Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Vaginal Itching Tips
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
To have a healthy vagina a woman needs to maintain a certain level of ph in the vagina. There are so many factors which can play a key role in the maintenance of the ph level and the factors can be either environmental or natural; these factors could lead a woman to experience various problems like burning, itching and change in the discharge from the vagina.
;
There are certain steps which you can follow to keep your vaginal ph level balanced and to do thi...more
453 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
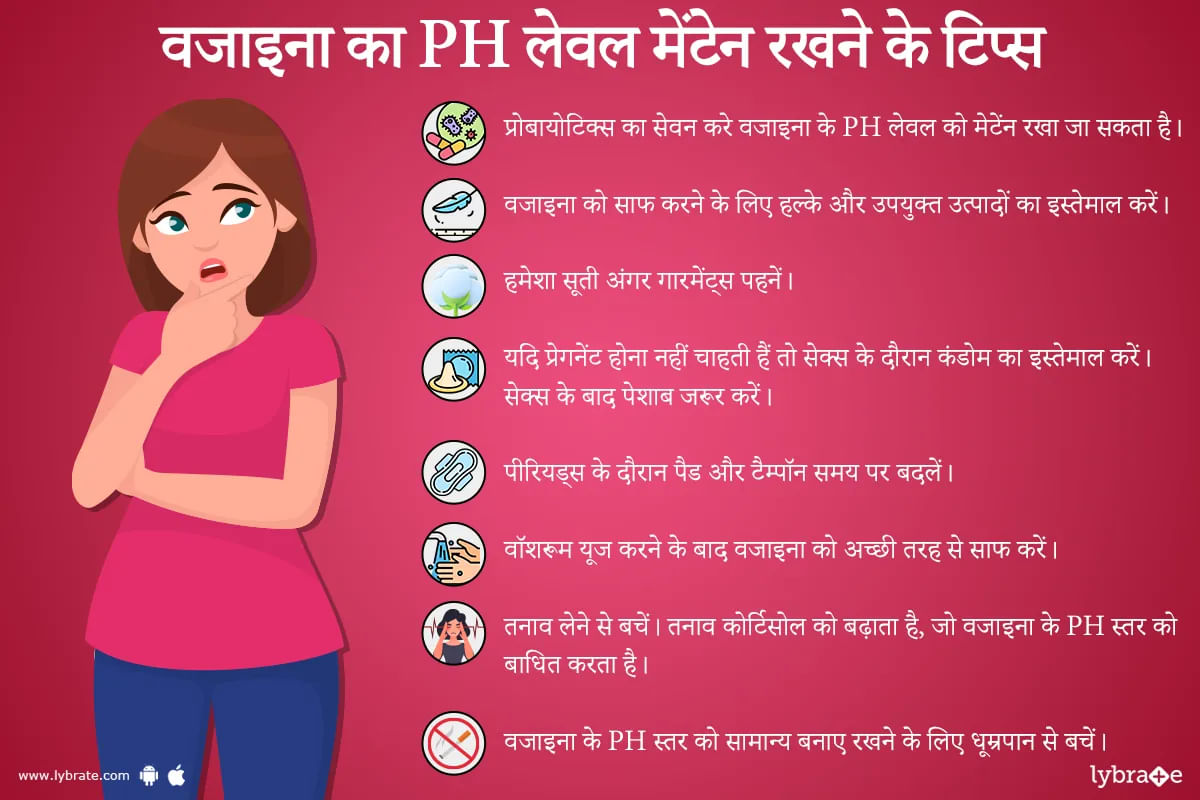
शरीर के स्वास्थ्य का ध्यान रखने के साथ हमारे लिए अपनी सेक्सुअल हेल्थ का भी ध्यान रखना ज़रूरी है। महिलाओं को अपनी योनि को साफ और स्वस्थ् रखने के लिए उसका पीएच बैलेंस सही स्तर पर बनाए रखना आवश्यक है। प्राकृतिक तौर पर योनि का आंतरिक वातावरण अम्लीय यानी एसिडिक होता है जिसका सामान्य पीएच स्तर 4.5 से कम होता है।
पीएच एक ऐसा पैमाना है जो किसी भी पदार्थ के एसिडिक या एल्कलाइन स्तर को नापने के लिए इस्तेमाल किया जाता है।यदि आप ऐसी उम्र में जब आपका शरीर प्रजनन कर सकता है तो आपकी योनि का पीएच 3.8 औ...more
पीएच एक ऐसा पैमाना है जो किसी भी पदार्थ के एसिडिक या एल्कलाइन स्तर को नापने के लिए इस्तेमाल किया जाता है।यदि आप ऐसी उम्र में जब आपका शरीर प्रजनन कर सकता है तो आपकी योनि का पीएच 3.8 औ...more
1870 people found this helpful
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Burning and itching, along with an unpleasant odor, are common symptoms which indicate a vaginal infection. Vaginal infections, also known as vaginitis are common in women. All women experience some form of it during their lifetime. A vaginal infection may occur when the normal vaginal balance is affected. The balance may be disturbed by factors such as douches, changes in hormone level, certain antibiotic medicines, pregnancy and vaginal intercourse. There are several different types of vaginal...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Trichomonas Vaginalis, a virus, which affects almost 7.4 million men and women each year. This virus can cause a sexually transmitted disease upon contact with a person who may be carrying the same. This condition is more common in women than it is in men and causes a variety of symptoms. Let us learn more about this infection.
Symptoms
This disease does not have any obvious symptoms until the problem becomes pretty severe. The symptoms for men include irritation inside the pen...more
Symptoms
This disease does not have any obvious symptoms until the problem becomes pretty severe. The symptoms for men include irritation inside the pen...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Trichomonas Vaginalis, a virus, which affects almost 7.4 million men and women each year. This virus can cause a sexually transmitted disease upon contact with a person who may be carrying the same. This condition is more common in women than it is in men and causes a variety of symptoms. Let us learn more about this infection.
Symptoms
This disease does not have any obvious symptoms until the problem becomes pretty severe. The symptoms for men include irritation inside the pen...more
Symptoms
This disease does not have any obvious symptoms until the problem becomes pretty severe. The symptoms for men include irritation inside the pen...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Trichomonas Vaginalis, a virus, which affects almost 7.4 million men and women each year. This virus can cause a sexually transmitted disease upon contact with a person who may be carrying the same. This condition is more common in women than it is in men and causes a variety of symptoms. Let us learn more about this infection.
Symptoms
This disease does not have any obvious symptoms until the problem becomes pretty severe. The symptoms for men include irritation inside the penis, d...more
Symptoms
This disease does not have any obvious symptoms until the problem becomes pretty severe. The symptoms for men include irritation inside the penis, d...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Trichomonas Vaginalis, a virus, which affects almost 7.4 million men and women each year. This virus can cause a sexually transmitted disease upon contact with a person who may be carrying the same. This condition is more common in women than it is in men and causes a variety of symptoms. Let us learn more about this infection.
Symptoms
This disease does not have any obvious symptoms until the problem becomes pretty severe. The symptoms for men include irritation inside the penis, d...more
Symptoms
This disease does not have any obvious symptoms until the problem becomes pretty severe. The symptoms for men include irritation inside the penis, d...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Vaginal itching is a condition which occurs when the vagina comes in contact with irritants or because of a vaginal infection. Menopause may also lead to conditions that trigger itching in the vagina. In some cases, sexually transmitted diseases and skin allergies also lead to vaginal itching. The conditions in itself is not a major cause of concern, however, one should consult a doctor to treat the underlying condition, if any.
Causes-
The main component of vaginal itching is ...more
Causes-
The main component of vaginal itching is ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Trichomonas Vaginalis, a virus, which affects almost 7.4 million men and women each year. This virus can cause a sexually transmitted disease upon contact with a person who may be carrying the same. This condition is more common in women than it is in men and causes a variety of symptoms. Let us learn more about this infection.
Symptoms
This disease does not have any obvious symptoms until the problem becomes pretty severe. The symptoms for men include irritation inside the pen...more
Symptoms
This disease does not have any obvious symptoms until the problem becomes pretty severe. The symptoms for men include irritation inside the pen...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Vaginal itching is a condition which occurs when the vagina comes in contact with irritants or because of a vaginal infection. Menopause may also lead to conditions that trigger itching in the vagina. In some cases, sexually transmitted diseases and skin allergies also lead to vaginal itching. The conditions in itself is not a major cause of concern, however, one should consult a doctor to treat the underlying condition, if any.
Causes-
The main component of vaginal itching is ...more
Causes-
The main component of vaginal itching is ...more
Book appointment with top doctors for Vaginal Itching treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously