Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Migraine Prophylaxis Tips
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
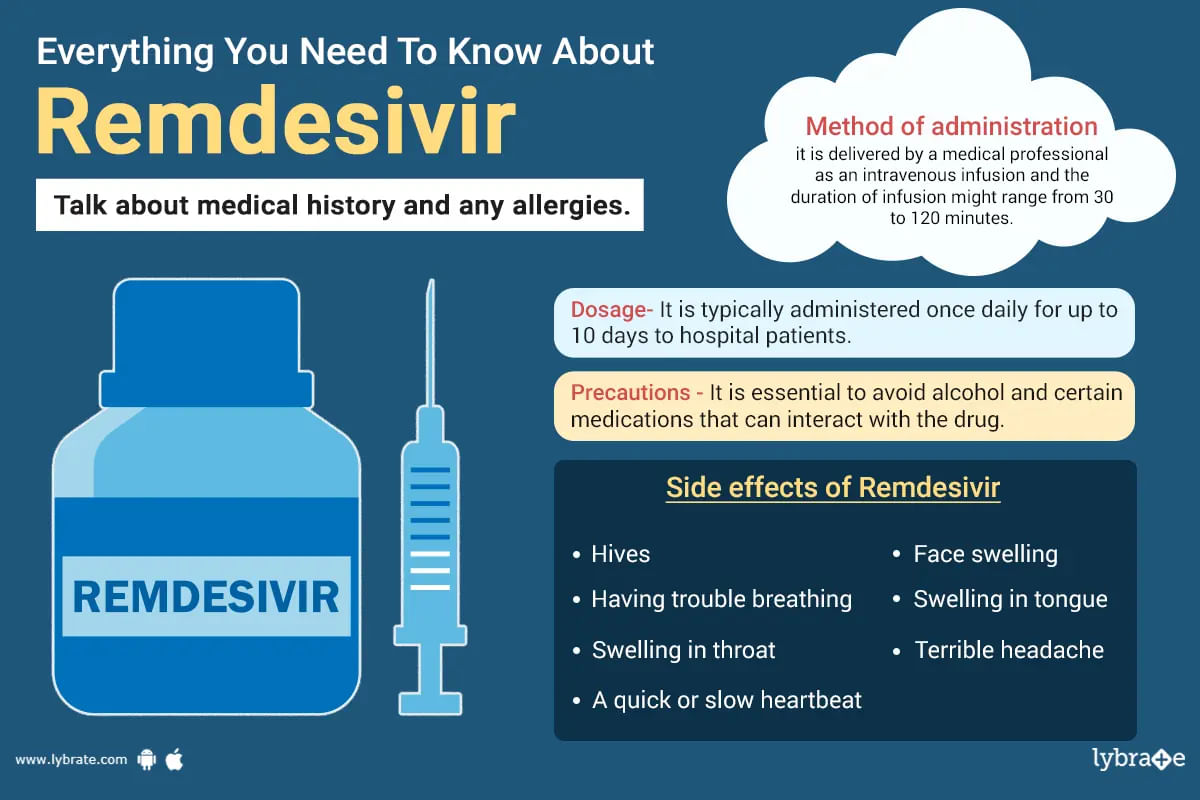
Remdesivir is an antiviral drug used to treat individuals with positive results for covid-19. It has been approved for the treatment of covid-19 and works by preventing the virus from replicating and disseminating itself throughout the body. ;
It can be used by adults and kids who are at least 28 days old and 7 pounds or more (3 kilograms). It is offered to patients who are undergoing medical treatment as well as those with mild-to-moderate covid-19 who ar...more
78 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
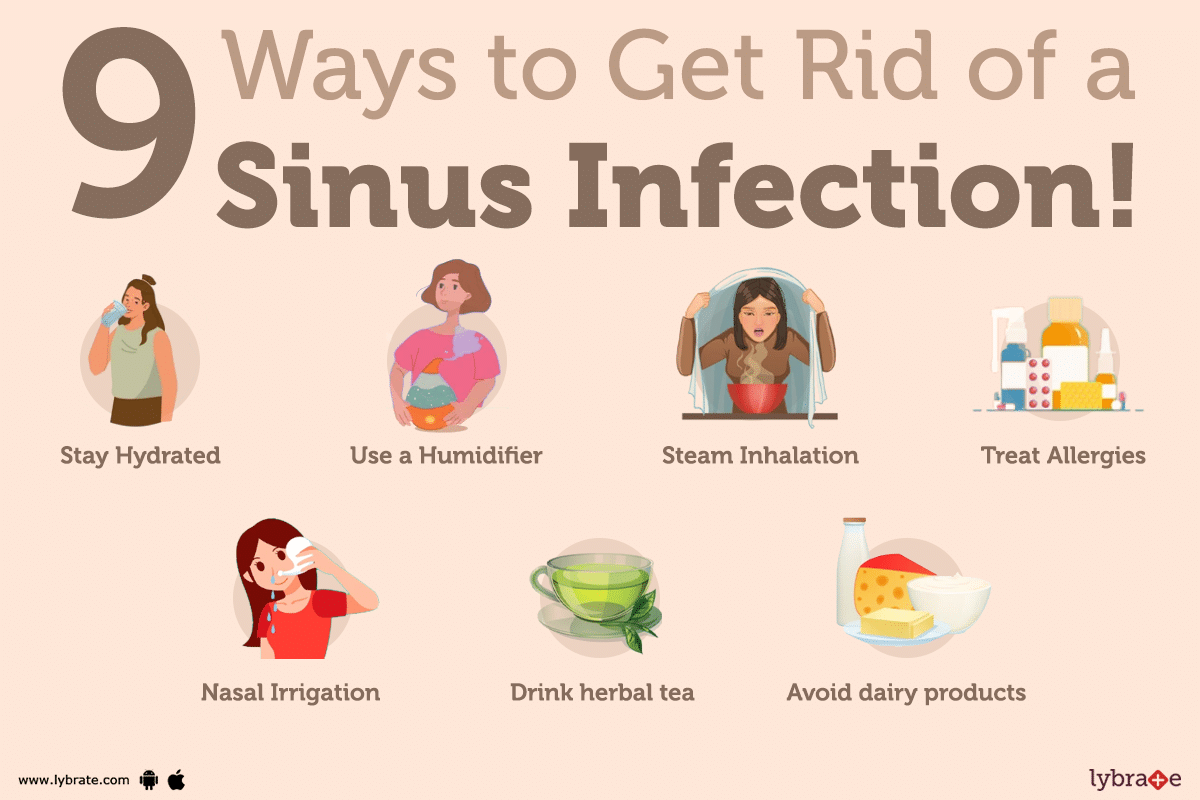
What is sinus infection?
Sinus infection, also known as sinusitis, is an inflammation of the paranasal sinuses, which are air-filled cavities surrounding the nose. ;
This inflammation can be caused by a bacterial or viral infection, or from allergies and environmental irritants like smoke.
What are the signs and symptoms of sinus infection?
The most common symptoms of sinus infection include facial pain/pressure, nasal congestion, nasal di...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
1. Dr. Harihara murthy. P
Https://www. Lybrate. Com/bangalore/doctor/dr-p-harihara-murthy-ear-nose-throat-ent-specialist-1 ;
Mbbs, Ms. - ent, diploma in otorhinolaryngology (dlo)
38 years experience 500 - 600 at clinic 400 online
Dr. Harihara murthy is a highly experienced and well-respected ent specialist in bangalore, india. He obtained his mbbs from k. M. C. Mangalore, mysore university, in 1984, his Ms. In ent from bangalore medic...more
83 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Dr. Prof. Arunangshu bhatacharyya
Https://www. Lybrate. Com/kolkata/doctor/dr-arunangshu-bhatacharyya-orthopedist ;
Mbbs, Ms. - orthopaedics
27 years experience 800 at clinic 400 online
Prof. Arunangshu bhatacharyya, md, is an accomplished orthopaedic surgeon who has devoted his career to helping those in suffering. In 1995, he graduated with an mbbs from burdwan medical college, and in 2000, he earn...more
62 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
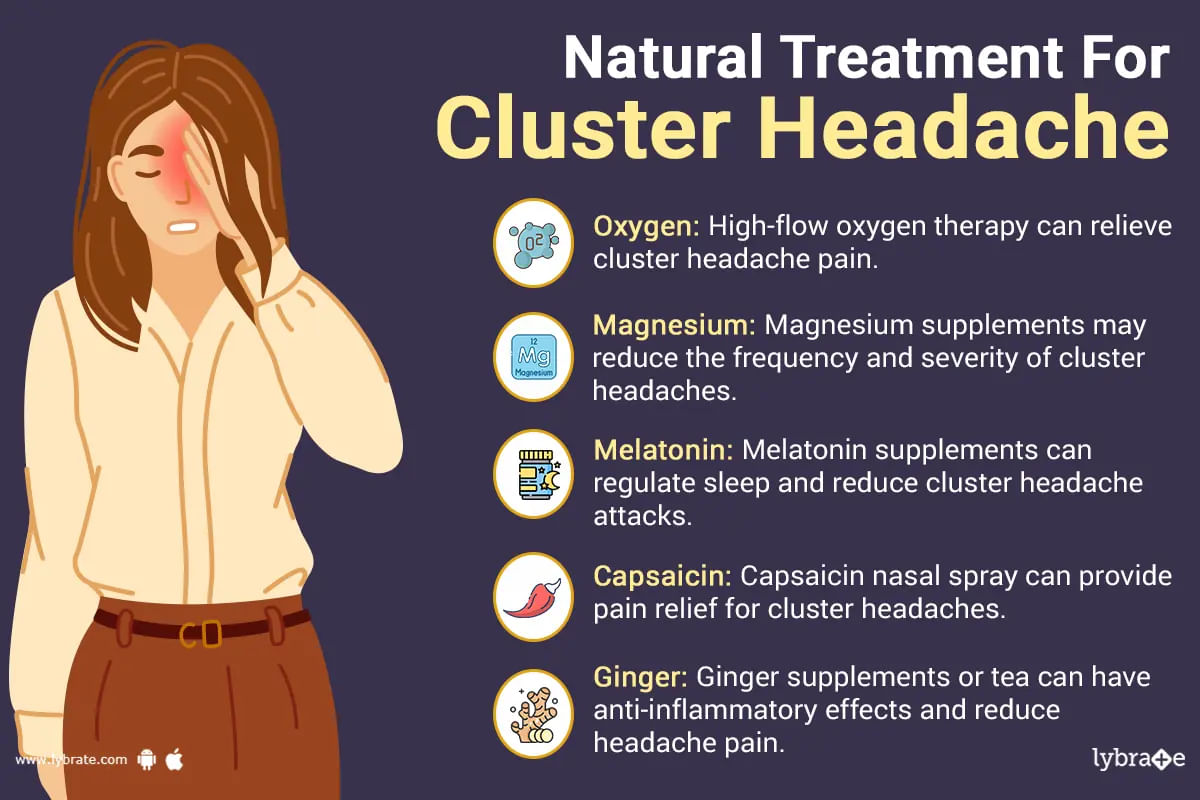
Headache means the pain in the head. The other name of headache is cephalalgia. The pain in the head is the result of the disorder of migraine, cluster headache, headache due to the tension and stress. There are various types of headache, such as cold-stimulus headache, sinus headache, tension headache, cluster headache, hangover headache and migraine headache. The symptoms of headache are pain in the head, neck pain, dizziness, high blood pressure, sensitivity to light, loss...more
287 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
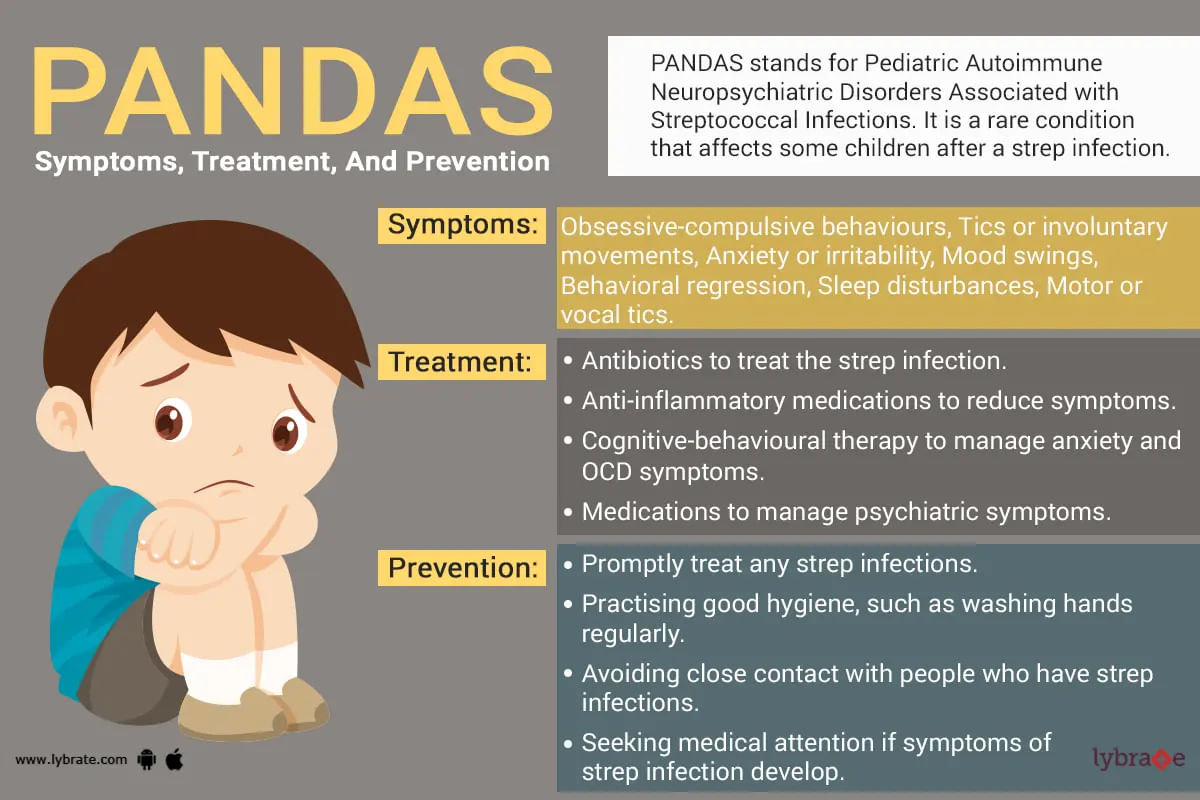
When there is pediatric streptococcal infection to children or adults, there is onset or aid in a neuropsychiatric disorder or condition called pandas (autoimmune neuropsychiatric disorders associated with streptococcus infections). Pans (pediatric acute-onset neuropsychiatric syndrome) is an umbrella under which pandas come as a subtype. Pans have many triggers and associated causes due to which different problems occur in the body. In pandas main symptoms are: ocd (obsessiv...more
673 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
1. Dr. Namadhar sharma
Https://www. Lybrate. Com/delhi/doctor/dr-namadhar-sharma-ayurveda ;
Bams, md - ayurveda
38 years experience 200 at clinic 600 online
He is a committed and skilled ayurvedic physician. Both as a general practitioner and an expert in internal medicine, he sees patients. He earned his bams from baba mastnath ayurvedic medical college in rohtak and his md in ayurveda from the institute of postgraduate t...more
186 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
This is a kind of headache which has a very severe impact on the person suffering from it and the person experiencing it can have several attacks of these occurring in a very severe fashion for a time period of 24 hours and these attacks are more likely to occur during the night time. This kind of cluster headaches are likely to happen daily for weeks or months and after sometime it is going to be on a remission but there is no surety that it will not be returning back and th...more
956 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
1. Dr. Kavitha v. Reddy ;
Https://www. Lybrate. Com/bangalore/doctor/dr-kavitha-v-reddy-general-physician
Dgo, mbbs
21 years experience 450 at clinic ;
She is a highly recognized general physician who has successfully helped several people with intricate issues. Headaches can range from mild to severe in intensity and frequency from person to person, for which the physician has a lot of experience dealing with a countless n...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Ayurvedic Doctor•Chennai
क्लस्टर सिरदर्द एक गंभीर प्रकार का सिरदर्द है। इसमें रोगी को अचानक सिर दर्द उठता है जो लगभग 24 घंटों तक बना रह सकता है।ये अधिकतर रात में होते हैं। दैनिक क्लस्टर सिरदर्द के अटैक हफ्तों या महीनों तक जारी रह सकते हैं। हालांकि इसके बाद कुछ महीनों या सालों तक इनके अटैक नहीं भी पड़ सकते हैं।
क्लस्टर सिरदर्द अन्य प्रकार के सिरदर्द से काफी भिन्न होते हैं। ये बहुत गंभीर हो सकते हैं और अक्सर इन्हें चिकित्सा प्रबंधन की आवश्यकता होती है। ये बात अलग है कि ये बहुत दर्दनाक हो सकते हैं पर क्लस्टर सिरद...more
क्लस्टर सिरदर्द अन्य प्रकार के सिरदर्द से काफी भिन्न होते हैं। ये बहुत गंभीर हो सकते हैं और अक्सर इन्हें चिकित्सा प्रबंधन की आवश्यकता होती है। ये बात अलग है कि ये बहुत दर्दनाक हो सकते हैं पर क्लस्टर सिरद...more
Book appointment with top doctors for Migraine Prophylaxis treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously