Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTips
Supraventricular Tachycardia Tips
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Dermatologist•Delhi
Hypertension is a killer disease whose symptoms develop late when the damage is in advanced stages. Hypertensive Retinopathy is one such disease.
It damages the retina of eyes. Since retina is responsible for vision formation, Hypertensive Retinopathy can result in loss of vision. It is of grave concern that in most cases, Hypertensive Retinopathy is diagnosed later.
This is due to the fact that there are often no symptoms in the early stages of the disease. In some cases, wher...more
It damages the retina of eyes. Since retina is responsible for vision formation, Hypertensive Retinopathy can result in loss of vision. It is of grave concern that in most cases, Hypertensive Retinopathy is diagnosed later.
This is due to the fact that there are often no symptoms in the early stages of the disease. In some cases, wher...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
We all know about the heartbeat, which is produced by the opening and closing of the valves in the heart, which in turn controls our blood flow. There is a regular pattern to this beat, and when, due to various reasons, it becomes irregular, it is known as arrhythmia. Atrial fibrillation, known shortly as AFib, is one of the common types of arrhythmia.
Why AFib: The heart has an electrical impulse system, which controls the opening/closing of its valves. Due to various changes, be it li...more
Why AFib: The heart has an electrical impulse system, which controls the opening/closing of its valves. Due to various changes, be it li...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
As the nomenclature appears to indicate, Arrhythmia is a condition where the heartbeat of the affected person does not conform to the rhythm it is designed for. But there are cases of Arrhythmia where the normal heartbeat is available as well. The underlying causes of the condition can be many, including a disorder in the coronary artery and the person having suffered a heart attack or undergone heart surgery. The irregular heartbeat is medically referred to as fibrillation.
The fact is...more
The fact is...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Cardiomyopathy is a heart muscle disease that makes it difficult for your heart to supply blood to the rest of the body. This disease affects the heart s size, shape and structure, hence resulting in heart failure. Some of the common types of cardiomyopathies are
Hypertrophic cardiomyopathy
Restrictive cardiomyopathy
dilated cardiomyopathy.
The disease is generally inherited and some family members might get more affected than others, while others may not suffer at all or co...more
Hypertrophic cardiomyopathy
Restrictive cardiomyopathy
dilated cardiomyopathy.
The disease is generally inherited and some family members might get more affected than others, while others may not suffer at all or co...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Pericardial effusion is the excess fluid between the heart and sac surrounding the heart. The fluid keeps the heart moving in the sac. The excess fluid can cause a problem in the workings of the heart and may lead to death. The space between two layers of sac usually contain 2-3 tablespoons of clear liquid. But pericardial effusion can affect the heart beats and make it weaker.
Causes
The leading cause of the pericardial effusion is pericarditis. In this condition, the layered...more
Causes
The leading cause of the pericardial effusion is pericarditis. In this condition, the layered...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Cardiomyopathy is a heart muscle disease that makes it difficult for your heart to supply blood to the rest of the body. This disease affects the heart s size, shape and structure, hence resulting in heart failure. Some of the common types of cardiomyopathies are
Hypertrophic cardiomyopathy
Restrictive cardiomyopathy
dilated cardiomyopathy.
The disease is generally inherited and some family members might get more affected than others, while others may not suffer at all or co...more
Hypertrophic cardiomyopathy
Restrictive cardiomyopathy
dilated cardiomyopathy.
The disease is generally inherited and some family members might get more affected than others, while others may not suffer at all or co...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Cardiomyopathy is serious heart disease. It is a disease associated with heart muscle or myocardium. In this disease, the heart muscles get weak and fail to pump blood to the organs of the body. It has several categories. The categorization depends upon the range of factors. In this disease, irregular heartbeat is observed. These irregularities can lead to heart failure or attack or can trigger problems in the valves. It is important to take care of your heart to avoid such a condition. It is al...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Heart ablation or cardiac ablation is a procedure done to treat irregular heartbeats or arrhythmias. It is performed by an interventional cardiologist, a doctor who specialises in doing procedures for heart problems and it involves threading long wires called catheters through a blood vessel into your heart. The irregular heartbeat is treated by delivering an electrical pulse using electrodes to specific areas of your heart.
Arrhythmias
A normal heart beats at a steady rate, but som...more
Arrhythmias
A normal heart beats at a steady rate, but som...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
MBBS, MD - Paediatrics, FNB Pediatric Ca...read more
Pediatric Cardiologist•Delhi
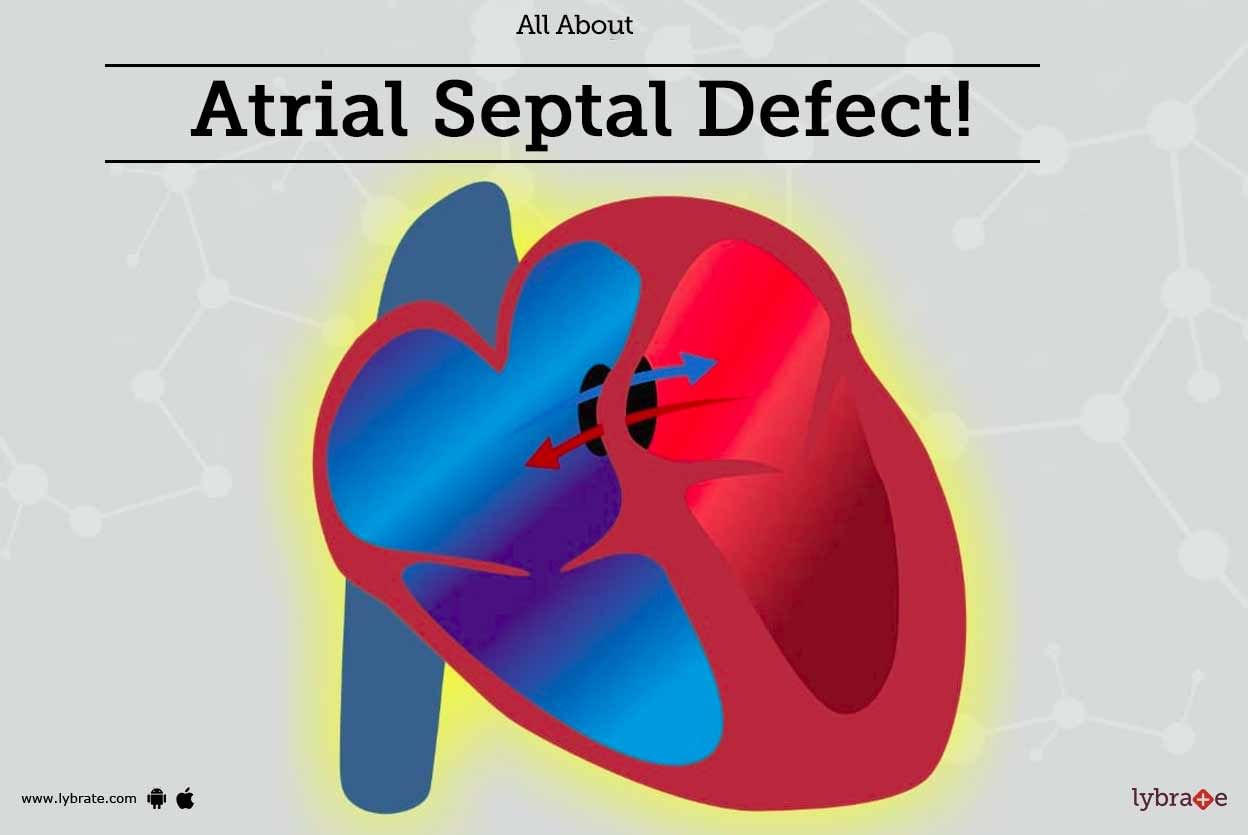
An Atrial Septal Defect is present at birth (congenital heart disease). The condition refers to a hole in the septum or walls (atrial septum) that separate the heart s upper chambers atria.
The heart of the fetus develops during pregnancy. Normally, there are several openings in the septum dividing the atria, which close during pregnancy or soon after birth. However, a hole is formed if one of the openings does not close, leading to atrial septal defect.
Due to a hole in the heart, blo...more
The heart of the fetus develops during pregnancy. Normally, there are several openings in the septum dividing the atria, which close during pregnancy or soon after birth. However, a hole is formed if one of the openings does not close, leading to atrial septal defect.
Due to a hole in the heart, blo...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Pulmonary edema is a disorder wherein fluid accumulates in the lungs leading to lack of oxygen in the body. The usual cause of pulmonary edema is congestive heart failure (the muscles of the heart are unable to pump blood). In this disorder, the heart has to work extra hard to pump blood, so this adds extra pressure on the blood vessels that are present in the lungs. In a bid to relieve this added pressure, fluid is released into the lungs by the blood vessels.
The function of your lung...more
The function of your lung...more
Book appointment with top doctors for Supraventricular Tachycardia treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously