Get the App
For Doctors
Login/Sign-up
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Spinal Deformity Correction Tips
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Osteogenesis Imperfecta (OI) is a group of genetic disorders that primarily affect the bones, making them extremely weak. It is also known as brittle bones disease . This genetic disease is incurable and the treatment is primarily focused on pacifying the condition by reducing pain and strengthening the bones.
The symptoms of OI include, but are not limited to, recurring fractures, bluish tinge in the white of the eyes, hearing loss, breathing problems, short height, loose joints and d...more
The symptoms of OI include, but are not limited to, recurring fractures, bluish tinge in the white of the eyes, hearing loss, breathing problems, short height, loose joints and d...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Your spine or backbone is composed of 26 bone discs, known as vertebrae. The vertebra shields your spinal cord and allows you to bend forwards and backwards, and stand. However, a number of problems, such as the following can change the structure or cause the vertebrae and its surrounding tissues to become damaged
Injuries
Infections
Tumours
Changes in bone formation due to ageing herniated disks, spinal stenosis
Conditions like scoliosis and ankylosing spo...more
Injuries
Infections
Tumours
Changes in bone formation due to ageing herniated disks, spinal stenosis
Conditions like scoliosis and ankylosing spo...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Physical deformities that occur due to birth defects can affect one both physically and psychologically, and thus giving them the right treatment is important. Typically, a physical deformity usually refers to musculoskeletal deformities and these can be treated using deformity correction.
Deformity correction refers to the process of adjusting or modifying such bone deformities. Although the process can be used for almost any part of the skeletal structure, it is usually implemented on...more
Deformity correction refers to the process of adjusting or modifying such bone deformities. Although the process can be used for almost any part of the skeletal structure, it is usually implemented on...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
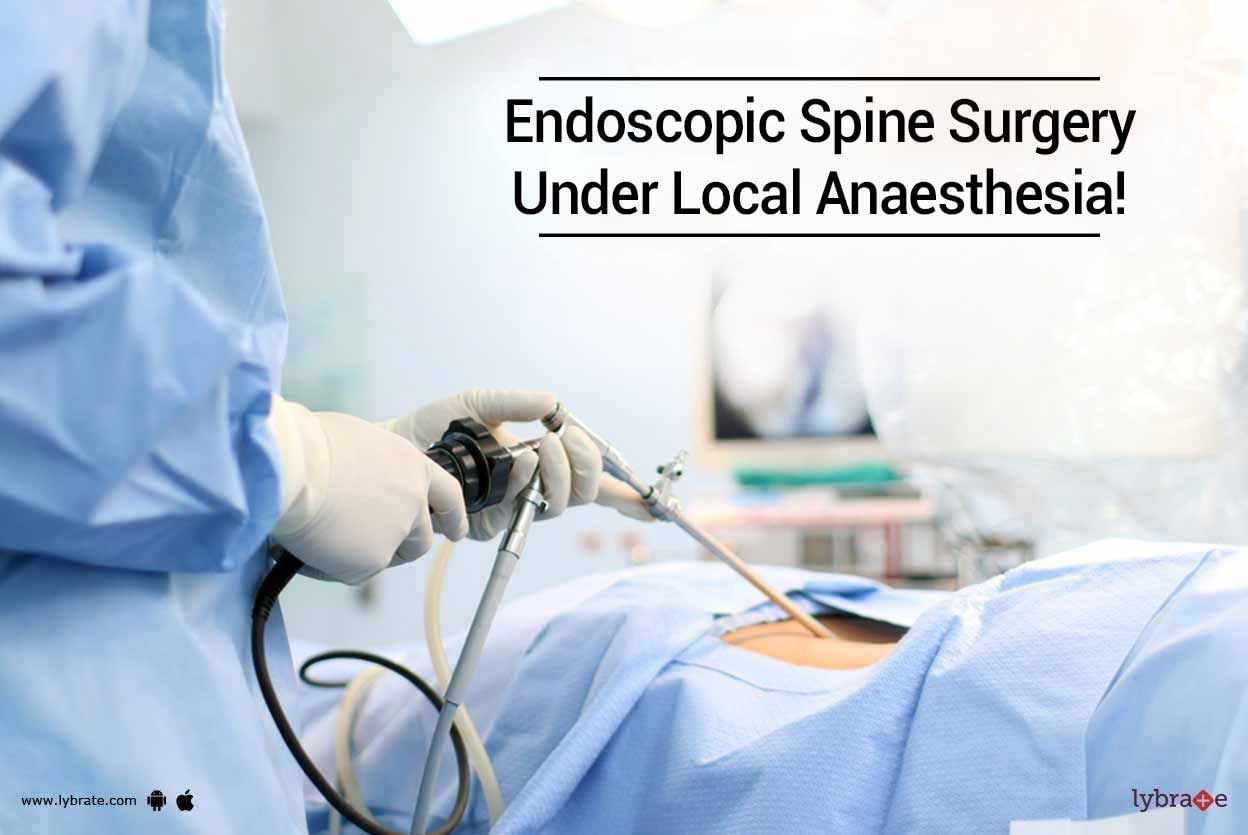
Surgery on the spine is typically performed as an open surgery. This implies that the surgery is performed by making a large incision that allows the surgeon to do the surgery while seeing the spine. However, advancements in medicine have helped surgeons operate on the spine through minimally invasive surgical techniques. This type of surgery involves making a few small incisions instead of a large incision through which the surgeon inserts specially designed instruments to operate on the spine....more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Spinal Tumors are an abnormal mass that grows in the spinal cord or around it. Since these tumors occur in the spinal region, whether spinal cord or column, they came to be known as Spinal tumors. The primary tumor originates in the spine, and secondary tumors may grow in the other areas. They can be benign or malignant. Oncologists classify the spinal tumors according to their location and nature of cancer. They can be cervical, thoracic, lumbar or sacrum.
Causes of Spinal Tumor
more
Causes of Spinal Tumor
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Spinal surgery is a process used for correcting the problems in your spine. The process involves welding two bones or vertebrae into one single bone. This reduces the movement of those bones, which in turn, helps to reduce back pain and stabilize the spine.
This type of surgery is performed when physiotherapy and medicines have not helped cure your back pain. The specialists recommend this option when they are able to understand the actual reason behind your pain.
To locate the...more
This type of surgery is performed when physiotherapy and medicines have not helped cure your back pain. The specialists recommend this option when they are able to understand the actual reason behind your pain.
To locate the...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Clinical Fellowship In Pain Management, ...read more
Pain Management Specialist•Hyderabad
What is spinal compression fracture?
Spinal compression fractures are getting frequent due to the many lifestyle changes which we undergo. The body should not be made to be put use in a certain way like posture, lifting heavy weights, etc. However, prolonged and repeated usage affects the spine directly and results in compression fractures. Though the condition looks, gratifying, modern science has advanced to levels where the fractures can be addressed very effectively, and the pain symptom...more
Spinal compression fractures are getting frequent due to the many lifestyle changes which we undergo. The body should not be made to be put use in a certain way like posture, lifting heavy weights, etc. However, prolonged and repeated usage affects the spine directly and results in compression fractures. Though the condition looks, gratifying, modern science has advanced to levels where the fractures can be addressed very effectively, and the pain symptom...more
12 people found this helpful
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
What is Spinal Stenosis: The narrowing of the gaps in the spine or the backbone is called as Spinal stenosis. This leads to pressure on the nerves and the spinal cord. 5% of cases of spinal stenosis are seen in the low back of the lumbar spine. In some cases the narrowing of the spine leads to the compressing of the nerve root, which leads to pain in the leg.
Causes of spinal stenosis: It can be caused by aging, arthritis, trauma to the spine, spondylolisthesis and tumor of the spinemore
Causes of spinal stenosis: It can be caused by aging, arthritis, trauma to the spine, spondylolisthesis and tumor of the spine
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
MS - Orthopaedics, MCH, Membership of th...read more
Orthopedic Doctor•Delhi
Spinal surgery becomes inevitable when back pain cannot be managed with medications and/or exercise. This is a major decision and requires planning for many things before, during, and after the surgery.
Before a spinal surgery - This preparation will help in smooth recovery, especially if you do not have a full-time caretaker.
Discontinue pain killers: Discontinue pain killers at least 10 to 14 days before surgery. These are blood thinners and can prolong bleeding during the s...more
Before a spinal surgery - This preparation will help in smooth recovery, especially if you do not have a full-time caretaker.
Discontinue pain killers: Discontinue pain killers at least 10 to 14 days before surgery. These are blood thinners and can prolong bleeding during the s...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Introduction Scoliosis is the abnormal twisting and curvature of the spine. It is usually first noticed by a change in the appearance of the back. There are several types of scoliosis based on the cause and age when the curve develops; the majority of patients have no known cause.
Typical signs include:
1. Visibly curved spine
2. One shoulder is higher than the other
3. One shoulder or hip being more prominent than the other
4. Clothes not hanging properly
5. A ...more
Typical signs include:
1. Visibly curved spine
2. One shoulder is higher than the other
3. One shoulder or hip being more prominent than the other
4. Clothes not hanging properly
5. A ...more
Book appointment with top doctors for Spinal Deformity Correction treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously