Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Kidney Disease Tips
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
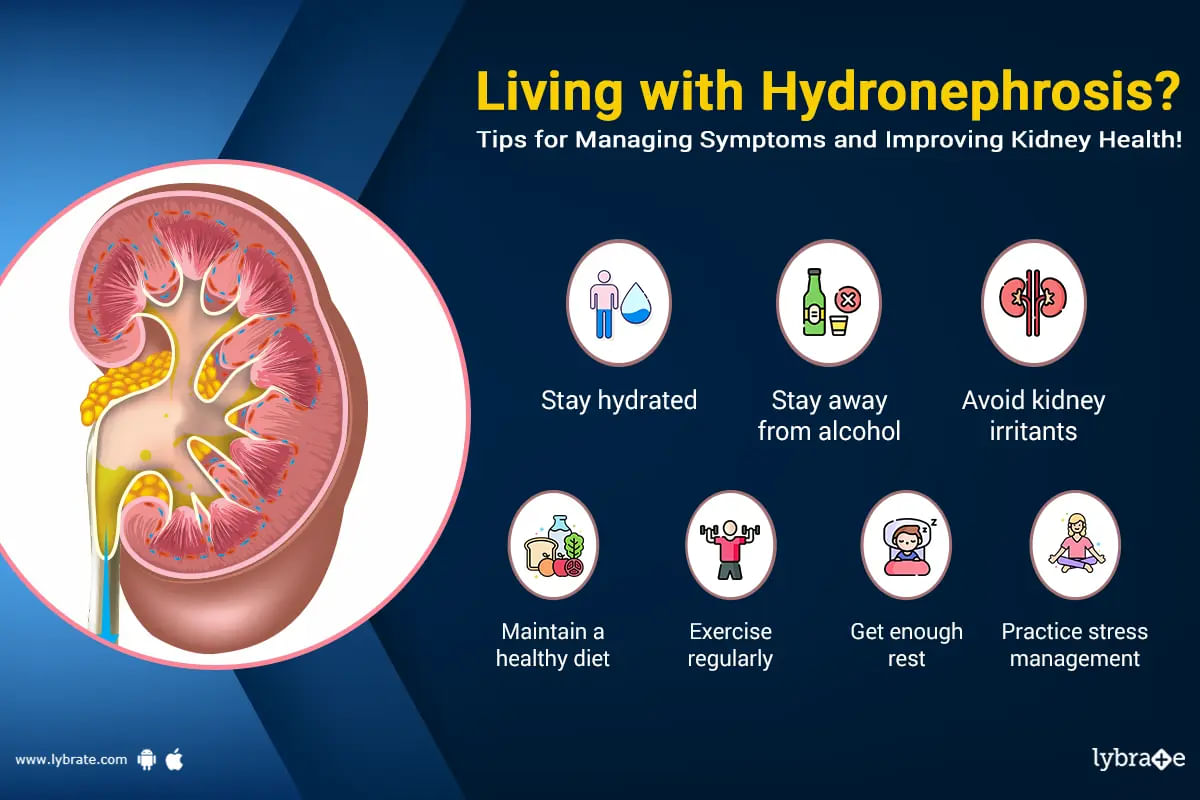
When there is swelling of one or two kidneys in the body. Inside kidney urine gets collected due to blockage of tubes. Urine stores inside when urine tubes block due to anatomical defect or stones get stuck inside. This can cause infection inside the kidney. The filtered water from the kidney is stopped by it and this whole swelling of the kidney is called hydronephrosis.
At any age this swelling called hydronephrosis can happen. Hydronephrosis is diagnosed when a ch...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
हमारे शरीर में दिल, गुर्दा, दिमाग की तरह कई तरह के भीतरी अंग होते हैं, जिनका अलग-अलग काम होता है। जब इन्ही अंगों की संरचना में कोई बदलाव आता है या उनके काम करने की क्षमता में कोई कमी आती है तो शरीर में रोग की उत्पत्ति होती है, जो विभिन्न प्रकार से जनजीवन को प्रभावित करता है।
शरीर में ऐसा ही एक अंग है किडनी, जिसका मुख्य कार्य खून को साफ़ करना और पानी व क्षार का संतुलन करके पेशाब का निर्माण करना है। लेकिन किन्ही कारणों से जब पेशाब बाहर नहीं निकल पाता और किडनी में जमा हो जाता है, तो किडनी म...more
शरीर में ऐसा ही एक अंग है किडनी, जिसका मुख्य कार्य खून को साफ़ करना और पानी व क्षार का संतुलन करके पेशाब का निर्माण करना है। लेकिन किन्ही कारणों से जब पेशाब बाहर नहीं निकल पाता और किडनी में जमा हो जाता है, तो किडनी म...more
18 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
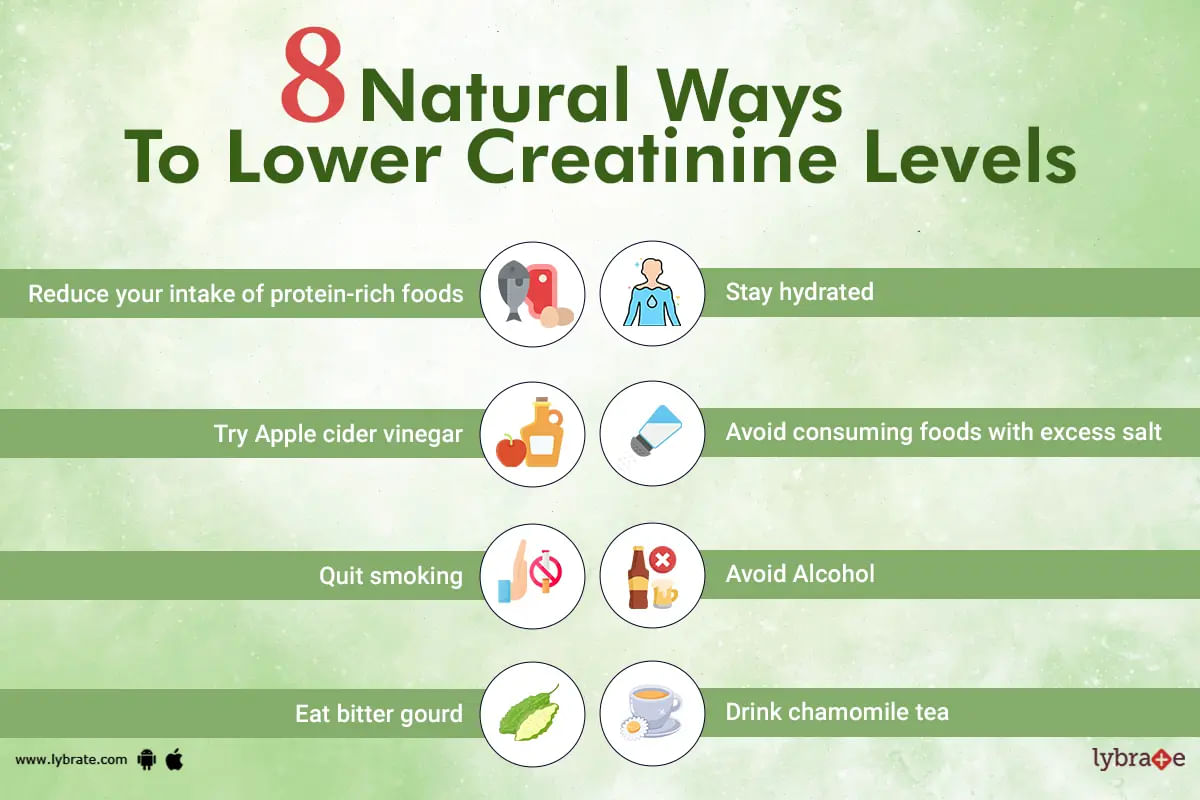
Creatinine can be best defined as an organic compound that's produced as a waste product when your muscles are used. Apart from that, eating lots of protein can also generate small amounts of creatinine in the body. In other words, creatinine is a muscle waste product that the kidneys are responsible for removing from the body and is found in a person's blood and urine.
As we already know, creatinine is a waste product that's generated from muscle metabolism. It is t...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
शरीर है जटिल मशीन
हमारा शरीर एक जटिल मशीन की तरह है जिसमें कई तरह के सिस्टम मौजूद हैं। एक रक्त संचार चलता है तो दूसरा शरीर से गंदगी बाहर निकालता है। आज हम शरीर से जहरीले कचरे को खत्म करने के लिए मौजूद तंत्र के बारे में विमर्श करेंगे।
इस तंत्र के विफल होने पर आपको उच्च क्रिएटिनिन लेवल जैसी जटिलताओं का अनुभव हो सकता है। ऐसी समस्या से गंभीर स्वास्थ्य जोखिम हो सकते हैं।
क्या आपको पता है कि उचित क्रिएटिनिन स्तर क्या है और उसे संतुलित क्यों होना चाहिए। तो इस लेख में हम इसी पर चर...more
हमारा शरीर एक जटिल मशीन की तरह है जिसमें कई तरह के सिस्टम मौजूद हैं। एक रक्त संचार चलता है तो दूसरा शरीर से गंदगी बाहर निकालता है। आज हम शरीर से जहरीले कचरे को खत्म करने के लिए मौजूद तंत्र के बारे में विमर्श करेंगे।
इस तंत्र के विफल होने पर आपको उच्च क्रिएटिनिन लेवल जैसी जटिलताओं का अनुभव हो सकता है। ऐसी समस्या से गंभीर स्वास्थ्य जोखिम हो सकते हैं।
क्या आपको पता है कि उचित क्रिएटिनिन स्तर क्या है और उसे संतुलित क्यों होना चाहिए। तो इस लेख में हम इसी पर चर...more
Last Updated: 4 years ago• Featured Tip
Share
Bookmark
Report
Most people have a bladder that can store urine until it is convenient to go to the toilet typically 4-8 times a day. Needing to rush to the bathroom more than 8 times a day or waking up in the middle of the night could mean you have been drinking too much fluid before going to bed. Technically, this condition is known as frequent urination.
However, frequent urination does not always happen when you drink up gallons of water. If you feel the urge to urinate frequently, especially at ...more
However, frequent urination does not always happen when you drink up gallons of water. If you feel the urge to urinate frequently, especially at ...more
Last Updated: 4 years ago• Featured Tip
Share
Bookmark
Report
Polycystic kidney disease (pkd) is a genetic disorder of the kidneys, where multiple ;cysts filled with fluid develop within the organ, causing it to enlarge and gradually lose its ability to function. The cysts are usually non-cancerous but differ in size. Polycystic kidney disease can harm your kidneys and cause mild to severe symptoms.
Symptoms of pkd
If multiple cysts develop in your kidney, you may experience the following symptoms
High blood pressur...more
Symptoms of pkd
If multiple cysts develop in your kidney, you may experience the following symptoms
High blood pressur...more
Last Updated: 4 years ago• Featured Tip
Share
Bookmark
Report
Kidney rupture is usually caused by a traumatic injury or direct blow to the front or sides of the abdomen, or low-to-mid back that tears or damages the organ. This type of injury is usually common in sports activities such as rugby, football, gymnastics, boxing, and horseback riding.
Renal failure or kidney rupture occurs when the kidneys stop functioning suddenly. The organ is no longer able to eliminate waste products and maintain a balance between the salt, water, and electrolytes i...more
Renal failure or kidney rupture occurs when the kidneys stop functioning suddenly. The organ is no longer able to eliminate waste products and maintain a balance between the salt, water, and electrolytes i...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
The second Thursday of March is celebrated every year as World Kidney Day. The day is marked by a global campaign aimed at increasing awareness about kidneys. In 2006 when it had initially begun, 66 countries had taken part. In 2 years, the number had gone up to 88 countries. The International Federation of Kidney Foundations (IFKF) and the International Society of Nephrology (ISN) had come together and taken the initiative to make people aware of kidney health.
What are the objectives ...more
What are the objectives ...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
General Physician•
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
The kidneys are bean-shaped organs located on either side of the spine behind the abdominal organs. Their main function is the removal of wastes from the body. On any given day, the kidneys filter out about 200 litres of blood and remove the toxins from the body via water.
In addition to this, the kidneys also produce hormones which help in vitamin D regulation and blood pressure control. Also, the red blood cell production in the bone marrow is promoted by the kidneys.
Due to ...more
In addition to this, the kidneys also produce hormones which help in vitamin D regulation and blood pressure control. Also, the red blood cell production in the bone marrow is promoted by the kidneys.
Due to ...more
Book appointment with top doctors for Kidney Disease treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously