Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Vertebroplasty Tips
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Clinical Fellowship In Pain Management, ...read more
Pain Management Specialist•Hyderabad
Vertebroplasty means shaping the backbone i.e. vertebra for backbone and plasty is related to shape. This is an outpatient procedure done to treat compression fractures of the spinal cord. The backbone is made up of multiple small bones which are stacked one on top of the other with a filling material in between that is known as vertebrae. The stack of bones are held in place by the soft, elastic vertebral material.
Vertebroplasty & similar procedure called kyphoplasty is a non-surgical...more
Vertebroplasty & similar procedure called kyphoplasty is a non-surgical...more
11 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
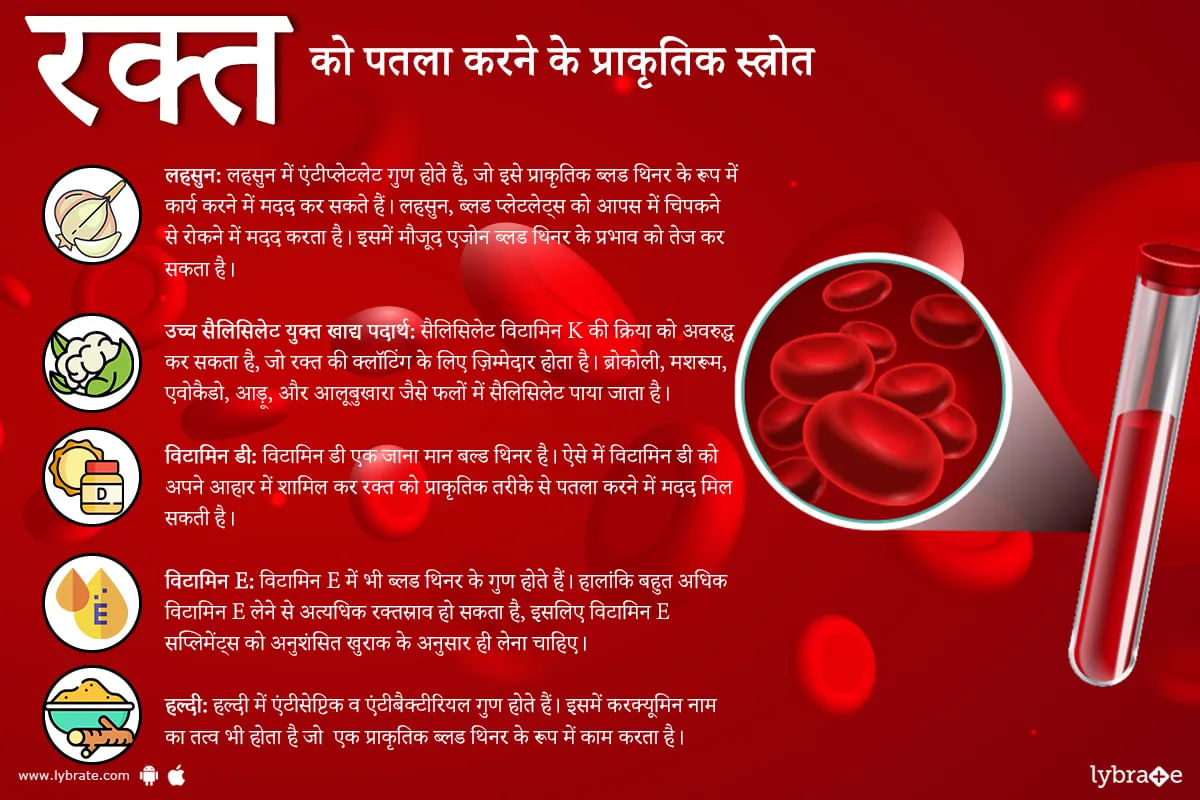
हमारे शरीर का हर अंग प्राकृतिक रूप से बनाए गए नियमों के अनुसार काम करता है। और अगर उसके किसी अंग में कोई बदलाव आ जाए तो स्वास्थ्य संबंधी दिक्कत आ जाती है। ठीक उसी प्रकार हमारे रक्त में भी अगर गाढ़ापन आ जाए या थक्का ना जमे या अधिक जमने लगे तो ये बहुत घातक हो सकता है।पर कुछ दवाओं या बीमारियों के कारण रक्त में ऐसे परिवर्तन आ जाते हैं।ऐसे में आपके मस्तिष्क और हृदय जैसे आवश्यक अंगों की आपूर्ति करने वाली महत्वपूर्ण धमनियों में रक्त के थक्के जमा हो सकते हैं, जिससे संभावित रूप से स्ट्रोक या दिल का दौरा ...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
1. Dr. Adarsh kumar
Https://www. Lybrate. Com/delhi/doctor/dr-adarsh-kumar-ayurveda ;
Bams
17 years experience 300 at clinic 300 online
The doctor has been treating cervical issues, which are a well-known condition in this stressful atmosphere. Dr. Adarsh treats patients with a holistic and spiritual approach, including ayurvedic medications and panchakarma treatments. In 2005, he earned his official education as a bachelor of ayurved...more
150 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
1. Dr. Madu sridhar
Https://www. Lybrate. Com/chennai/doctor/dr-madu-sridhar-orthopedist
Ms in orthopaedics, m. Ch trauma & ortho, diploma in orthopaedics (d. Ortho),
14 years experience 250 at clinic 300 online
He is regarded as a senior clinician with expertise as an orthopaedic doctor. He is a kind hearted experienced physician with extensive experience as an orthopaedic surgeon, paediatric orthopedist, joint replacement surgeon, as wel...more
Https://www. Lybrate. Com/chennai/doctor/dr-madu-sridhar-orthopedist
Ms in orthopaedics, m. Ch trauma & ortho, diploma in orthopaedics (d. Ortho),
14 years experience 250 at clinic 300 online
He is regarded as a senior clinician with expertise as an orthopaedic doctor. He is a kind hearted experienced physician with extensive experience as an orthopaedic surgeon, paediatric orthopedist, joint replacement surgeon, as wel...more
29 people found this helpful
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Rheumatoid Arthritis is an autoimmune condition wherein the body s immune system mistakenly attacks the linings of the joint. This condition affects both sides of the body including the eyes, hands and legs. Unlike the depreciating damage of osteoarthritis, rheumatoid arthritis causes a distressful swelling that consequently leads to bone deformity and even erosion. As such, it is one of the more important characteristics of the condition which distinguishes it from other forms of arthritis. It ...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
MBBS Bachelor of Medicine and Bachelor o...read more
Orthopedic Doctor•Bhubaneswar
Arthritis has often turned out to be a party-pooper for aged people. The worsening pain as one grows older is a concern for many, with more than 10 million official cases filed per year, in India. Hip and knee arthroplasty, in a strict sense, is the surgical reconstruction or replacement of joints that swell with age.
Main types of arthroplasty
Arthroplasty is generally done on people aged sixty or above and those suffering from osteoarthritis, frozen shoulder, joint stiffness, etc....more
Main types of arthroplasty
Arthroplasty is generally done on people aged sixty or above and those suffering from osteoarthritis, frozen shoulder, joint stiffness, etc....more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The physical constitution of a woman s body is complex and must be subject to regular medical check-ups. The reproductive system in women is especially sensitive to many factors. Colposcopy is a surgical procedure that entails an examination of the vulva, vagina, and cervix by using a tool known as the colposcope. This process is performed if unusual results are detected in Pap smear test.
The Pap smear is a medical screening test that helps identify abnormal cervical cells. The doctor ...more
The Pap smear is a medical screening test that helps identify abnormal cervical cells. The doctor ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Arthroscopic Surgery is the most common orthopedic process, which helps in diagnosing and treating joint problems such as in the knee, ankle, shoulder, hip, and elbow. The term "arthroscopy" is a combination of two Greek terms - 'arthro' means joint and scope means look. Arthroscopic surgery helps examine the inside of a joint. During the surgery, a small camera and optical fiber are inserted inside the affected joint through incisions. Obtained images are then projected onto a display screen...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Rotator cuff constitutes the muscles and tendons that hold the shoulder in position. It is a crucial component of the shoulder as it helps in lifting the arm to complete any task. Repetitive actions, deterioration with age or an outstretched hand can lead to a sudden tear.
4 Important Things To Know About Rotator Cuff Repair
An injured rotator cuff can be repaired surgically. Arthroscopy and open surgery are among the techniques used to fix a tear of the rotator cuff surgically. An ...more
4 Important Things To Know About Rotator Cuff Repair
An injured rotator cuff can be repaired surgically. Arthroscopy and open surgery are among the techniques used to fix a tear of the rotator cuff surgically. An ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Shoulder arthroscopy is done using a device containing a tiny camera known as the arthroscope. This is why it is termed as shoulder arthroscopy. It is used to examine tissues around the shoulder joint. If the examination reveals damage, the surgeon uses the arthroscope to treat the area by a cuff/labral repair. The surgeon inserts the arthroscope through a small incision on the shoulder.
Why Is Shoulder Arthroscopy Required?
There are a number of muscles and tendons in the shou...more
Why Is Shoulder Arthroscopy Required?
There are a number of muscles and tendons in the shou...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Arthroscopy has brought about a revolutionary change in the way doctors visualize, diagnose, and then treat problems in knee joints, elbow joints, shoulder joints, ankle joints, and hip joints. For performing Arthroscopy, the doctor makes an incision on the skin of the patient and inserts a slender instrument through the incision. The instrument contains a small lens along with a lighting system to illuminate and magnify structures inside the joint. This instrument is known as an arthroscope, an...more
Book appointment with top doctors for Vertebroplasty treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously