Plasma (Human Anatomy): Image, Functions, Diseases and Treatments
Last Updated: Mar 17, 2023
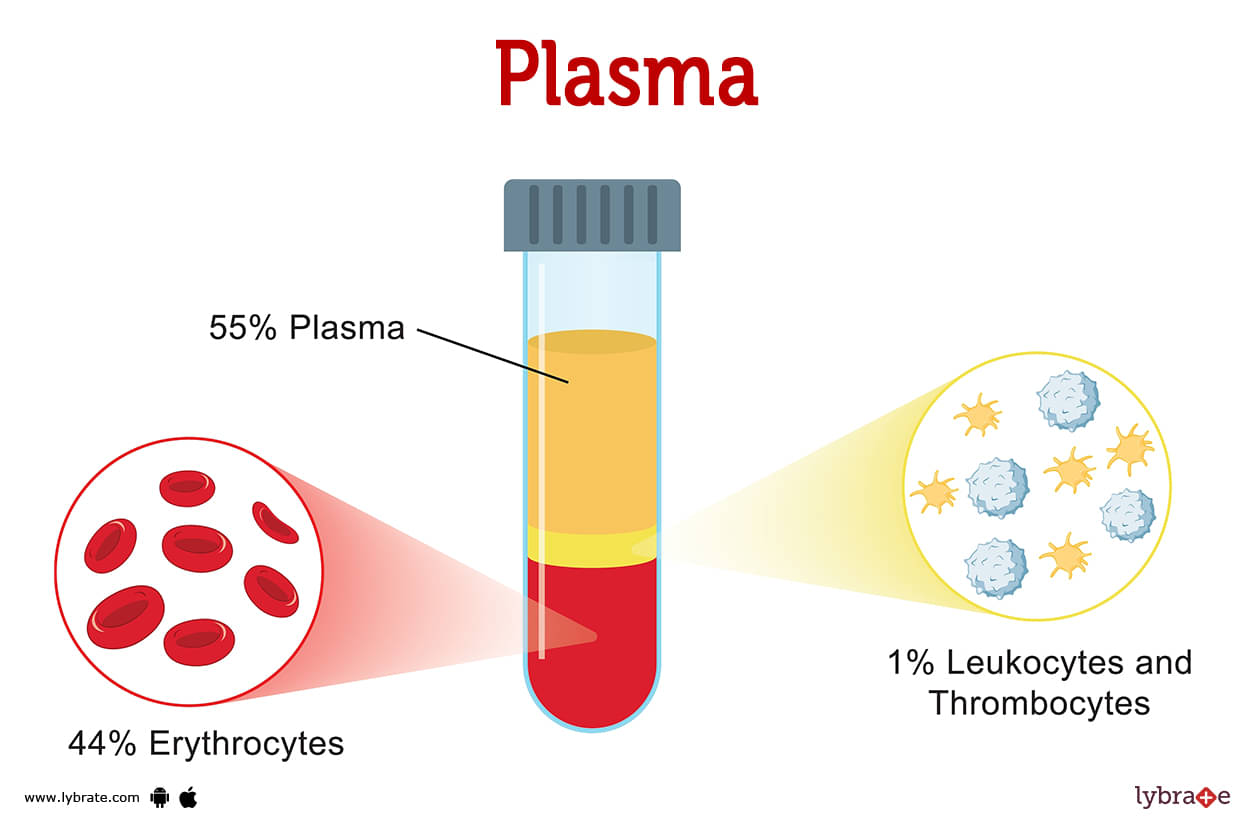
Plasma Image
Your blood's liquid portion, called plasma, makes up 55% of the total volume of your blood. Your circulatory system has to transport plasma in order for it to aid in infection prevention, nutrient distribution, waste removal, and wound healing. Plasma is the liquid component of blood. Whole blood is made up of platelets, red, white, and other blood cells that float in your plasma. The amount of blood in your body ranges from 5 to 6 quarts (5 liters).
Plasma Functions
- Plasma serves several functions in the body. Plasma is in charge of redistributing water to where it is needed in your body. It aids in d elivering hormones, nutrients, and proteins to various parts of your body while also assisting in the exchange of oxygen and carbon dioxide.
- It helps in keeping blood vessels from collapsing or becoming clogged, and k eeping blood pressure and circulation normal. It absorbs and releases heat to regulate body temperature.
- It also plays a major role in waste removal from cells and transport to the liver, lungs, and kidneys for excretion, and aiding in the clotting of blood Infection protection against bacteria, viruses, fungi, and parasites.
What is plasma used for?
Your body requires plasma to function. Plasma donations can assist you replenish your blood and plasma you've lost if you lose a significant volume of blood via surgery, an accident, a clotting issue, an immunological weakness, or a bleeding disorder.
How do I donate plasma?
There are two methods for donating plasma:
- Donating whole blood: Whenever you donate whole blood, a medical professional puts a needle into an arm vein and draws blood. Later, plasma will be separated as needed in a laboratory.
- Donating plasma only (plasmapheresis): A healthcare professional will place a needle into the a vein in your arm to take only the plasma, comparable to whole blood donation. The plasma is subsequently separated from the blood cells and platelets by placing this blood in a centrifuge. The device takes out the plasma and gives the body its remaining blood components along with a saltwater (saline) solution. After taking plasma from your bloodstream, the lab freezes it within 24 hours to preserve the clotting factors and immunoglobulins. The plasma that has been frozen can be kept for a year. Plasma obtained from donors with an AB blood group is best because it doesn't have antibodies and can be given to people with any blood type. However, anyone can give blood.
Where is plasma developed?
Plasma cells are made by cells in the umbilical cord that are part of the embryo. Plasma proteins are made in the soft tissue of the bones (bone marrow), in your liver cells, in blood cells that are dying, and in your spleen.
What does plasma look like?
Plasma, in contrast to other gases, may be melted and poured. The colour is a delicate yellow that resembles straw in tone. Even though more over half of your blood's volume is made up of plasma, red blood cells are what give your blood its predominant colour.
What percentage of blood is plasma?
About half of your blood is plasma. Next in line at 44% of blood volume are red blood cells, followed by 1% each of white blood cells and platelets.
How do you separate plasma from the other components of blood?
In the process known as centrifugation, the whole blood sample is divided into a number of layers as it is spun in a centrifuge machine after your blood has been extracted. Plasma makes up the top layer, which is yellow, and the layer below that contains the blood cells (both red and white) as well as platelets
What is plasma made of?
The components that make up blood plasma are: Water, proteins (albumin, fibrinogen, globulin), salts and minerals (which have been liquefied and carry an electrical charges-electrolytes), and Immunoglobulins (components that fight infections).
What proteins are in plasma?
Plasma may contain a variety of proteins, including:
- Albumin: carries hormones, enzymes, and vitamins throughout your body. It also helps to maintain blood pressure regulation so that tissues don't leak extra fluid.
- Antibodies are also referred to as immunoglobulins: wards off pathogens such as bacteria, fungi, viruses, and cancer cells from entering your body.
- Clotting factors (Fibrinogen and the von Willebrand factor): reduce bleeding.
Plasma Conditions and Disorders
- Plasma cell neoplasms: These are tumours caused by abnormal plasma cells or cells that may grow either in hard or soft tissues. In the fight against infection, M protein, an antibody protein generated by plasma cells, is both unnecessary and ineffectual.
- Monoclonal gammopathy: Monoclonal gammopathies are disorders attributed to the presence of abnormal proteins in the blood. Plasma cells, which are responsible for the generation of these proteins, reside in the bone marrow. Plasma cells are a kind of leukocyte. Their major aim is infection prevention.
- Multiple myeloma: A plasma cell's aberrant development is what leads to the disease known as multiple myeloma. The production of immunoglobulins by healthy plasma cells supports the fight against illness.
- Heavy chain diseases (rare): In the relatively uncommon B cell proliferative illnesses known as heavy chain diseases, a component of the immunoglobulin heavy chain is generated as a monoclonal (M) protein without a bound light chain.
- Hypercalcemia: Organ damage, especially to the kidneys, from hypercalcemia or harmful light chains released by malignant plasma cells. Some M-proteins have been seen to have antibodies that work against self-antigens.
- Impaired immunity: Problems with the immune system, such as fewer T-cell responses and less production of other immunoglobulins.
- Bleeding tendency: M-protein can cause bleeding in a number of ways, such as by coating platelets, stopping clotting factors from working, making blood thicker, and so on.
- Amyloidosis: Heart and kidneys are the most common sites of M-protein fibrillar deposit accumulation, which leads to amyloidosis.
- Mixed cryoglobulinemia syndrome: Purpura, arthralgia, and weakening to more severe neurologic and renal involvement are the clinical manifestations of mixed cryoglobulinemia syndrome (MCS), which is characterised by the presence of circulating type II or type III cryoglobulins in the blood.
- The POEMS syndrome: Nerve damage as well as other systemic signs may be brought on by a disorder known as POEMS syndrome, which affects the blood in very rare cases and is passed down via families. Symptoms include fatigue, numbness, and tingling in the legs (and occasionally the hands), as well as difficulty breathing.
- Waldenstrom's Macroglobulinemia: A rare form of cancer that starts in white blood cells is this one. Those who are afflicted with Waldenstrom macroglobulinemia have an excessively large amount of WBCs in their bone marrow, which may result in a variety of different issues.
Plasma tests
- Plasma protein test: A blood test known as a plasma protein test counts all the proteins present in the plasma. These tests are typically requested by a clinician as part of the larger metabolic panel (CMP) at a visit. Plasma protein concentrations are frequently assessed as a proxy for total protein.
- Complete blood count (CBC): A complete blood count measures the quantity of red and white blood cells as well as the concentration and amount of haemoglobin in each type of cell.
- Blood chemistry test: Your creatine (which reflects renal function), albumin (a protein), calcium, and lactic dehydrogenase quantities are revealed by blood chemistry examination. LDH is a tumor marker. A tumor marker is a substance in malignant or normal cells that responds to malignancy.
- Quantitative immunoglobulin test: A quantitative immunoglobulin test measures the amounts of particular antibodies in your blood.
- Electrophoresis: This test detects M-proteins in the blood.
- Urine tests: The existence of Bence Jones protein in the urine is an additional sign of multiple myeloma; thus, your healthcare provider may ask you to collect urine at residence for 24 hours.
What are the symptoms of plasma disorders?
Pain in the bones, bruising and/or bleeding readily, cardiac palpitations (arrhythmia), and achy hands and wrists are all signs of plasma problems (carpal tunnel syndrome).
Plasma Treatments
- Chemotherapy: Chemotherapy is used to get rid of as many abnormal plasma cells as possible.
- Immunotherapy: It is a way to treat cancer that tends to work by enhancing the immune system of the body to make more cells which can fight the disease.
- Radiation therapy: Bone marrow and blood are rich in specialised cells called stem cells. In many cases, doctors will suggest an autologous stem cell transplant. In this technique, the patient's own healthy stem cells are employed to replace the diseased or damaged ones. Good quality donor plasma stem cells are quite uncommon. The process of a stem cell allogeneic transplant is underway.
- Plasma Medicines: Blood thinners for plasma dysfunction: Aspirin is a significant painkiller that also serves as an antipyretic and an anti-inflammatory medication. Any type of bleeding, including gastrointestinal bleeding, is a contraindication.
- Clopridogrel for increase in fluidity in the plasma: It's an ADP receptor inhibitor that's also especially prescribed for vascular bleeding and used therapeutically when standing; it is contraindicated in the event of an unexpected haemorrhage.
- Thrombolytics: Thrombin and platelet factor 10 activity are both decreased by heparin. It is used to treat both pulmonary embolism and deep vein thrombosis. If bleeding is present, it should not be utilised. Apixaban for reducing coagulation of blood: It is a Factor Xa inhibitor that is used to treat deep vein thrombosis, pulmonary embolism, and lowers the risk of atrial fibrillation.
- Cyclosporine: One of the most significant calcineurin inhibitors, it is frequently utilised during transplant surgeries. Nephrotoxicity, hypertension, alopecia, gingival hyperplasia, hirsutism, hyperlipidemia, and other adverse effects are only a few of the complications it might cause.
- Alteplase: It works as a strong tissue plasminogen activator to treat myocardial infarction, pulmonary embolism, and reduce the risk of ischemic stroke. It is not advised when there is a very high danger of bleeding and neurological adverse effects.
How do I keep my plasma healthy?
You may maintain the health of your plasma by consuming a significant amount of water and maintaining a state of hydration, by k eeping a healthy diet, and by e xercising on a consistent basis. Maintaining a clean and healthy lifestyle is essential to warding against infections. Increasing your consumption of vitamins will strengthen your resistance against disease.
Table of content
Find Hematologist near me
Ask a free question
Get FREE multiple opinions from Doctors