Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Menopause Health Feed
Asked for female, 47 years old from Salem
Share
Bookmark
Report
Asked for female, 58 years old from new delhi
Share
Bookmark
Report
Bachelor of Ayurveda, Medicine and Surge...read more
Ayurvedic Doctor•Zirakpur
Prasterone (intrarosa) is an intravaginal product used to treat moderate to severe dyspareunia due to vulvar and vaginal atrophy caused by menopause. The mechanism of action of intravaginal prasterone is not known, but it may involve local metabolism to estrogens and androgens. Pl talk by booking consultation slot. Simple things used with some simple efforts will be win win for you.
5 people found this helpful
Asked for female, 53 years old from Navi Mumbai
Share
Bookmark
Report
Asked for female, 28 years old from Bangalore
Share
Bookmark
Report
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Menopause is a very important phase of a women's life but before this transition phase begins there are some events that occur before the onset of the menopause and these events are said to be premenopausal events. These events are an indication that your body has started to produce less amount of estrogen than the required amount. This diminished production of this estrogen hormone leads the women to experience irregularity in their periods, further she will notice that she ...more
615 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
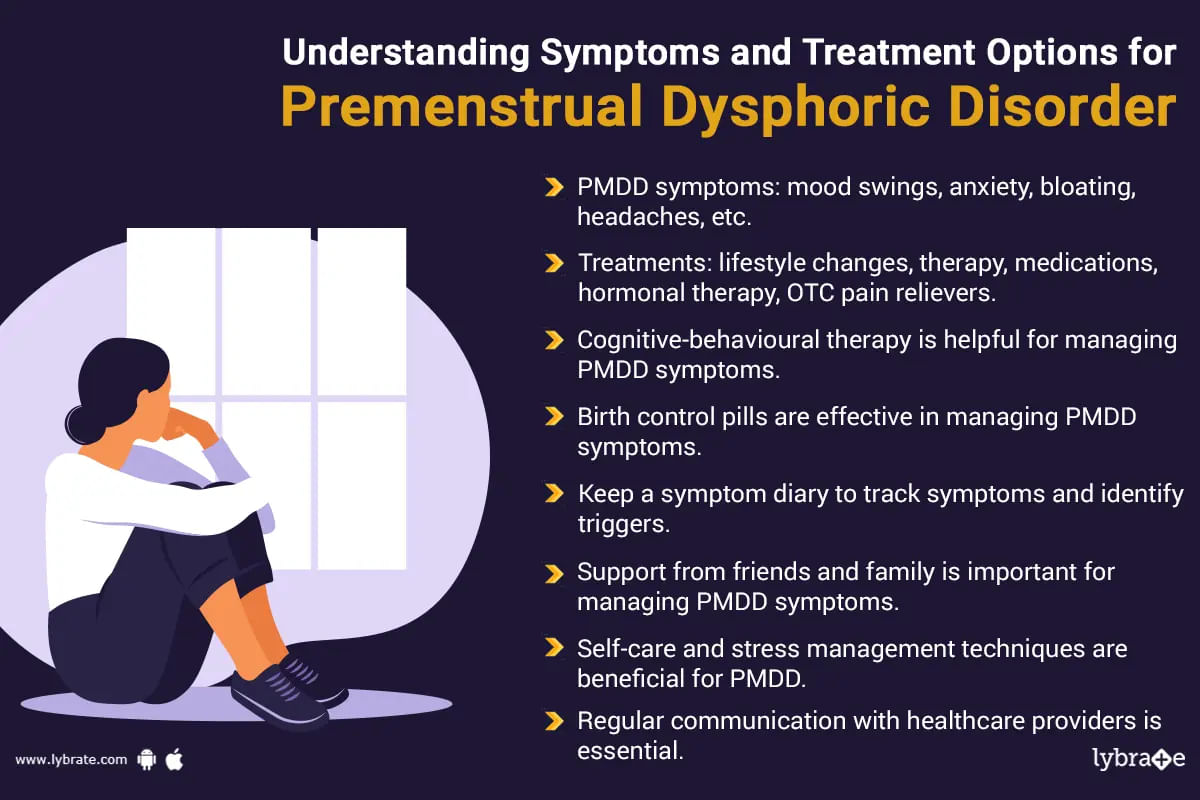
Premenstrual dysphoric disorder (pmdd) is a form of the premenstrual syndrome (pms) which occurs as a result of the disturbance of the level of hormones. Around 2 to 5 percent of the women who are about to experience the condition of menopause. The symptoms of this syndrome is somewhat similar to that of pms which means the woman will suffer from problems like fatigue, food cravings and irritability but in this case the woman will experience these symptoms in an amplified man...more
476 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
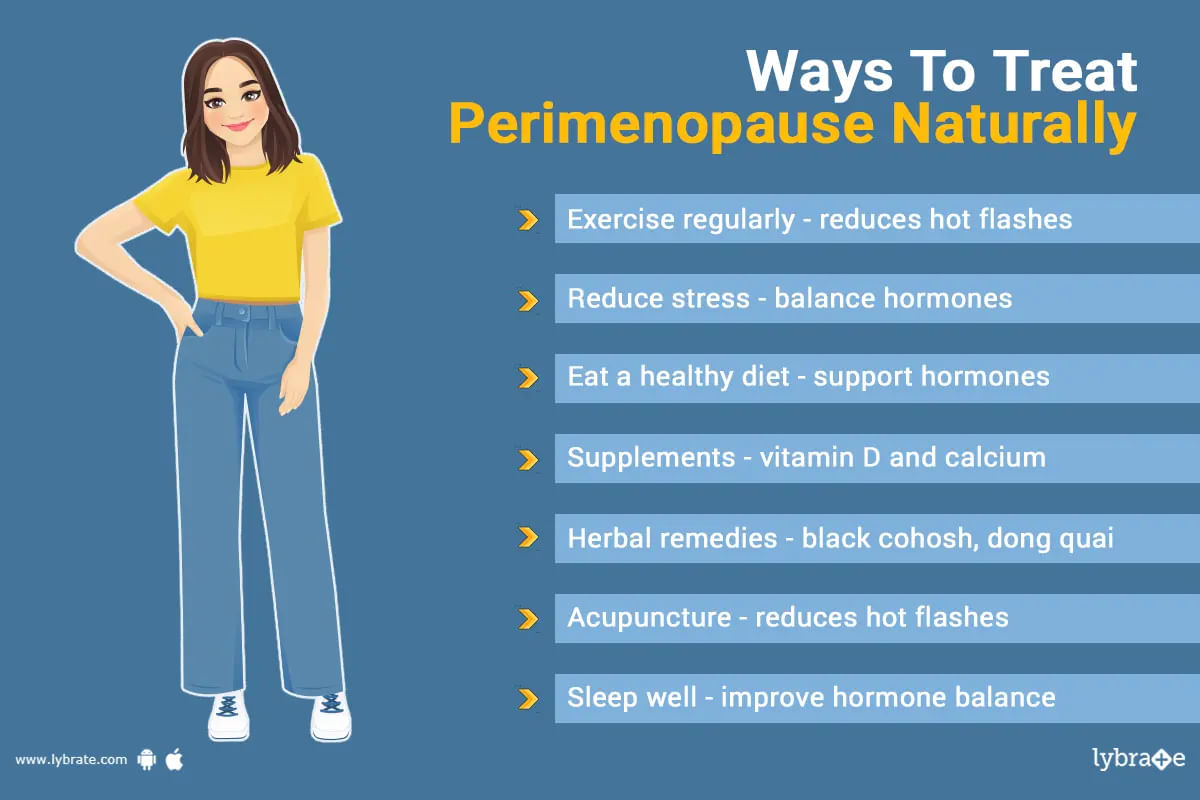
पेरिमेनोपॉज़ वह समय है जो रजोनिवृत्ति यानी मीनोपॉज के पहले से लेकर मीनोपॉज तक का होता है। इस समय के दौरान है कि लोग सबसे पहले लक्षणों का अनुभव करना शुरू करते हैं। ये लक्षण प्रोजेस्टेरोन और एस्ट्रोजन के स्तर में असंतुलन के परिणामस्वरूप होते हैं।
हालांकि हार्मोन रिप्लेसमेंट थेरेपी (एचआरटी) इन लक्षणों का इलाज करने में मदद कर सकती है, पर इस समय के लिए कोई भी महिला प्राकृतिक उपचार भी आजमा सकती है। इस लेख में कुछ प्राकृतिक उपचारों पर चर्चा होगी जो लोगों को पेरिमेनोपॉज़ के लक्षणों को प्राकृत...more
हालांकि हार्मोन रिप्लेसमेंट थेरेपी (एचआरटी) इन लक्षणों का इलाज करने में मदद कर सकती है, पर इस समय के लिए कोई भी महिला प्राकृतिक उपचार भी आजमा सकती है। इस लेख में कुछ प्राकृतिक उपचारों पर चर्चा होगी जो लोगों को पेरिमेनोपॉज़ के लक्षणों को प्राकृत...more
1430 people found this helpful
Health Query
Share
Bookmark
Report
I am sorry to hear about your concern but will be happy to assist you.
In some cases, an amount of blood will remain in the uterus after the period has ended. When this happens, the uterus contracts to remove the extra blood. These contractions can cause cramping and may also result in brown or black spotting as the old blood is pushed out.
Let's connect over a call so that we can discuss your concern in details and make a suitable treatment plan for you.
In some cases, an amount of blood will remain in the uterus after the period has ended. When this happens, the uterus contracts to remove the extra blood. These contractions can cause cramping and may also result in brown or black spotting as the old blood is pushed out.
Let's connect over a call so that we can discuss your concern in details and make a suitable treatment plan for you.
16 people found this helpful
Asked for male, 55 years old from Vadodara
Share
Bookmark
Report
I am sorry to hear about your concern but will be happy to assist you.
You may start missing periods as you approach the menopause. This is because oestrogen levels start to decrease, and ovulation becomes less regular. After the menopause, your periods stop completely.
Unprotected sex may lead to pregnancy also.
Let's connect over a call so that we can discuss your concern in details and make a suitable treatment plan for you.
You may start missing periods as you approach the menopause. This is because oestrogen levels start to decrease, and ovulation becomes less regular. After the menopause, your periods stop completely.
Unprotected sex may lead to pregnancy also.
Let's connect over a call so that we can discuss your concern in details and make a suitable treatment plan for you.
38 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Menopause is defined as stoppage of woman's menstrual cycles because of age or removal of ovaries or uterus (in few cases). This generally happens between the ages of 45-55 (mostly recorded at the age of 51). This lasts for a few years before the bleeding during the menstruation completely stops. When a woman doesn't have period for a full year (twelve months) then you can say that she has reached her full menopause.
Some women can experience perimenopause first before reaching full me...more
Some women can experience perimenopause first before reaching full me...more
365 people found this helpful
Book appointment with top doctors for Menopause treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously