Primary osteoarthritis
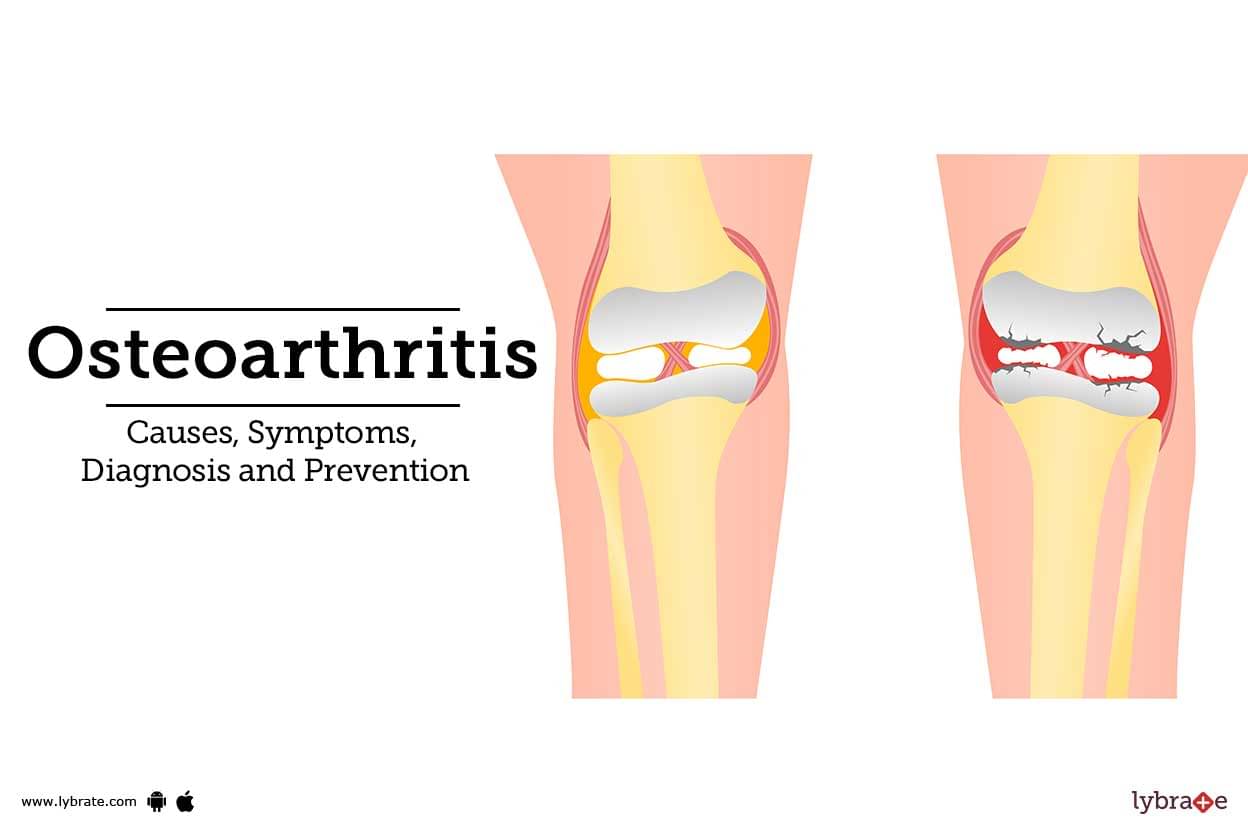
This type of osteoarthritis is the most frequently diagnosed and is thought to develop primarily as a result of 'wear and tear' through time. As a result, it is linked to aging; in fact, the most significant risk factor for OA is aging, and the more a person utilizes their joints, the greater the likelihood that they will develop this type of OA. Theoretically, if we live to a sufficiently old age, primary OA is unavoidable.
Beginning about the age of 55 or 60, people typically start to experience this type of osteoarthritis. Primary OA is typically classified by the site of involvement (e.g., hands and feet, knee, hip), yet it may potentially affect many joints, as it may be localized to specific joints.