Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Vaginal Infection Tips
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
As a pregnant woman, maintaining good hygiene is crucial for the health and well-being of both you and your baby. Taking care of your intimate area is an important part of this. From increased vaginal discharge to the risk of infections, pregnancy can bring about many changes to your body. That's why we've put together this guide on how to clean your private parts during pregnancy. Follow these tips to keep your intimate area clean, healthy, and comfortable throughout your pr...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
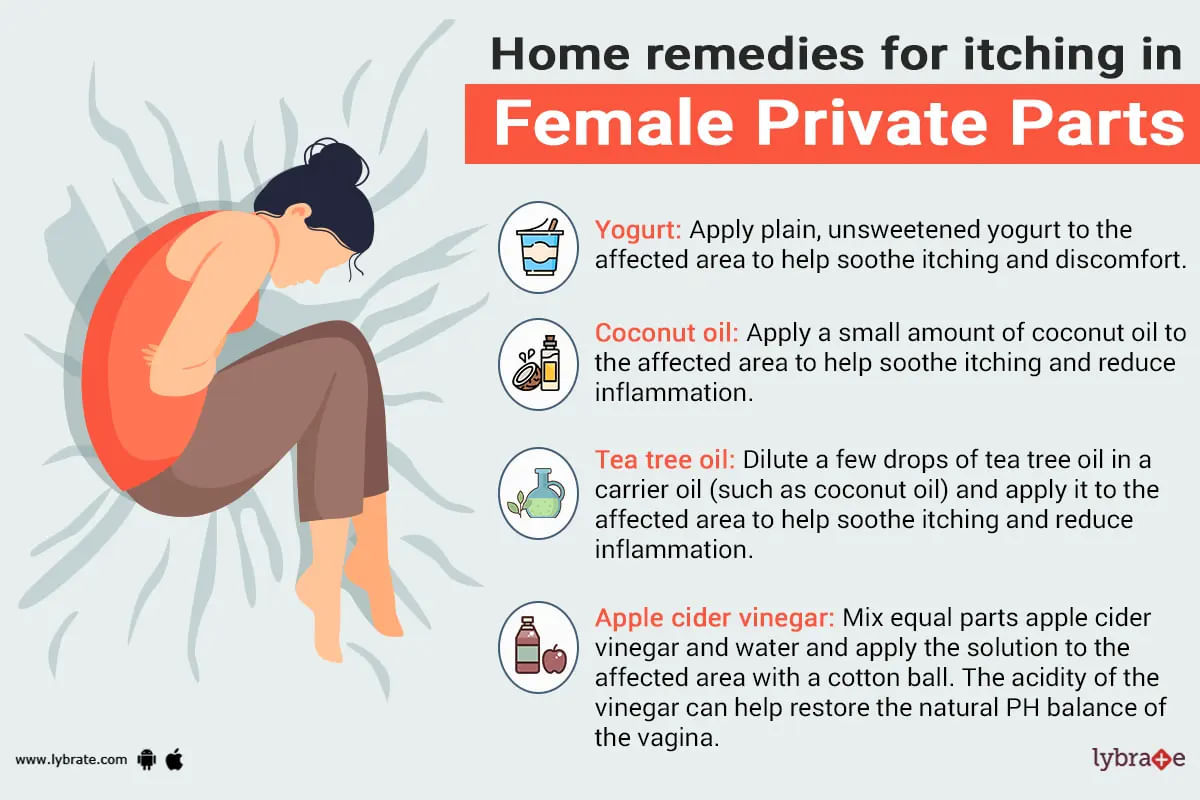
The itching in the private parts of females is an irritation that makes them feel uncomfortable. Itching in the private parts of the female is the symbol of the infection in the vagina, yeast infection, itching in the vulvar areas of the female. Mostly women feel the itching in the private parts during the menstrual cycle or during the menopausal transition due to some of the fluctuations in the estrogen level. They should visit the doctor immediately if they are having the genital red...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
To have a healthy vagina a woman needs to maintain a certain level of ph in the vagina. There are so many factors which can play a key role in the maintenance of the ph level and the factors can be either environmental or natural; these factors could lead a woman to experience various problems like burning, itching and change in the discharge from the vagina.
;
There are certain steps which you can follow to keep your vaginal ph level balanced and to do thi...more
453 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Gynaecologist•Hyderabad
Vagina is a part of female's genitals. This starts as an opening which is known as introitus or labia's inner part. A woman s vagina ends at the uterus' opening, known as the cervix.
The health of the vagina of a woman could be regarded as the most important part of her overall health. The vagina affects a lot of activities going on in a female's body and its good condition is responsible for a woman's total body welfare.
;
If there is any sort of problem w...more
The health of the vagina of a woman could be regarded as the most important part of her overall health. The vagina affects a lot of activities going on in a female's body and its good condition is responsible for a woman's total body welfare.
;
If there is any sort of problem w...more
409 people found this helpful
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Vaginal Candidiasis is a condition that is brought on by an infection in the vaginal area of the patient. This affects women as a rule. It is triggered by the presence of a fungus known as Candida Albicans which is usually present in the vagina. While it is harmless when it remains in its dormant state, there are many conditions in which it gets activated and causes an infection which can cause great pain and discomfort to the patient. Itching and discharge from the patient s vagina are normal s...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The urinary system in both men and women are susceptible to infections and many other internal disorders. Although many of the disorders may be caused due to underlying diseases or hereditary causes, many others may be caused due to bad lifestyle habits as well as personal hygiene issues. Personal hygiene issues will not only lead to infections, but if left unchanged, may cause more serious problems such as tumors over time. However, with the help of some basic tips and following some daily rout...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
When the vagina hurts and contracts involuntarily during the insertion of a foreign object, this is known as vaginismus. The muscles in the vagina tighten around the foreign object and causes pain, discomfort and a burning sensation. It is basically an involuntary spasm occurring in the vaginal muscles which makes a penetration in the vagina almost impossible. Vaginismus works in a reflex mechanism, just like the eye shuts automatically when an object comes towards it.
Symptoms -
more
Symptoms -
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
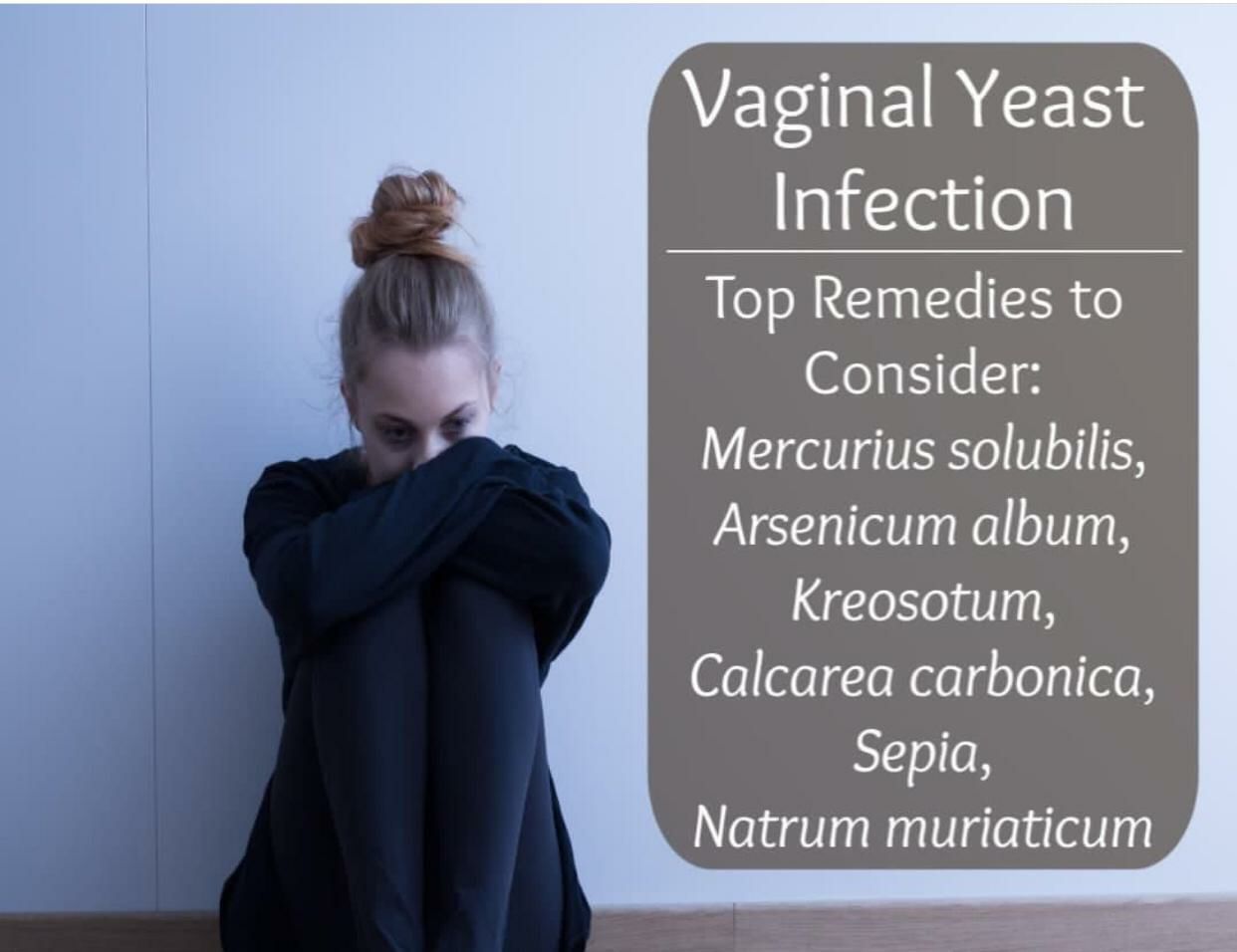
A yeast infection in the vagina is characterized by itchiness, irritation in the vulva and vaginal discharge. Inflammation occurs in the tissues of the vagina, leading to constant itching. Though this is not a sexually transmitted infection, the fungus may spread via oral sex where the mouth and genitals come in contact.
The symptoms of vaginal yeast infection are:
1. You may experience a painful sensation during sexual intercourse
2. An itching sensation in the vagina...more
The symptoms of vaginal yeast infection are:
1. You may experience a painful sensation during sexual intercourse
2. An itching sensation in the vagina...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
In a healthy individual, there are millions of microorganisms in different parts of the body which are essential for normal functioning of that particular organ. Be it the mouth or the gut or the reproductive tract, there are normally organisms. These form part of the normal flora of that body part. It is when there is an imbalance between the good and bad bacteria, where the bad ones take over, then there is a problem. This results in an infection, which manifests with symptoms and requires tre...more
Book appointment with top doctors for Vaginal Infection treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously