Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTips
Scaling and Root Planing Tips
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
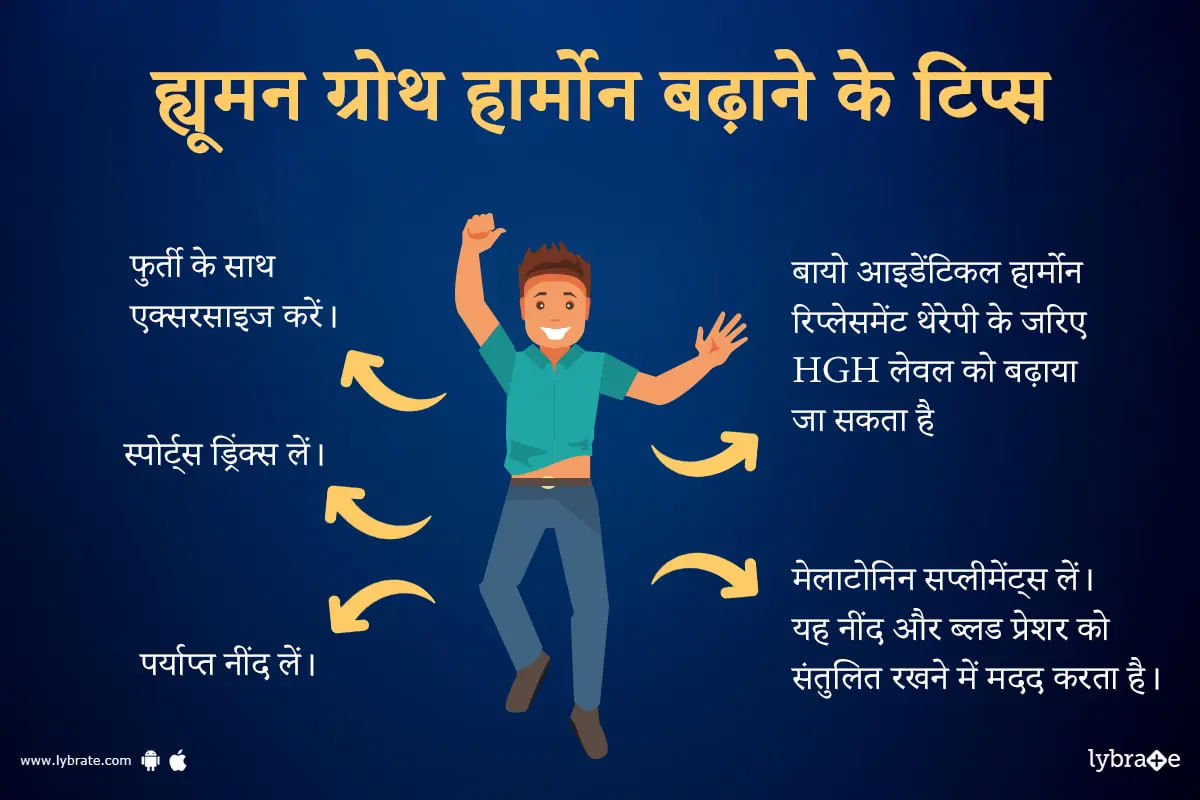
ह्यूमन ग्रोथ हार्मोन यानी एचजीएच पिट्यूटरी ग्लैंड में उत्पन्न होता है और बच्चों और किशोरों में ग्रोथ को बढ़ावा देता है। यह शरीर की संरचना, शरीर के तरल पदार्थ, मांसपेशियों और हड्डियों के विकास, शुगर और फैट मेटाबॉलिज्म, और संभवतः हृदय की सेहत को भी विकसित करने में भी मदद करता है। एचजीएच को बाहर से सप्लीमेंट के तौर पर भी लिया जाता है और यह दवा की दुकानों और ऑनलाइन उपलब्ध अन्य उत्पादों में सक्रिय घटक है। आइए विस्तार से जानते हैं कि ह्यूमन ग्रोथ हार्मोन को बढ़ाने के लिए 15 सटीक और...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
People suffering from acne scars go through mental pressure as well as emotional problems. Studies have shown that people suffering from acne scars are more likely to suffer from anxiety, depression, low self-esteem, and low confidence. Typical causes of acne include bacteria, excess oil, and clogged hair follicles. The acne can get more severe due to some medications, stress, or diet.
Severe acne may be treated with proper medications but it leaves behind scars. These scars can be trea...more
Severe acne may be treated with proper medications but it leaves behind scars. These scars can be trea...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The prostate, a small walnut-shaped gland located under the bladder. Its main function is to add fluid to the semen produced by the reproductive system. It does not cause any problems in men until later in life when it begins to grow. Benign Prostatic Hyperplasia or BPH can affect some men, but you can reduce your risk of this condition.
Risk factors for BPH
Knowing and understanding factors that cause BPH will help you avoid or reduce your risk of this condition. In addition to age...more
Risk factors for BPH
Knowing and understanding factors that cause BPH will help you avoid or reduce your risk of this condition. In addition to age...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Dentist•Jalandhar
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Benign Prostatic Hyperplasia(BPH) is the enlargement of the prostate gland which can lead to other serious problems of the urinary tract, bladder, and kidneys.
It might be the result of an infection of the urinary tract or a scar in the bladder from an earlier surgery. Prostrate inflammation or urethral narrowing can also cause an enlargement of the gland. Kidney or bladder stones may also be responsible for prostate enlargement.
Age also plays a role in the enlargement of the ...more
It might be the result of an infection of the urinary tract or a scar in the bladder from an earlier surgery. Prostrate inflammation or urethral narrowing can also cause an enlargement of the gland. Kidney or bladder stones may also be responsible for prostate enlargement.
Age also plays a role in the enlargement of the ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
A root canal is a treatment to repair and save badly damaged or infected tooth. The procedure involves removing the damaged area of the tooth (the pulp), cleaning and disinfecting it and then filling and sealing it. The common causes affecting the pulp are cracked tooth, a deep cavity, repeated dental treatment to the tooth or trauma. The term "root canal" comes from cleaning of the canals inside the tooth's root.
Millions of teeth are treated and saved each year with the root canal, or...more
Millions of teeth are treated and saved each year with the root canal, or...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Skin problems are very common among all age groups. However, once you start ageing, keeping that natural glow on your face is a struggle. This is because our skin goes through a lot of wear and tear in extreme conditions and gradually loses its radiance over time. Before you know it, you develop fine lines, wrinkles, scars and blemishes on the face. This not only leaves you devastated but also lowers your self-esteem and can be unappealing.
Essential beauty products may not be the solut...more
Essential beauty products may not be the solut...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
BHMS, PG Diploma In Clinical Cosmetology...read more
Cosmetic Physician•Navi Mumbai
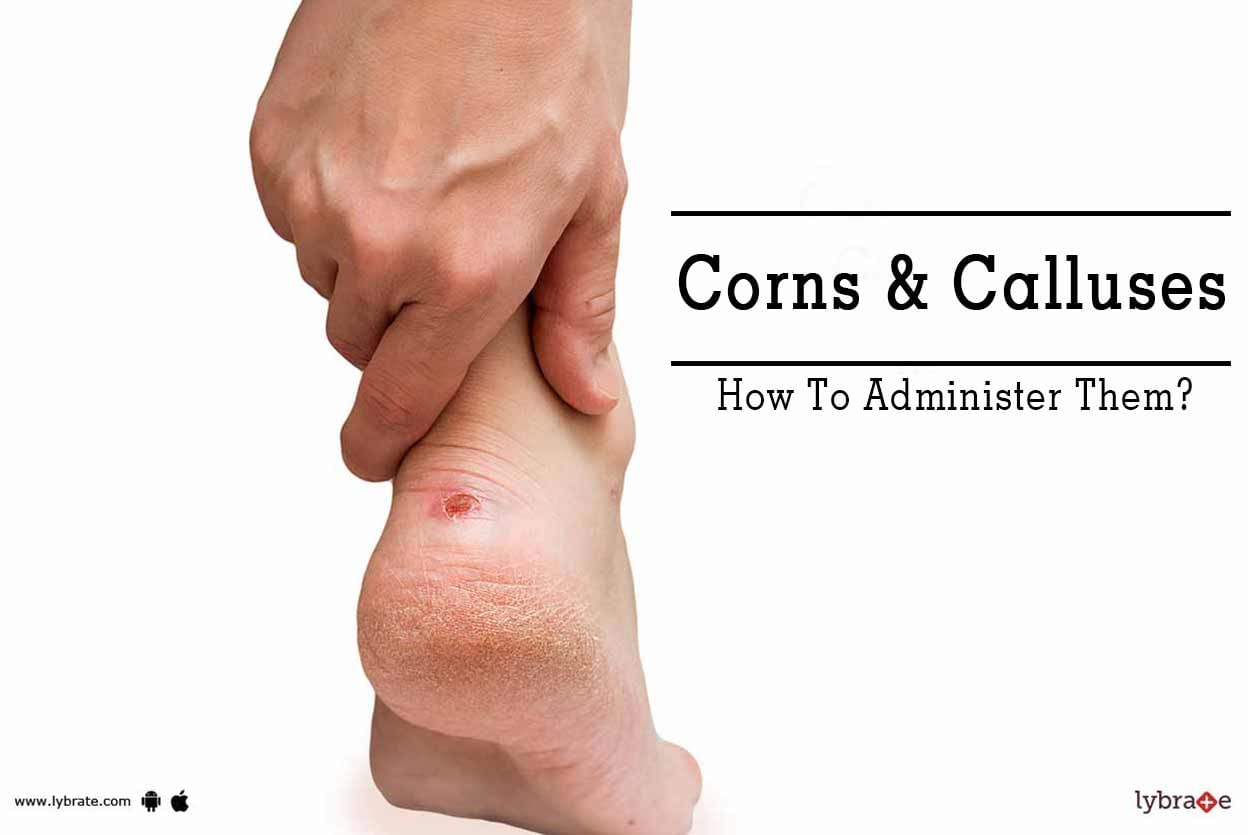
Corn, Warts, and Moles are not life-threatening. But they can be very ugly and uncomfortable. One should book an appointment with the cosmetic physician for spot removal. There are a number of methods for Corn, Warts, and Moles removal, which are safe and easy on pockets.
Corn, Warts, and Moles can be painful and disrupt in daily life. However, with the appropriate removing method, one can lead a normal and comfortable lifestyle.
Corn:
Corn typically appears at the bo...more
Corn, Warts, and Moles can be painful and disrupt in daily life. However, with the appropriate removing method, one can lead a normal and comfortable lifestyle.
Corn:
Corn typically appears at the bo...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Corns and calluses are defined as thickened and hardened areas of the skin which are formed due to excess pressure, friction or rubbing in a particular area. They generally form at the bottom of the feet and can cause discomfort and pain while walking. Corns usually form on the sides and tops of toes. There are several variants of corn such as hard corn, soft corn and seed corns. Calluses typically form in areas which undergo high friction. It can appear on hands and feet. Read on to find more a...more
Book appointment with top doctors for Scaling and Root Planing treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously