Get the App
For Doctors
Login/Sign-up
Health Feed
Find Doctors
Health Packages
AllQ&AsTips
Splinting Tips
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
The shin is the frontal part of the lower leg and runs from slightly below the knee almost all the way to the foot. This area takes a lot of stress during movements such as walking and running and most forms of exercises of the lower body. Any other form of movement where the weight of the upper body has to be transferred to the feet also involves the shin. Thus repeated stresses may sometimes take their toll resulting in shin splints which can be quite painful.
What exactly are shin sp...more
What exactly are shin sp...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
MBBS Bachelor of Medicine and Bachelor o...read more
Orthopedic Doctor•Bhubaneswar
Shin splints' is a condition, which is characterized by pain in the shin bone, the bone that is present in front of the leg. Shin splints tend to occur quite frequently in runners and dancers as their activities tend to stress the shin bone.
Causes: When excess force is applied to the shinbone, it may result in swelling of the muscles, causing pain and inflammation. It may also occur from stress reactions to fractures in the bone. Cracks tend to develop due to constant application of fo...more
Causes: When excess force is applied to the shinbone, it may result in swelling of the muscles, causing pain and inflammation. It may also occur from stress reactions to fractures in the bone. Cracks tend to develop due to constant application of fo...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
Shin splints' is a condition, which is characterized by pain in the shin bone, the bone that is present in front of the leg. Shin splints tend to occur quite frequently in runners and dancers as their activities tend to stress the shin bone.
Causes
When excess force is applied to the shinbone, it may result in swelling of the muscles, causing pain and inflammation. It may also occur from stress reactions to fractures in the bone. Cracks tend to develop due to constant applicati...more
Causes
When excess force is applied to the shinbone, it may result in swelling of the muscles, causing pain and inflammation. It may also occur from stress reactions to fractures in the bone. Cracks tend to develop due to constant applicati...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
Shin splints' is a condition, which is characterized by pain in the shin bone, the bone that is present in front of the leg. Shin splints tend to occur quite frequently in runners and dancers as their activities tend to stress the shin bone.
Causes
When excess force is applied to the shinbone, it may result in swelling of the muscles, causing pain and inflammation. It may also occur from stress reactions to fractures in the bone. Cracks tend to develop due to constant appl...more
Causes
When excess force is applied to the shinbone, it may result in swelling of the muscles, causing pain and inflammation. It may also occur from stress reactions to fractures in the bone. Cracks tend to develop due to constant appl...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
Shin splints' is a condition, which is characterized by pain in the shin bone, the bone that is present in front of the leg. Shin splints tend to occur quite frequently in runners and dancers as their activities tend to stress the shin bone.
Causes
When excess force is applied to the shinbone, it may result in swelling of the muscles, causing pain and inflammation. It may also occur from stress reactions to fractures in the bone. Cracks tend to develop due to constant applicati...more
Causes
When excess force is applied to the shinbone, it may result in swelling of the muscles, causing pain and inflammation. It may also occur from stress reactions to fractures in the bone. Cracks tend to develop due to constant applicati...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
Shin splints' is a condition, which is characterized by pain in the shin bone, the bone that is present in front of the leg. Shin splints tend to occur quite frequently in runners and dancers as their activities tend to stress the shin bone.
Causes: When excess force is applied to the shinbone, it may result in swelling of the muscles, causing pain and inflammation. It may also occur from stress reactions to fractures in the bone. Cracks tend to develop due to constant application of fo...more
Causes: When excess force is applied to the shinbone, it may result in swelling of the muscles, causing pain and inflammation. It may also occur from stress reactions to fractures in the bone. Cracks tend to develop due to constant application of fo...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
Shin splints' is a condition, which is characterized by pain in the shin bone, the bone that is present in front of the leg. Shin splints tend to occur quite frequently in runners and dancers as their activities tend to stress the shin bone.
Causes: When excess force is applied to the shinbone, it may result in swelling of the muscles, causing pain and inflammation. It may also occur from stress reactions to fractures in the bone. Cracks tend to develop due to constant application of fo...more
Causes: When excess force is applied to the shinbone, it may result in swelling of the muscles, causing pain and inflammation. It may also occur from stress reactions to fractures in the bone. Cracks tend to develop due to constant application of fo...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
MS - Orthopaedics, M Ch. Ortho, Shoulder...read more
Orthopedic Doctor•Hyderabad
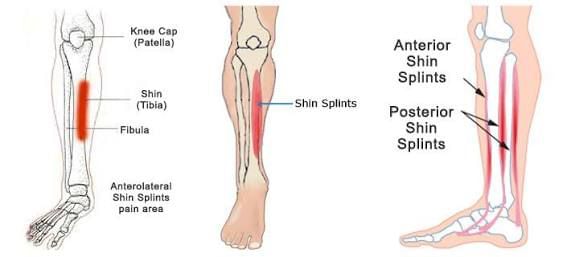
Shin splints, the catch-all term for lower leg pain that occurs below the knee either on the front outside part of the leg (anterior shin splints) or the inside of the leg (medial shin splints), are the bane of many athletes, runners, tennis players, even dancers. They often plague beginning runners who do not build their mileage gradually enough or seasoned runners who abruptly change their workout regimen, suddenly adding too much mileage, for example, or switching from running on flat surface...more
Last Updated: 8 years ago• Featured Tip
Share
Bookmark
Report
Shin splints' is a condition, which is characterized by pain in the shin bone, the bone that is present in front of the leg. Shin splints tend to occur quite frequently in runners and dancers as their activities tend to stress the shin bone.
Causes
When excess force is applied to the shinbone, it may result in swelling of the muscles, causing pain and inflammation. It may also occur from stress reactions to fractures in the bone. Cracks tend to develop due to constant applicati...more
Causes
When excess force is applied to the shinbone, it may result in swelling of the muscles, causing pain and inflammation. It may also occur from stress reactions to fractures in the bone. Cracks tend to develop due to constant applicati...more
Last Updated: 8 years ago• Featured Tip
Share
Bookmark
Report
Shin splints' is a condition, which is characterized by pain in the shin bone, the bone that is present in front of the leg. Shin splints tend to occur quite frequently in runners and dancers as their activities tend to stress the shin bone.
Causes
When excess force is applied to the shinbone, it may result in swelling of the muscles, causing pain and inflammation. It may also occur from stress reactions to fractures in the bone. Cracks tend to develop due to constant applicati...more
Causes
When excess force is applied to the shinbone, it may result in swelling of the muscles, causing pain and inflammation. It may also occur from stress reactions to fractures in the bone. Cracks tend to develop due to constant applicati...more
Book appointment with top doctors for Splinting treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously