Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Urinary Incontinence Tips
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
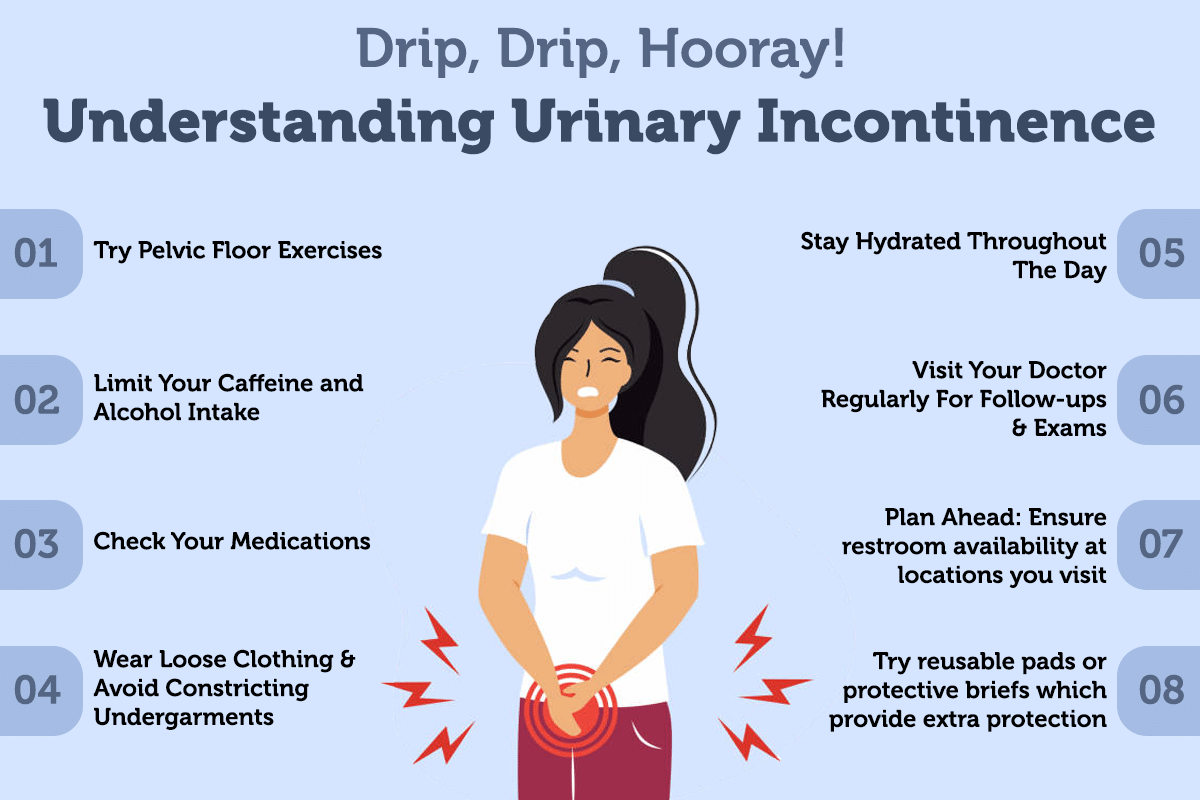
What is urinary incontinence?
Urinary incontinence is the unintentional loss of urine. It is a common problem among all age groups, though it occurs more frequently in older people, and women are affected more than men.
It can be caused by physical problems such as weak bladder or neurological disorders, or it can be the result of certain lifestyle habits and conditions. Treatment for urinary incontinence will depend on the type and severity of your condition, but ma...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Pee- gasm is currently considered as a rising situation in the case of women. During this, the women experiences delay in the release of urine while urinating and when the urine is released they experience an orgasm like feeling. Experiencing this pee gasm is a totally normal phenomenon and it is not a matter about which we should be concerned. ;
Majority of the women who experience pee-gasm consider it as a problem or malfunction of their body and they do...more
939 people found this helpful
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
While certain health conditions cause physical trauma, there are conditions that cause mental trauma as well. One such problem is urinary incontinence that causes embarrassment in the sufferer. Urinary incontinence is a clinical condition where there is a loss of bladder control which invariably leads to accidental leakage of urine. An individual suffering from this condition may feel an urgent need to pass urine right before passing a significant amount of urine.
The severity of the co...more
The severity of the co...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Urinary incontinence refers to a condition where an individual loses control of the bladder. UI is a common, distressing problem, which can largely affect your quality of life. A number of factors could be causing urinary incontinence stress, obesity, or simply coughing/sneezing. The chances of developing UI increase with age.
PRP for Urinary Incontinence -
Platelet Rich Plasma or PRP treatment offers viable, safe management for urinary incontinence in people. It belongs to the br...more
PRP for Urinary Incontinence -
Platelet Rich Plasma or PRP treatment offers viable, safe management for urinary incontinence in people. It belongs to the br...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
A common problem that is not restricted to older people is urinary incontinence, and many are not aware that behavioral strategies play an important role in controlling urinary incontinence. These include alterations in the diet, urinary habits, and lifestyle changes.
The required changes and alterations to be made are entirely dependent on the individual conditions of the patient. However, these are the most common tips as far as the diet to overcome urinary incontinence is concerned:<...more
The required changes and alterations to be made are entirely dependent on the individual conditions of the patient. However, these are the most common tips as far as the diet to overcome urinary incontinence is concerned:<...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Anal fistulas or fistula-in-ano generally cause discomfort due pus or watery discharges and sometimes pain. This is a condition where a nodular swelling appears in area surrounding the anal opening. Intermittent pus discharged is noticed from this nodular swelling. Instead of a nodular swelling; there might be simply an opening in this region. An anal abscess is one of the most common causes for this condition. Here are seven things you should know about these anal fistulas:
It is curab...more
It is curab...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
What is Urinary Incontinence?
Urinary incontinence is the unintentional discharge of urine. Urinary incontinence may manifest itself in different forms. This may include an overactive bladder, mixed or transient incontinence.
Causes of Incontinence-
Incontinence may be a result of weakened or damaged pelvic floor muscles or an obstruction in the bladder. It most often occurs in women after pregnancy and menopause. Rapid weight gain or a genetic pre-disposition can increase ...more
Urinary incontinence is the unintentional discharge of urine. Urinary incontinence may manifest itself in different forms. This may include an overactive bladder, mixed or transient incontinence.
Causes of Incontinence-
Incontinence may be a result of weakened or damaged pelvic floor muscles or an obstruction in the bladder. It most often occurs in women after pregnancy and menopause. Rapid weight gain or a genetic pre-disposition can increase ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Urinary incontinence refers to the inability to control bladder movements. While it does not affect the person s health, it can be an embarrassing condition. The severity of this condition can range from passing small amounts of urine every time you sneeze or cough, to getting a sudden strong urge to urinate without the time to get to a toilet. Urinary incontinence is not a disease by itself but rather is a sign of another underlying condition. It may be caused as a result of childbirth, age, me...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
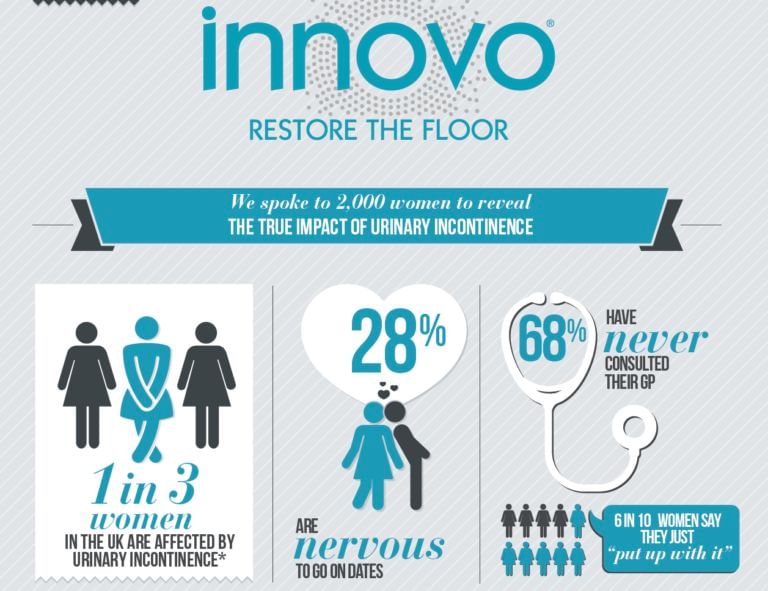
This device was FDA approved late last year as the first transcutaneous stimulator with such an indication.
It delivers electric current through the body toward muscles that control the pelvic floor, which in turn can help maintain continence in both men and women.
The technology provides a non-invasive option that, in a clinical trial, demonstrated that 87% of individuals were dry or nearly so after a three-month treatment. 80% of the women studied had results after only a mo...more
It delivers electric current through the body toward muscles that control the pelvic floor, which in turn can help maintain continence in both men and women.
The technology provides a non-invasive option that, in a clinical trial, demonstrated that 87% of individuals were dry or nearly so after a three-month treatment. 80% of the women studied had results after only a mo...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Involuntary and sudden urine loss in women is termed as urinary incontinence. Some of the contributory factors to urinary incontinence are menopause, pregnancy and childbirth.
Types:
There are seven types of urinary incontinence.
Stress incontinence: If normal physical movements like sneezing, coughing and exercising cause small amounts of urine to leak out, it is called 'stress incontinence'.
Urge incontinence: If large amounts of urine leak out during unexpected and a...more
Types:
There are seven types of urinary incontinence.
Stress incontinence: If normal physical movements like sneezing, coughing and exercising cause small amounts of urine to leak out, it is called 'stress incontinence'.
Urge incontinence: If large amounts of urine leak out during unexpected and a...more
Book appointment with top doctors for Urinary Incontinence treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously