Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Hepatic Encephalopathy Health Feed
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Hepatitis C is a viral infection that causes liver inflammation, sometimes leading to serious liver damage. The hepatitis C virus (HCV) spreads through contaminated blood.
Signs and Symptoms :
Bleeding easily
Bruising easily
Fatigue
Poor appetite
Yellow discoloration of the skin and eyes (jaundice)
Dark-colored urine
Itchy skin
Fluid buildup in your abdomen (ascites)
Swelling in your legs
Weight loss
Confusion, drowsiness and slurred spee...more
Signs and Symptoms :
Bleeding easily
Bruising easily
Fatigue
Poor appetite
Yellow discoloration of the skin and eyes (jaundice)
Dark-colored urine
Itchy skin
Fluid buildup in your abdomen (ascites)
Swelling in your legs
Weight loss
Confusion, drowsiness and slurred spee...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Hepatitis C is a viral infection that causes liver inflammation, sometimes leading to serious liver damage. The hepatitis C virus (HCV) spreads through contaminated blood.
Signs and Symptoms :
Bleeding easily
Bruising easily
Fatigue
Poor appetite
Yellow discoloration of the skin and eyes (jaundice)
Dark-colored urine
Itchy skin
Fluid buildup in your abdomen (ascites)
Swelling in your legs
Weight loss
Confusion, drowsiness and slurred spee...more
Signs and Symptoms :
Bleeding easily
Bruising easily
Fatigue
Poor appetite
Yellow discoloration of the skin and eyes (jaundice)
Dark-colored urine
Itchy skin
Fluid buildup in your abdomen (ascites)
Swelling in your legs
Weight loss
Confusion, drowsiness and slurred spee...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
Hepatic encephalopathy is a condition associated with liver cirrhosis. It refers to an abnormal level of consciousness caused by liver failure when toxins start building up in the brain as the damaged liver is unable to remove them from the body. It happens due to the diversion of the portal blood into the systemic circulation and is experienced by patients who have advanced stage of liver dysfunction. It is also a result of the impact of neurotoxic substances, which take a seat into the body af...more
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
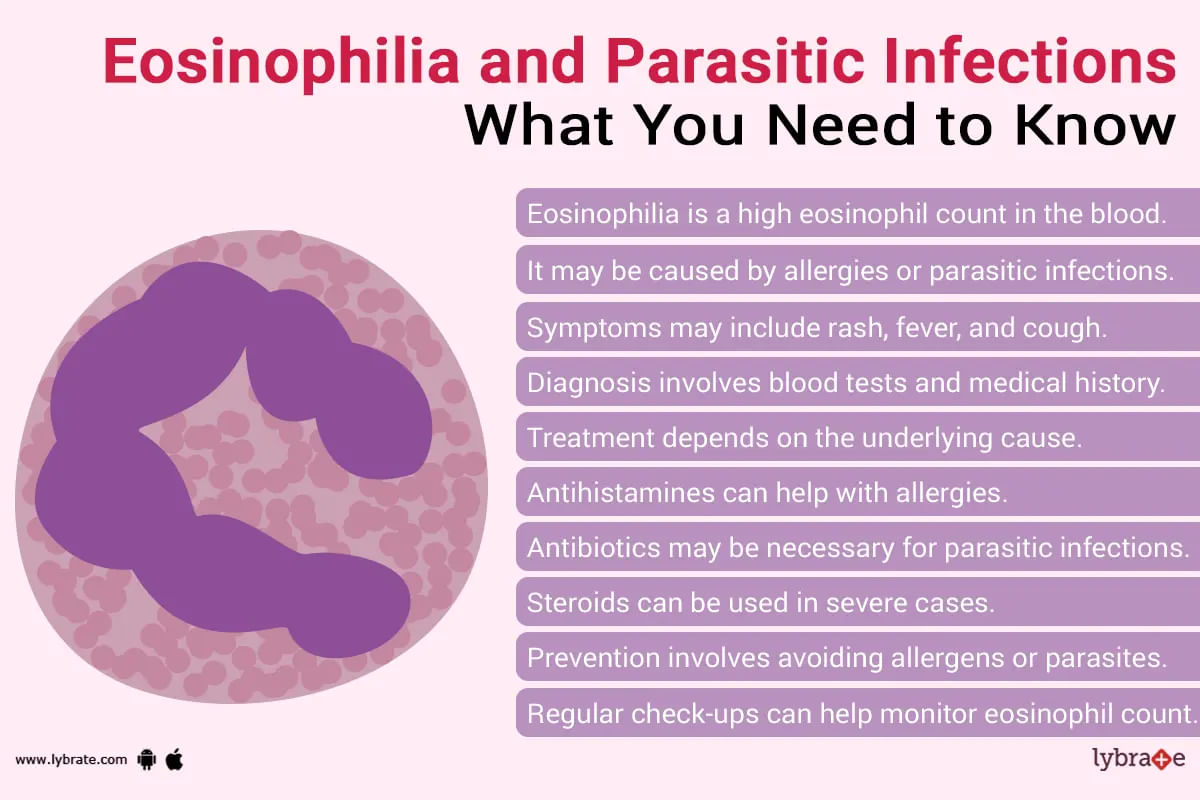
Eosinophilia is when the level of eosinophils is higher than normal level in blood. Eosinophils are a type of WBC (white blood cells). These cells are the immune system of our body which helps to fight diseases. When there is parasitic infection, bacterial infection or any type of allergic reaction, these cells help us to fight it. It is also useful in defeating cancer.
If there is an attack of foreign substance/lives there is an increase at levels of eosinophils in blood or if attack i...more
If there is an attack of foreign substance/lives there is an increase at levels of eosinophils in blood or if attack i...more
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
ईओसिनोफिलिया तब होता है जब आपका शरीर असामान्य रूप से ईओसिनोफिल पैदा करता है। ईओसिनोफिल कई श्वेत रक्त कोशिकाओं में से एक हैं जो आपकी प्रतिरक्षा प्रणाली का सहयोग करती हैं।
कभी-कभी, कुछ चिकित्सीय स्थितियां और दवाएं ईओसिनोफिल के उच्च स्तर का कारण बनती हैं।
ईओसिनोफिलिया क्या है?
ईओसिनोफिल श्वेत रक्त कोशिकाओं में से एक हैं जो आपकी प्रतिरक्षा प्रणाली को सपोर्ट करती हैं। वे एलर्जी के खिलाफ आपके शरीर की रक्षा प्रणाली का हिस्सा हैं और आपके शरीर को फंगल और परजीवी संक्रमण से बचाने में ...more
कभी-कभी, कुछ चिकित्सीय स्थितियां और दवाएं ईओसिनोफिल के उच्च स्तर का कारण बनती हैं।
ईओसिनोफिलिया क्या है?
ईओसिनोफिल श्वेत रक्त कोशिकाओं में से एक हैं जो आपकी प्रतिरक्षा प्रणाली को सपोर्ट करती हैं। वे एलर्जी के खिलाफ आपके शरीर की रक्षा प्रणाली का हिस्सा हैं और आपके शरीर को फंगल और परजीवी संक्रमण से बचाने में ...more
79 people found this helpful
Asked for female, 40 years old from Leh
Share
Bookmark
Report
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
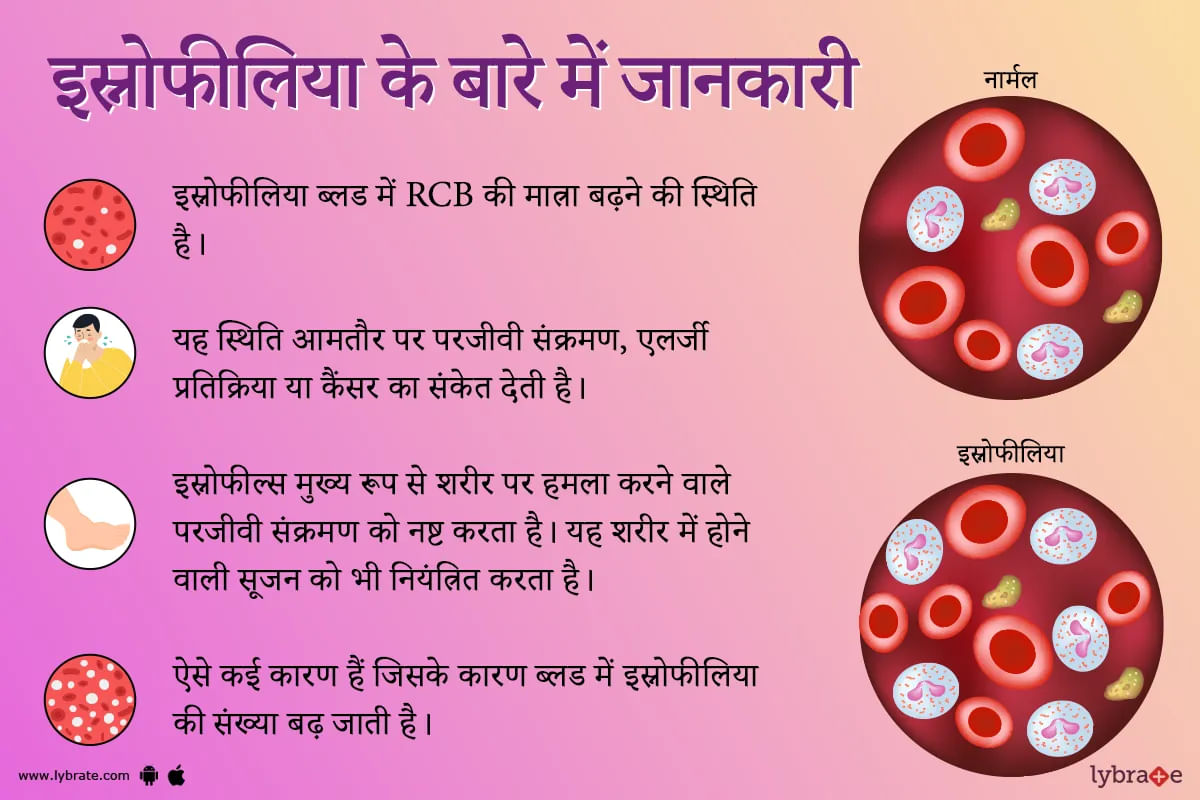
इओसिनोफिलिया एक ऐसी स्थिति है जब आपके रक्त में इओसिनोफिल के सामान्य स्तर से अधिक पाया जाता है। इओसिनोफिल्स एक प्रकार की बीमारी से लड़ने वाली श्वेत रक्त कोशिका हैं। इसे कई बार सामान्य भाषा में स्नोफीलिया कहा जाता है। यह स्थिति अक्सर परजीवी संक्रमण, एलर्जी प्रतिक्रिया या कैंसर का संकेत देती है।
आपके रक्त में उच्च स्तर के इओसिनोफिल्स कई जगहों पर पाए जा सकते हैं खून में (रक्त इओसिनोफिलिया) या संक्रमण या सूजन (ऊतक इओसिनोफिलिया) के स्थान पर ऊतकों में भी हो सकते हैं।
ऊतक इओसिनोफिलिया ...more
आपके रक्त में उच्च स्तर के इओसिनोफिल्स कई जगहों पर पाए जा सकते हैं खून में (रक्त इओसिनोफिलिया) या संक्रमण या सूजन (ऊतक इओसिनोफिलिया) के स्थान पर ऊतकों में भी हो सकते हैं।
ऊतक इओसिनोफिलिया ...more
Asked for male, 28 years old from Malappuram
Share
Bookmark
Report
Asked for male, 26 years old from Malappuram
Share
Bookmark
Report
Asked for Male, 52 years old from Mumbai
Share
Bookmark
Report
Health Query
Share
Bookmark
Report
This condition usually occurs with those having curly hairs. There are a few things you may do to avoid getting skin bumps and rash:
Shave with the grain of the beard and do not stretch the skin. Use only one stroke over each area of the beard.
Use of an electric shaver may also help the condition because it does not cut as close as blades do. Use the electric razor on high setting to avoid close shaving and prepare beard with electric razor pre-shave. Do not stretch the skin ...more
Shave with the grain of the beard and do not stretch the skin. Use only one stroke over each area of the beard.
Use of an electric shaver may also help the condition because it does not cut as close as blades do. Use the electric razor on high setting to avoid close shaving and prepare beard with electric razor pre-shave. Do not stretch the skin ...more
7 people found this helpful
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
1. Esophagitis: Prolonged acid or bile reflux (Gastroesophageal reflux disease GERD) from the stomach can cause injury to the lower esophagus and causing esophagitis. It can be either Erosive esophagitis or Non-erosive reflux disease (NERD). Gastroscopy is usually recommended to document the extent of the injury. Prolonged untreated GERD can cause Barret s esophagitis, upper GI bleeding or Cancer of the food pipe. Diagnosis usually involves Gastroscopy, 24 hours Phmetry and Esophageal manometry....more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The surgical procedure to remove the oesophagus (the tube between your stomach and mouth), partially or completely, and reconstruct it by using a section of the large intestine or stomach is called esophagectomy.
Esophagectomy is commonly used to treat oesophageal cancer.
Uses:
Early-stage oesophageal cancer is frequently treated with an esophagectomy. Other than that, esophagectomy is also performed to treat oesophageal dysplasia (a condition in which cells in the oes...more
Esophagectomy is commonly used to treat oesophageal cancer.
Uses:
Early-stage oesophageal cancer is frequently treated with an esophagectomy. Other than that, esophagectomy is also performed to treat oesophageal dysplasia (a condition in which cells in the oes...more
Book appointment with top doctors for Hepatic Encephalopathy treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously