Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Peritonitis Tips
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Peritoneal Cancer is a rare form of cancer. It forms a thin layer of tissue in the abdomen, which lines that region. It covers the parts like uterus, gallbladder, and rectum. The structure is called the peritoneum which is made of epithelial cells. For the organs to move freely inside the abdomen, the peritoneum produces fluid.
This cancer is different from intestinal cancer or the general type of cancer which tends to spread.
Symptoms of Peritoneal Cancer:
This cancer...more
This cancer is different from intestinal cancer or the general type of cancer which tends to spread.
Symptoms of Peritoneal Cancer:
This cancer...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
No Blood, No needle, No visit to hospital, you can do yourself at home with water. A thin layer of transparent screen like structure hangs in front of the abdominal muscles known as peritoneum. This peritoneum protects the abdominal structures and the muscle. This can also be used for performing dialysis which is carried out when the functioning of kidney gets affected. In peritoneal dialysis a thin and soft catheter is placed in the person s belly one week before performing the procedure.
<...more
<...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
No Blood, No needle, No visit to hospital, you can do yourself at home with water. A thin layer of transparent screen like structure hangs in front of the abdominal muscles known as peritoneum. This peritoneum protects the abdominal structures and the muscle. This can also be used for performing dialysis which is carried out when the functioning of kidney gets affected. In peritoneal dialysis a thin and soft catheter is placed in the person s belly one week before performing the procedure.
<...more
<...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
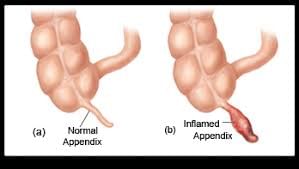
APPENDICITIS LAPAROSCOPIC APPENDECECTOMY
APPENDICITIS is an inflammation of the appendix, a finger-shaped pouch that projects from your colon on the lower right side of your abdomen. The appendix doesn't seem to have a specific purpose. Appendicitis causes pain in lower right abdomen. However, in most people, pain begins around the navel and then moves. As inflammation worsens, appendicitis pain typically increases and eventually becomes severe. Although anyone can develop appendicitis,...more
APPENDICITIS is an inflammation of the appendix, a finger-shaped pouch that projects from your colon on the lower right side of your abdomen. The appendix doesn't seem to have a specific purpose. Appendicitis causes pain in lower right abdomen. However, in most people, pain begins around the navel and then moves. As inflammation worsens, appendicitis pain typically increases and eventually becomes severe. Although anyone can develop appendicitis,...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
No Blood, No needle, No visit to hospital, you can do yourself at home with water. A thin layer of transparent screen like structure hangs in front of the abdominal muscles known as peritoneum. This peritoneum protects the abdominal structures and the muscle. This can also be used for performing dialysis which is carried out when the functioning of kidney gets affected. In peritoneal dialysis a thin and soft catheter is placed in the person s belly one week before performing the procedure.
<...more
<...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
No Blood, No needle, No visit to hospital, you can do yourself at home with water. A thin layer of transparent screen like structure hangs in front of the abdominal muscles known as peritoneum. This peritoneum protects the abdominal structures and the muscle. This can also be used for performing dialysis which is carried out when the functioning of kidney gets affected. In peritoneal dialysis a thin and soft catheter is placed in the person s belly one week before performing the procedure.
<...more
<...more
Last Updated: 8 years ago• Featured Tip
Share
Bookmark
Report
No Blood, No needle, No visit to hospital, you can do yourself at home with sterile fluid. A thin layer of transparent screen like structure hangs in front of the abdominal muscles known as peritoneum. This peritoneum protects the abdominal structures and the muscle. This can also be used for performing dialysis which is carried out when the functioning of kidney gets affected. In peritoneal dialysis a thin and soft catheter is placed in the person s belly one-two weeks before performing the pro...more
Last Updated: 8 years ago• Featured Tip
Share
Bookmark
Report
Endometriosis is an often painful disorder in which tissue that normally lines the inside of your uterus the endometrium grows outside your uterus. Endometriosis most commonly involves your ovaries, fallopian tubes and the tissue lining your pelvis. Rarely, endometrial tissue may spread beyond pelvic organs.
With endometriosis, displaced endometrial tissue continues to act as it normally would it thickens, breaks down and bleeds with each menstrual cycle. Because this displaced ti...more
With endometriosis, displaced endometrial tissue continues to act as it normally would it thickens, breaks down and bleeds with each menstrual cycle. Because this displaced ti...more
Last Updated: 8 years ago• Featured Tip
Share
Bookmark
Report
Chronic kidney disease or CKD is the decreased function of the function of the kidney for a minimum of three months or more. In this the end stage renal disease usually refers to the end of the kidney function where the kidneys work for less than 15% of what they are supposed to. The kidneys play a vital role in the human body and if they do not function properly then a person can die. The functioning of many organs depends on the kidneys. However, the main function of the kidneys is to remove t...more
Last Updated: 8 years ago• Featured Tip
Share
Bookmark
Report
No Blood, No needle, No visit to hospital, you can do yourself at home with water. A thin layer of transparent screen like structure hangs in front of the abdominal muscles known as peritoneum. This peritoneum protects the abdominal structures and the muscle. This can also be used for performing dialysis which is carried out when the functioning of kidney gets affected. In peritoneal dialysis a thin and soft catheter is placed in the person s belly one week before performing the procedure.
<...more
<...more
Book appointment with top doctors for Peritonitis treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously