Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTips
Carcinoid Health Feed
Health Query
Share
Bookmark
Report
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
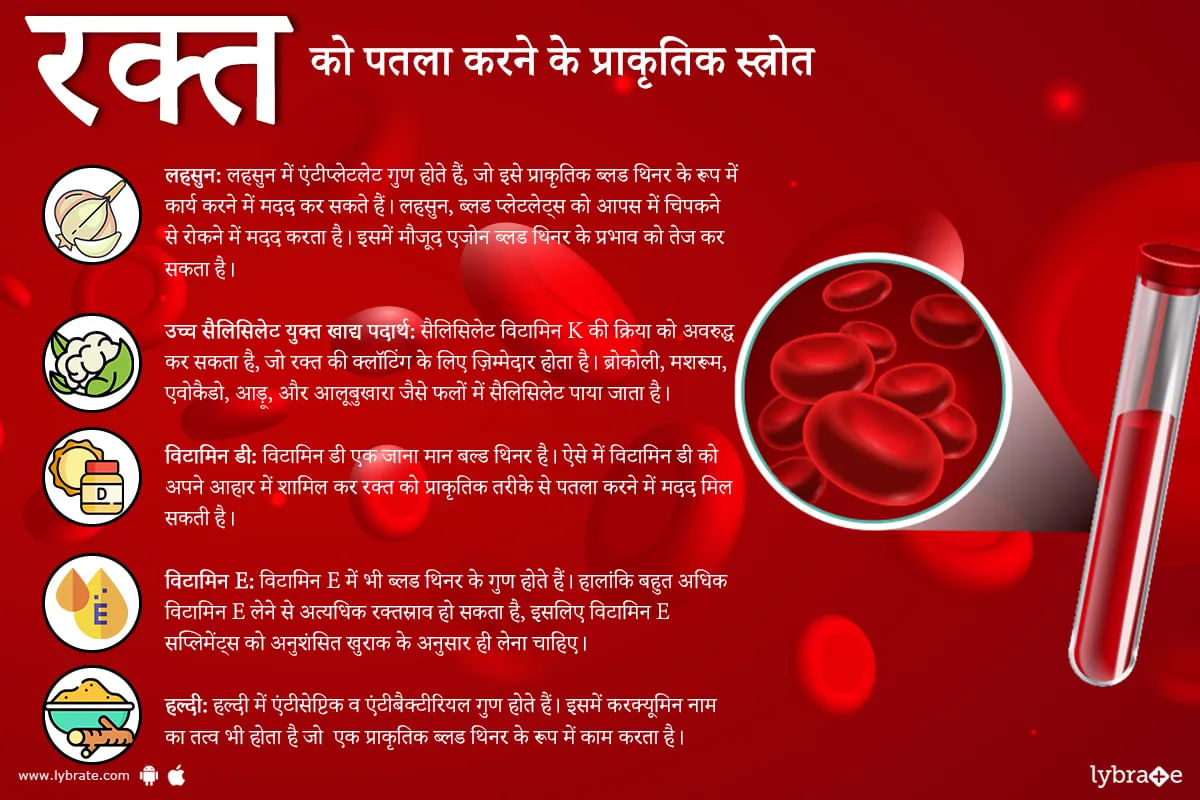
हमारे शरीर का हर अंग प्राकृतिक रूप से बनाए गए नियमों के अनुसार काम करता है। और अगर उसके किसी अंग में कोई बदलाव आ जाए तो स्वास्थ्य संबंधी दिक्कत आ जाती है। ठीक उसी प्रकार हमारे रक्त में भी अगर गाढ़ापन आ जाए या थक्का ना जमे या अधिक जमने लगे तो ये बहुत घातक हो सकता है।पर कुछ दवाओं या बीमारियों के कारण रक्त में ऐसे परिवर्तन आ जाते हैं।ऐसे में आपके मस्तिष्क और हृदय जैसे आवश्यक अंगों की आपूर्ति करने वाली महत्वपूर्ण धमनियों में रक्त के थक्के जमा हो सकते हैं, जिससे संभावित रूप से स्ट्रोक या दिल का दौरा ...more
Asked for male, 32 years old from Muzaffarnagar
Share
Bookmark
Report
Homeopathy Doctor•Mumbai
Polysomnography, a type of sleep study, is a multi-parametric test used in the study of sleep and as a diagnostic tool in sleep medicine. The test result is called a polysomnogram, also abbreviated psg. The name is derived from greek and latin roots: but why you want to know..
929 people found this helpful
Asked for female, 58 years old from Ahmedabad
Share
Bookmark
Report
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
MCh - Surgical Gastroenterology/G.I. Sur...read more
Surgical Gastroenterologist•Delhi
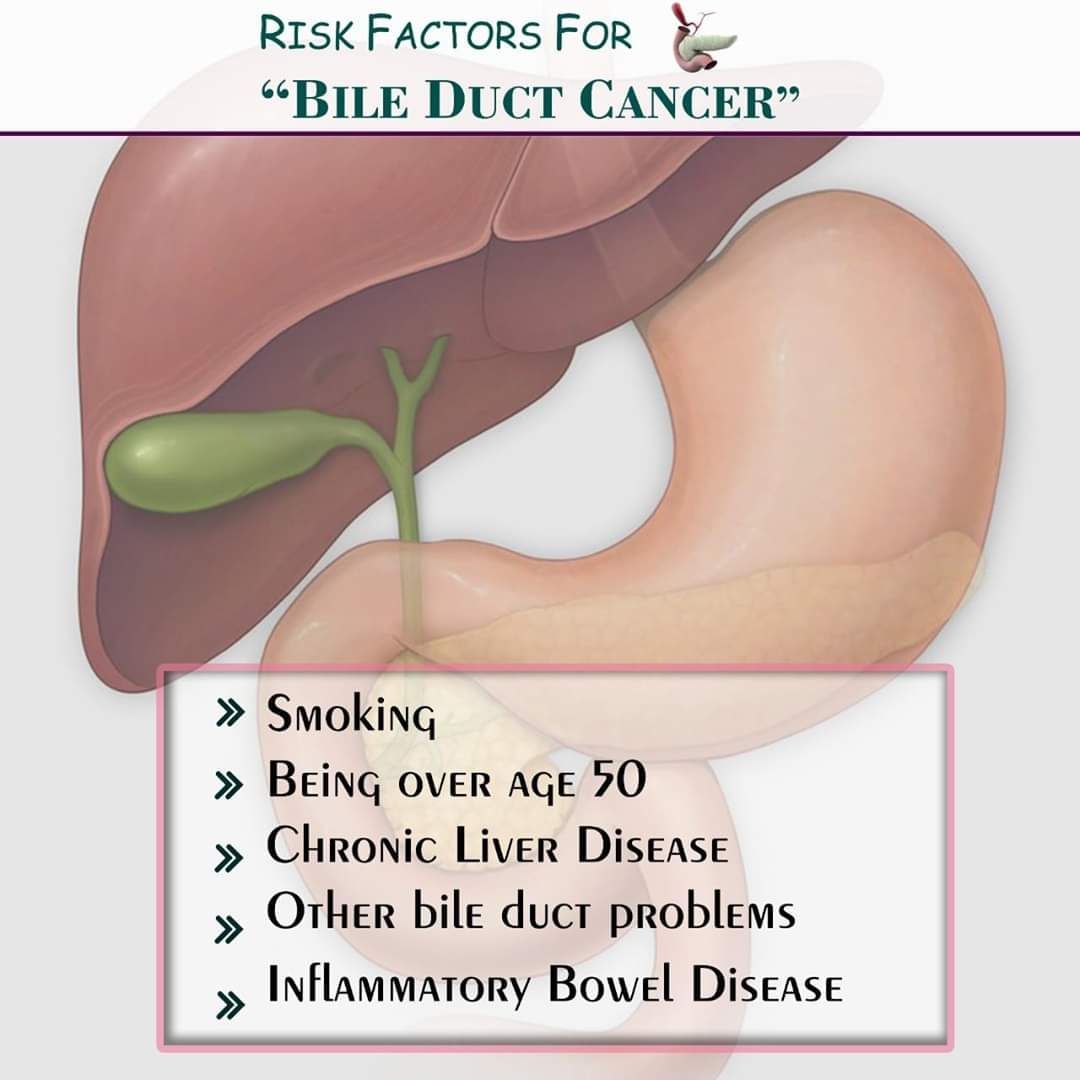
The bile duct is a thin tube which collects bile from the liver, stores it in the gall bladder and carries it to the intestine. Cancer of the bile duct is also known as cholangiocarcinoma. It can either involve the upper part or lower part of the bile duct and is called intrahepatic, hilar or distal cholangiocarcinoma.
Anything causing inflammation in the bile duct increases the risk of this cancer. Examples include
smoking.
choledochal cyst.
infection with liver flukes...more
Anything causing inflammation in the bile duct increases the risk of this cancer. Examples include
smoking.
choledochal cyst.
infection with liver flukes...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Dyslipidemia is a condition in which the patient has high or low levels of lipid in the blood. Lipids are fatty substances in the blood like cholesterol and triglycerides. A balanced and healthy diet can help the patient regulate Dyslipidemia condition. However, medication is often recommended by doctors in most cases.
Dyslipidemia is caused due to various reasons. Some common reasons are the high level of bad cholesterol, low levels of good cholesterol, high levels of triglycerides in...more
Dyslipidemia is caused due to various reasons. Some common reasons are the high level of bad cholesterol, low levels of good cholesterol, high levels of triglycerides in...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Nephrotic syndrome is a type of kidney disorder wherein, the body passes out excess amount of proteins through urine, owing to the damage caused to the tiny clusters of blood vessels in the kidneys. The symptoms include putting on excessive weight as a result of fluid retention, foamy urine and severe swelling around the region of the feet, ankles and eyes.
Common causes behind it:
Minimal change disease (also known as nil disease) leads to the abnormal functioning of the kidne...more
Common causes behind it:
Minimal change disease (also known as nil disease) leads to the abnormal functioning of the kidne...more
Asked for male, 31 years old from Pune
Share
Bookmark
Report
1. For your dq's, you can get operated and tendons can be released instantly. It's a short procedure, not so costly and very effective.
2. For your forefinger pain, I think carpal tunnel syndrome could be the cause. Get your never conduction velocity and electromyography of that upper limb done.
3. Also get yourself checked for diabetes and thyroid, uric acid, rheumatoid arthritis
4. Osteoarthritis is not common in young individuals except post trauma.
2. For your forefinger pain, I think carpal tunnel syndrome could be the cause. Get your never conduction velocity and electromyography of that upper limb done.
3. Also get yourself checked for diabetes and thyroid, uric acid, rheumatoid arthritis
4. Osteoarthritis is not common in young individuals except post trauma.
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
What is Diabetic Nephropathy?
Diabetic nephropathy (Diabetic Kidney Disease) is defined as the progressive damage to the kidneys caused by diabetes. It is characterised by the scarring of the glomeruli in the kidneys due to prolonged diabetes mellitus.
What Causes Diabetic Nephropathy?
Diabetes is a condition characterized by high concentration of blood sugar. Although the cause of Diabetes Nephropathy is not yet well defined, it is likely that the high sugar levels in...more
Diabetic nephropathy (Diabetic Kidney Disease) is defined as the progressive damage to the kidneys caused by diabetes. It is characterised by the scarring of the glomeruli in the kidneys due to prolonged diabetes mellitus.
What Causes Diabetic Nephropathy?
Diabetes is a condition characterized by high concentration of blood sugar. Although the cause of Diabetes Nephropathy is not yet well defined, it is likely that the high sugar levels in...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Contrast-induced nephropathy (CIN) is a serious complication that may arise during angiographic procedures and is elaborated as the impairment of renal function. It is estimated as either a 25% increase in the serum creatinine (SCr) from baseline or a 0.5 mg/dL (44 mol/L) increase in absolute creatinine value within two to three days after intravenous contrast administration of intravascular radiographic contrast material that is not attributable to other causes.
To simplify, contrast-...more
To simplify, contrast-...more
Book appointment with top doctors for Carcinoid treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously