Get the App
For Doctors
Login/Sign-up
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Eosinophilic Esophagitis Tips
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
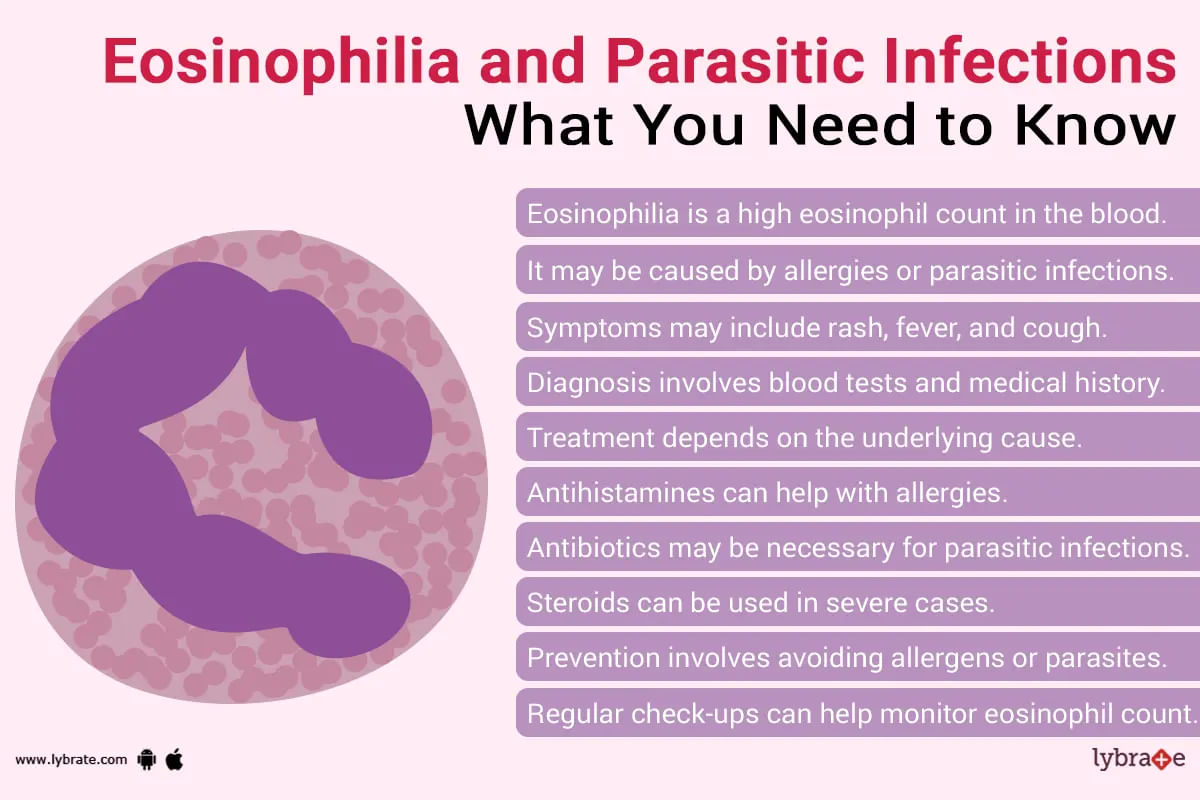
Eosinophilia is when the level of eosinophils is higher than normal level in blood. Eosinophils are a type of WBC (white blood cells). These cells are the immune system of our body which helps to fight diseases. When there is parasitic infection, bacterial infection or any type of allergic reaction, these cells help us to fight it. It is also useful in defeating cancer.
If there is an attack of foreign substance/lives there is an increase at levels of eosinophils in blood or if attack i...more
If there is an attack of foreign substance/lives there is an increase at levels of eosinophils in blood or if attack i...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
ईओसिनोफिलिया तब होता है जब आपका शरीर असामान्य रूप से ईओसिनोफिल पैदा करता है। ईओसिनोफिल कई श्वेत रक्त कोशिकाओं में से एक हैं जो आपकी प्रतिरक्षा प्रणाली का सहयोग करती हैं।
कभी-कभी, कुछ चिकित्सीय स्थितियां और दवाएं ईओसिनोफिल के उच्च स्तर का कारण बनती हैं।
ईओसिनोफिलिया क्या है?
ईओसिनोफिल श्वेत रक्त कोशिकाओं में से एक हैं जो आपकी प्रतिरक्षा प्रणाली को सपोर्ट करती हैं। वे एलर्जी के खिलाफ आपके शरीर की रक्षा प्रणाली का हिस्सा हैं और आपके शरीर को फंगल और परजीवी संक्रमण से बचाने में ...more
कभी-कभी, कुछ चिकित्सीय स्थितियां और दवाएं ईओसिनोफिल के उच्च स्तर का कारण बनती हैं।
ईओसिनोफिलिया क्या है?
ईओसिनोफिल श्वेत रक्त कोशिकाओं में से एक हैं जो आपकी प्रतिरक्षा प्रणाली को सपोर्ट करती हैं। वे एलर्जी के खिलाफ आपके शरीर की रक्षा प्रणाली का हिस्सा हैं और आपके शरीर को फंगल और परजीवी संक्रमण से बचाने में ...more
79 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
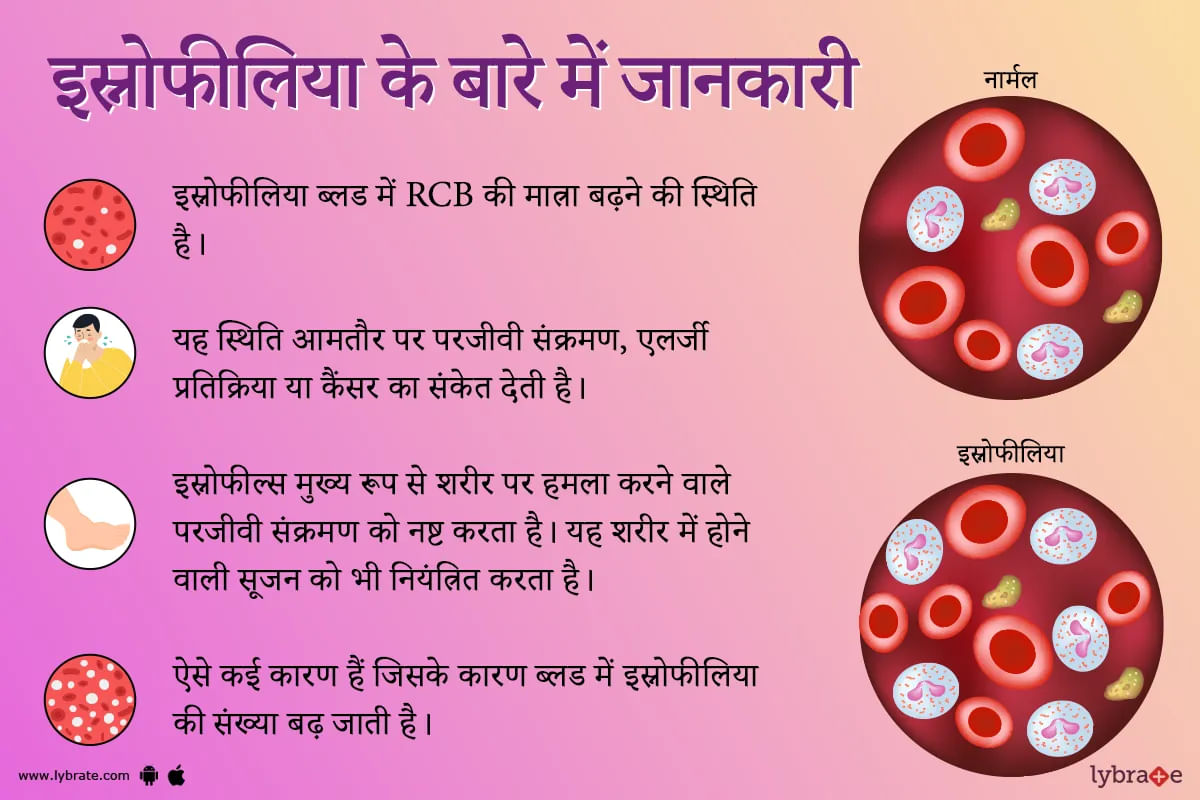
इओसिनोफिलिया एक ऐसी स्थिति है जब आपके रक्त में इओसिनोफिल के सामान्य स्तर से अधिक पाया जाता है। इओसिनोफिल्स एक प्रकार की बीमारी से लड़ने वाली श्वेत रक्त कोशिका हैं। इसे कई बार सामान्य भाषा में स्नोफीलिया कहा जाता है। यह स्थिति अक्सर परजीवी संक्रमण, एलर्जी प्रतिक्रिया या कैंसर का संकेत देती है।
आपके रक्त में उच्च स्तर के इओसिनोफिल्स कई जगहों पर पाए जा सकते हैं खून में (रक्त इओसिनोफिलिया) या संक्रमण या सूजन (ऊतक इओसिनोफिलिया) के स्थान पर ऊतकों में भी हो सकते हैं।
ऊतक इओसिनोफिलिया ...more
आपके रक्त में उच्च स्तर के इओसिनोफिल्स कई जगहों पर पाए जा सकते हैं खून में (रक्त इओसिनोफिलिया) या संक्रमण या सूजन (ऊतक इओसिनोफिलिया) के स्थान पर ऊतकों में भी हो सकते हैं।
ऊतक इओसिनोफिलिया ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
1. Esophagitis: Prolonged acid or bile reflux (Gastroesophageal reflux disease GERD) from the stomach can cause injury to the lower esophagus and causing esophagitis. It can be either Erosive esophagitis or Non-erosive reflux disease (NERD). Gastroscopy is usually recommended to document the extent of the injury. Prolonged untreated GERD can cause Barret s esophagitis, upper GI bleeding or Cancer of the food pipe. Diagnosis usually involves Gastroscopy, 24 hours Phmetry and Esophageal manometry....more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The surgical procedure to remove the oesophagus (the tube between your stomach and mouth), partially or completely, and reconstruct it by using a section of the large intestine or stomach is called esophagectomy.
Esophagectomy is commonly used to treat oesophageal cancer.
Uses:
Early-stage oesophageal cancer is frequently treated with an esophagectomy. Other than that, esophagectomy is also performed to treat oesophageal dysplasia (a condition in which cells in the oes...more
Esophagectomy is commonly used to treat oesophageal cancer.
Uses:
Early-stage oesophageal cancer is frequently treated with an esophagectomy. Other than that, esophagectomy is also performed to treat oesophageal dysplasia (a condition in which cells in the oes...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The Eosinophilic disorders are one of the major hematological diseases, which deal with the white blood cells in the human body. The Eosinophils or the white blood cells play an important role in the human body while responding to asthma, allergic reactions, and infections that are caused due to parasites. Eosinophils not only play an important role in protective immunity against parasites but also contribute a lot to inflammation which occurs during allergic disorders.
Different disord...more
Different disord...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
The surgical procedure to remove the oesophagus (the tube between your stomach and mouth), partially or completely, and reconstruct it by using a section of the large intestine or stomach is called esophagectomy.
Esophagectomy is commonly used to treat oesophageal cancer.
Uses:
Early-stage oesophageal cancer is frequently treated with an esophagectomy. Other than that, esophagectomy is also performed to treat oesophageal dysplasia (a condition in which cells in the oes...more
Esophagectomy is commonly used to treat oesophageal cancer.
Uses:
Early-stage oesophageal cancer is frequently treated with an esophagectomy. Other than that, esophagectomy is also performed to treat oesophageal dysplasia (a condition in which cells in the oes...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
The surgical procedure to remove the oesophagus (the tube between your stomach and mouth), partially or completely, and reconstruct it by using a section of the large intestine or stomach is called esophagectomy.
Esophagectomy is commonly used to treat oesophageal cancer.
Uses:
Early-stage oesophageal cancer is frequently treated with an esophagectomy. Other than that, esophagectomy is also performed to treat oesophageal dysplasia (a condition in which cells in the oes...more
Esophagectomy is commonly used to treat oesophageal cancer.
Uses:
Early-stage oesophageal cancer is frequently treated with an esophagectomy. Other than that, esophagectomy is also performed to treat oesophageal dysplasia (a condition in which cells in the oes...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
Adverse respiratory events (AREs) are leading causes of post-operative morbidity and mortality. Anesthesia is the use of medicine to prevent or reduce the feeling of pain or sensation during surgery or other painful procedures (such as getting stitches). Giving as an injection or through inhaled gases or vapours, different types of anesthesia affect the nervous system in various ways by blocking nerve impulses and, therefore, pain.
Anesthesia can help control your breathing, blood press...more
Anesthesia can help control your breathing, blood press...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
The surgical procedure to remove the oesophagus (the tube between your stomach and mouth), partially or completely, and reconstruct it by using a section of the large intestine or stomach is called esophagectomy.
Esophagectomy is commonly used to treat oesophageal cancer.
Uses:
Early-stage oesophageal cancer is frequently treated with an esophagectomy. Other than that, esophagectomy is also performed to treat oesophageal dysplasia (a condition in which cells in the oes...more
Esophagectomy is commonly used to treat oesophageal cancer.
Uses:
Early-stage oesophageal cancer is frequently treated with an esophagectomy. Other than that, esophagectomy is also performed to treat oesophageal dysplasia (a condition in which cells in the oes...more
Book appointment with top doctors for Eosinophilic Esophagitis treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously