Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Thalassemia Tips
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Bachelor of Ayurveda, Medicine and Surge...read more
Ayurvedic Doctor•Lakhimpur Kheri
Thalassemia is a grave blood disorder. That is why people who have been diagnosed with it need to be extra careful with how they live their lives. The focus is on always making healthy lifestyle choices. This improves the quality of their lives, helps manage the disorder and will have a less detrimental impact on their lifespan.
Keep the illness under control - With proper care and intervention, thalassemia can be managed efficiently. To continue being healthy, thalassemia patients must...more
Keep the illness under control - With proper care and intervention, thalassemia can be managed efficiently. To continue being healthy, thalassemia patients must...more
477 people found this helpful
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Bachelor of Ayurveda, Medicine and Surge...read more
Ayurvedic Doctor•Lakhimpur Kheri
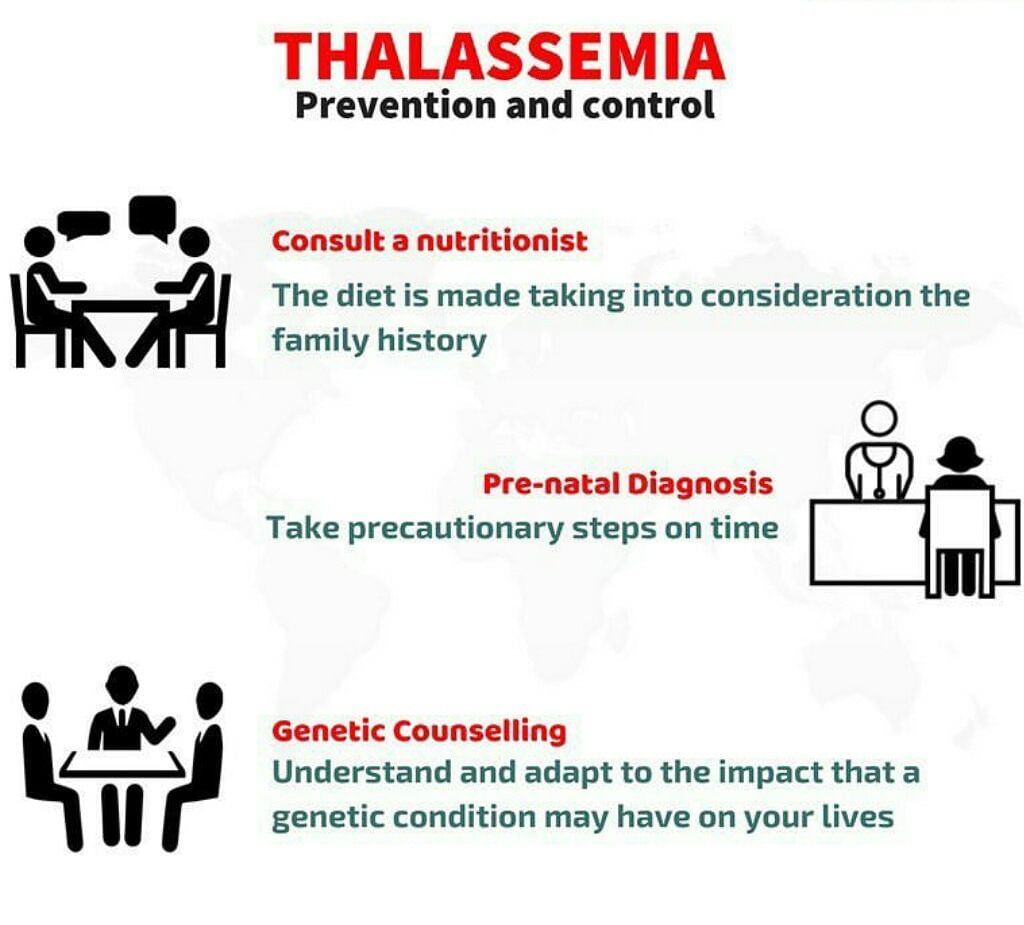
Thalassaemia is one of the most difficult hereditary diseases to live with. Even though there is no cure, parents can prevent their child from being born with this terrible disease if they are careful. Thalassemia is a blood illness. It is an inherited disorder. If even one parent is a carrier of thalassemia, the child will be born with this blood disorder. Our blood contains haemoglobin - a protein molecule. It carries oxygen to all parts of the body. But some people are born with an unnatural ...more
447 people found this helpful
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Thalassemia is a blood illness that destroys haemoglobin in the blood. Unless managed properly, thalassemia can be fatal. Keeping the disease under control involves not just blood transfusion, folate intake and chelation therapy but also diet. What the patients eat has an impact on how well their bodies will respond to treatment.
Diet for thalassemia patients
Thalassemia can trigger nutritional deficiency illnesses, haemolytic anaemia, diabetes and iron build-up (because of regular ...more
Diet for thalassemia patients
Thalassemia can trigger nutritional deficiency illnesses, haemolytic anaemia, diabetes and iron build-up (because of regular ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Thalassaemia is one of the most difficult hereditary diseases to live with. Even though there is no cure, parents can prevent their child from being born with this terrible disease if they are careful.
However, preventing the spread of disease in the world has proven difficult due to the lack of proper awareness about the condition. This is why the World Health Organization established May 8th as World Thalassaemia Day.
Importance of World Thalassaemia Day
8th May is d...more
However, preventing the spread of disease in the world has proven difficult due to the lack of proper awareness about the condition. This is why the World Health Organization established May 8th as World Thalassaemia Day.
Importance of World Thalassaemia Day
8th May is d...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Multi Speciality•Mumbai
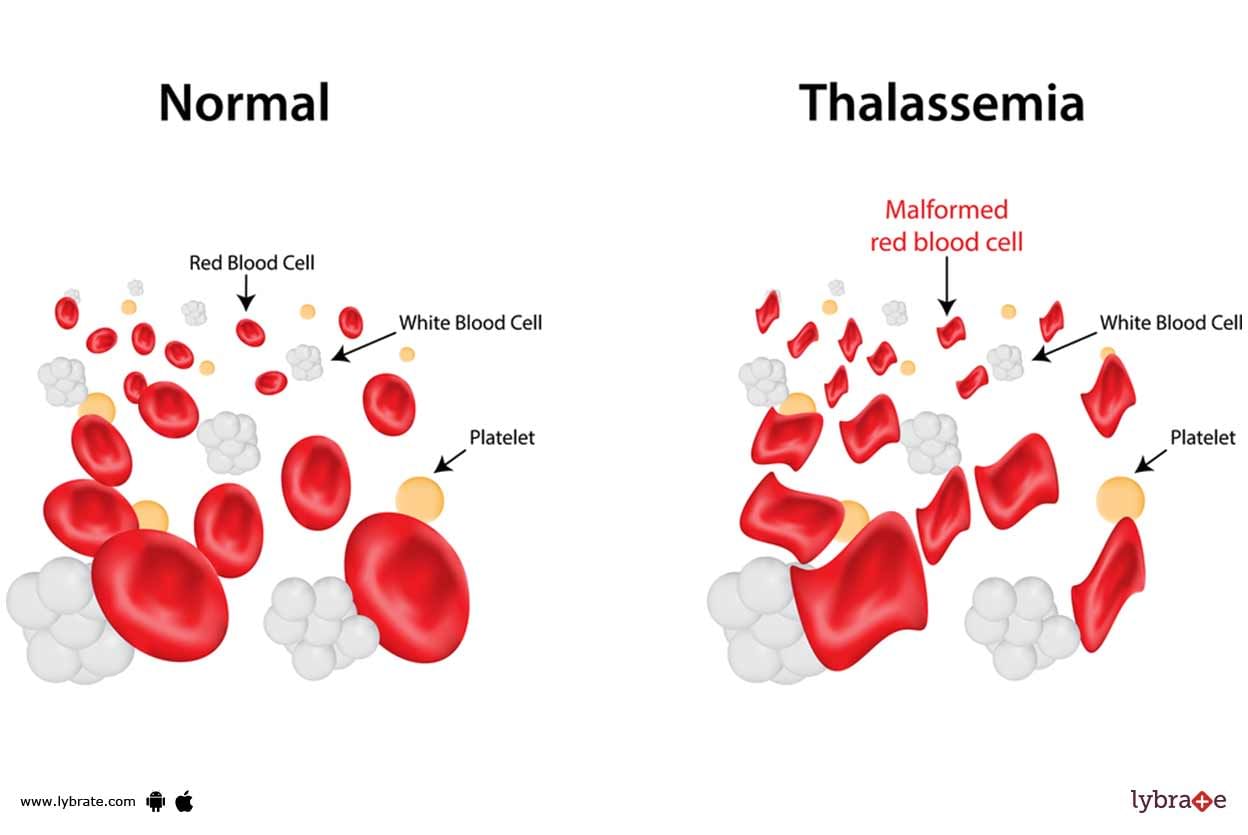
Thalassemia is a genetic (i.e., passed from parents to children through genes) blood disorder. People with Thalassemia disease are not able to make enough hemoglobin, which causes severe anemia. Hemoglobin is found in red blood cells and carries oxygen to all parts of the body. When there is not enough hemoglobin in the red blood cells, oxygen cannot get to all parts of the body. Organs then become starved for oxygen and are unable to function properly.
There are two types of Thalassemi...more
There are two types of Thalassemi...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Thalassemia is a genetic (i.e., passed from parents to children through genes) blood disorder. People with Thalassemia disease are not able to make enough hemoglobin, which causes severe anemia. Hemoglobin is found in red blood cells and carries oxygen to all parts of the body. When there is not enough hemoglobin in the red blood cells, oxygen cannot get to all parts of the body. Organs then become starved for oxygen and are unable to function properly.
There are two types of Thalassemi...more
There are two types of Thalassemi...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Bachelor of Ayurveda, Medicine and Surge...read more
Ayurvedic Doctor•Lakhimpur Kheri
थैलासीमिया एक प्रकार का ब्लड डिसऑर्डर है, जो आपके शरीर में असामान्य हीमोग्लोबिन और रेड ब्लड सेल्स के उत्पादन के लिए जिम्मेदार होती है. थैलासीमिया विभिन्न प्रकार के होते हैं जैसे अल्फा-थैलासीमिया, बीटा-थैलासीमिया इंटरमीडिया, कोली एनीमिया और मैडिटरेनियन एनीमिया. हीमोग्लोबिन ऑक्सीजन ले जाने में रेड ब्लड सेल्स की सहायता करता है. रेड ब्लड सेल्स और हीमोग्लोबिन में कमी के कारण एनीमिया हो सकता है. इसके परिणामस्वरूप कमजोरी और थकावट महसूस करते हैं. इसके अलावा, आप पेट में सूजन, डार्क यूरिन या पीले रंग की ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
M.Sc. in Dietetics and Food Service Mana...read more
Dietitian/Nutritionist•Mumbai
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
Thalassemia is a type of a disease, resulting in the abnormal production of hemoglobin in the blood. Hemoglobin stimulates oxygen circulation all over the body. Therefore, a dip in the hemoglobin count can lead to anemia, a disease inducing weakness as well as fatigue. Acute anemia can take a toll on the organs and ultimately cause death.
Severe thalassemia in children yields symptoms, such as dark urine, abdominal swelling, slow growth, jaundice, a pale appearance and deformed skull bo...more
Severe thalassemia in children yields symptoms, such as dark urine, abdominal swelling, slow growth, jaundice, a pale appearance and deformed skull bo...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
Thalassemia is a genetic (which is passed from parents to children through genes) blood disorder. People with Thalassemia disease are not able to make enough hemoglobin, which causes severe anemia. Hemoglobin is found in red blood cells and carries oxygen to all parts of the body. When there is not enough hemoglobin in the red blood cells, oxygen cannot get to all parts of the body. Organs then become starved for oxygen and are unable to function properly.
There are two types of Thalass...more
There are two types of Thalass...more
Book appointment with top doctors for Thalassemia treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously