Get the App
For Doctors
Login/Sign-up
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Muscle Weakness Tips
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Weakness of the muscles due to a genetically inherited condition is known as muscular dystrophy. This condition prevents the body from producing the required protein that can help in building muscles. This protein is also responsible for making the muscles strong and stable. This is most commonly seen in children who may seem clumsy as they begin to grow up and indulge in varied kinds of movements. Let us learn more about this condition and the ways in which it may be treated.
1. Sympto...more
1. Sympto...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The trapezius muscle is a triangular muscle which extends from the neck, down to the middle of the upper back and across the shoulder. It is one of the largest muscles in the body. It helps in stabilizing and moving the scapula. When you rotate your neck, move your arms, or even shrug your shoulders, you are able to do it because of the trapezius muscle. Overuse of the muscle can cause it to strain.
Trapezius strain can be quite annoying and uncomfortable as you will have difficulty in ...more
Trapezius strain can be quite annoying and uncomfortable as you will have difficulty in ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
MBBS Bachelor of Medicine and Bachelor o...read more
Orthopedic Doctor•Bhubaneswar
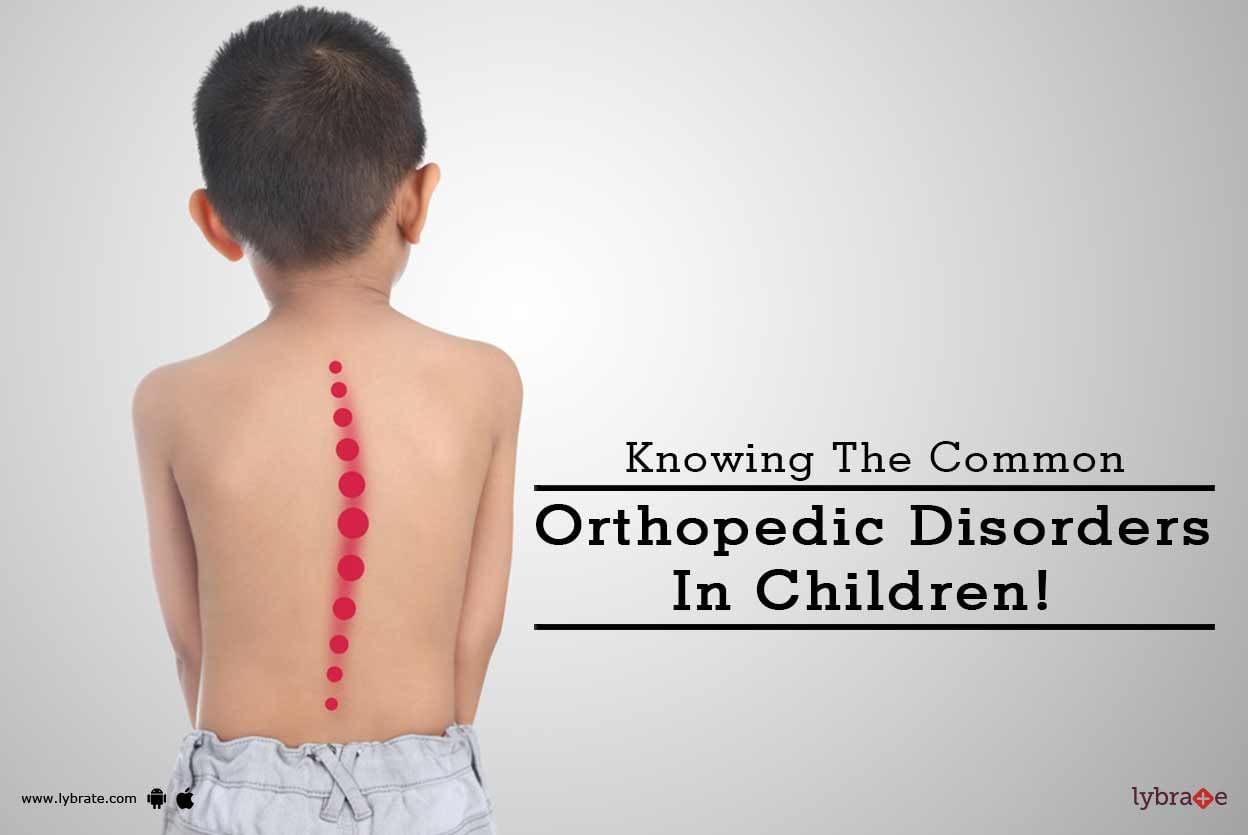
Sometimes children suffer from conditions where their feet may not be in proper shape or size, something that can affect their posture. Most of the times the disorders get corrected themselves as children grow up, but there can be situations where medical attention is required. These conditions can be normal variations in the anatomy as well which don't essentially require treatment. Some of the common orthopedic disorders found in children include:
Flatfeet: While most babies...more
Flatfeet: While most babies...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Sometimes children suffer from conditions where their feet may not be in proper shape or size which can affect their posture. Most of the times the disorders correct themselves as they grow up but certainly, there can be situations where medical attention is required. These conditions can be normal variations in the anatomy as well which don't essentially require treatment. Some of the common orthopedic disorders found in children include:
1. Flatfeet-
While most babies are born with fla...more
1. Flatfeet-
While most babies are born with fla...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
हमारे बदलते रहन-सहन और खान-पान के कारण अब हड्डियों की समस्या एक आम समस्या है. हड्डियों से संबंधित कई तरह के परेशानियों से लोग पीड़ित हैं. हड्डियों के इन परेशानियों को आपको गंभीरता से लेना चाहिए. यदि आप भी ऐसा सोचते हैं कि दिन में एक गिलास दूध पी लेने से हड्डियों में एक दिन के कैल्शियम की पूर्ति हो जाती है, तो आप गलत हैं. दरअसल कैल्शियम, हड्डियों के स्वास्थ्य और मजबूती के साथ ही ब्लड क्लॉटिंग और मांसपेशियों के विकाश में भी मददगार होती है. यही कारण है कि शरीर को अधिक मात्रा में कैल्शियम चाहिए. लेकि...more
33 people found this helpful
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Myelopathy refers to any neurological deficit in the spinal cord. The three most common types of myelopathy are cervical myelopathy, lumbar myelopathy and thoracic myelopathy. Here are the causes and symptoms of myelopathy.
Causes
1. Injury
This is a very common cause of myelopathy. Any type of accident or even a traumatic event can cause myelopathy and perhaps even paralysis.
2. Spinal stenosis
This is a condition in which the spinal cord narrows. It is one of ...more
Causes
1. Injury
This is a very common cause of myelopathy. Any type of accident or even a traumatic event can cause myelopathy and perhaps even paralysis.
2. Spinal stenosis
This is a condition in which the spinal cord narrows. It is one of ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Sometimes children suffer from conditions where their feet may not be in proper shape or size which can affect their posture. Most of the times the disorders correct themselves as they grow up but certainly there can be situations where medical attention is required. These conditions can be normal variations in the anatomy as well which don't essentially require treatment.
Some of the common orthopedic disorders found in children include:
1. Flatfeet
While most babies...more
Some of the common orthopedic disorders found in children include:
1. Flatfeet
While most babies...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Myelopathy refers to any neurological deficit in the spinal cord. The three most common types of myelopathy are cervical myelopathy, lumbar myelopathy and thoracic myelopathy.
Here are the causes and symptoms of myelopathy.
Causes
1. Injury
This is a very common cause of myelopathy. Any type of accident or even a traumatic event can cause myelopathy and perhaps even paralysis.
2. Spinal stenosis
This is a condition in which the spinal cord narrows. I...more
Here are the causes and symptoms of myelopathy.
Causes
1. Injury
This is a very common cause of myelopathy. Any type of accident or even a traumatic event can cause myelopathy and perhaps even paralysis.
2. Spinal stenosis
This is a condition in which the spinal cord narrows. I...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Sometimes children suffer from conditions where their feet may not be in proper shape or size which can affect their posture. Most of the times the disorders correct themselves as they grow up but certainly, there can be situations where medical attention is required. These conditions can be normal variations in the anatomy as well which don't essentially require treatment.
Some of the common orthopedic disorders found in children include:
1. Flatfeet
While most babies are born...more
Some of the common orthopedic disorders found in children include:
1. Flatfeet
While most babies are born...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Muscle strain or muscle pull is a condition, which is characterized by damage to the muscles or its adjoining tendons. Undue pressure can be exerted on the muscle when you are carrying out routine activities such as the sudden lifting of heavy things or playing contact sports. The damage to the muscle is usually in the form of partial or complete tearing of the tendons and fibers attached to the muscles. The small blood vessels in the muscles can also be damaged by the tearing of the muscles, le...more
Book appointment with top doctors for Muscle Weakness treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously