells from the esophagus and gives relief from the symptoms. The organs from where the reconstructing tissues are taken are generally large intestine and stomach.
more
more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Ovarian cysts are fluid-filled sacs in the ovaries, often in multiples, which are very common in women. This is absolutely different condition from polycystic ovaries. Most of them are benign and not indicative of an underlying problem. They produce no specific symptoms and even if detected, can be watched over a period of time. Treatment may be required only if there are serious symptoms or there is higher possibility of cancerous nature of the cyst. Read on to know more.
Types
<...more
Types
<...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Laparoscopy is one of the most common procedures for diagnosing and removing endometriosis. Instead of giving a big incision, this procedure of surgery uses lightweight instrument through a small hole or incision. There could be one or more incisions based on the number of instruments that require access inside the body. This procedure involves the use of a camera to ascertain endometriosis as well as treat it in the same sitting. This brings drastic improvement in infertility as well as pain as...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
It is a common wish of every individual to have flawless skin. Everyone wants skin sans spots, wrinkles or marks and this increasing demand has created a market for anti-aging, anti-wrinkle and other such creams that promise their customers flawless skin. But, these creams do not offer permanent solutions which is why people often opt for treatments such as chemical peels and radiofrequency. These treatments too are not the best.
HIFU or High-Intensity Focused Ultrasound is a new techno...more
HIFU or High-Intensity Focused Ultrasound is a new techno...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Your spine or backbone is composed of 26 bone discs, known as vertebrae. The vertebra shields your spinal cord and allows you to bend forwards and backwards, and stand. However, a number of problems, such as the following can change the structure or cause the vertebrae and its surrounding tissues to become damaged
Injuries
Infections
Tumours
Changes in bone formation due to ageing herniated disks, spinal stenosis
Conditions like scoliosis and ankylosing spo...more
Injuries
Infections
Tumours
Changes in bone formation due to ageing herniated disks, spinal stenosis
Conditions like scoliosis and ankylosing spo...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Laparoscopy surgery is a very vital component of the hernia repair. Studies have shown that many patients have a better outcome when they opt for laparoscopic surgery. Candidates eligible for this mode of surgery include those with bilateral inguinal hernias, ventral hernias, and recurrent hernia. People associated with athletics and other outdoor sports prefer to go for a laparoscopic hernia surgery as it ensures a speedy recovery and minimal tissue invasion (due to small incisions).
L...more
L...more
Book appointment with top doctors for Intubation treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously