Get the App
For Doctors
Login/Sign-up
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Interventional Diagnostic Tips
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
What is endocrine disorders?
Endocrine disorders are medical conditions that affect the body's endocrine system.
Many symptoms, including exhaustion, weight gain, and changes in mood or appetite, might be brought on by them.
Endocrine disorders may be caused by a number of factors, including genetics, environmental exposure, and other medical conditions.
Types of endocrine disorder:
Diabetes mellitus: it is a chronic disorder tha...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
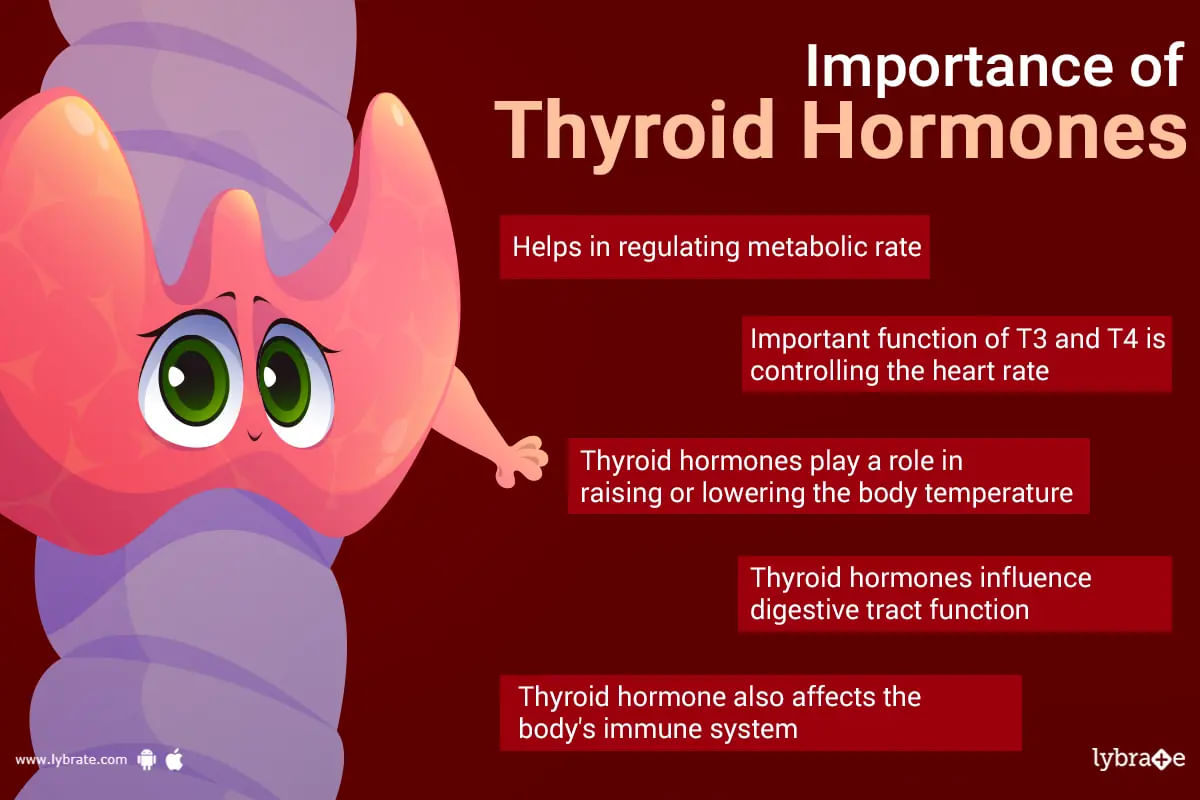
The thyroid gland produces thyroid hormone, which is essential for controlling the body's energy and metabolism. It is a type of hormone that is responsible for many important functions in the body, such as controlling the body's temperature, heart rate, and maintaining healthy levels of calcium in the blood. The body can become unbalanced as a result of the thyroid gland producing too much or too little thyroid hormone, which can result in a variety of symptoms and health is...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
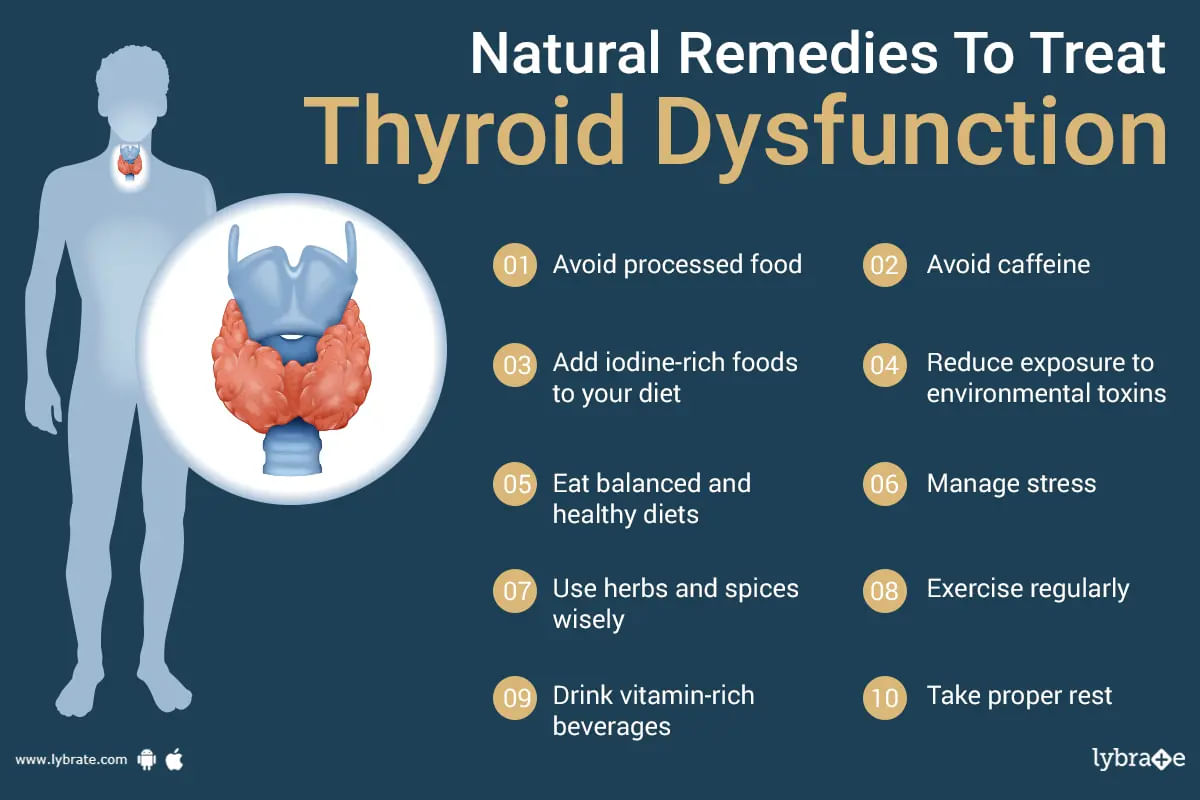
What is thyroid dysfunction?
Thyroid dysfunction, also known as hypothyroidism or hyperthyroidism, is a medical condition where the thyroid gland does not produce enough thyroid hormones or produces more than the body needs.
Hypothyroidism is the most common type of thyroid dysfunction and occurs when there is too little production of thyroid hormones. Hyperthyroidism occurs when there is too much production of these hormones. ;
Thyroid dysfunction can be ca...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Endocrinologist•Hyderabad
1. Dr. Bharath r ;
Https://www. Lybrate. Com/chennai/doctor/dr-bharath-r-endocrinologist-2
Mbbs, md - (medicine - endocrinology)
23 years experience 0 - 500 at clinic
;
He is a well regarded doctor who has helped numerous people with tough conditions. As an endocrinologist, his name is familiar. His impressive credentials include a mbbs from tirunelveli medical college and a md in endocrinology from king georges medical coll...more
232 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
1. Dr. Priya mani
Https://www. Lybrate. Com/bangalore/doctor/dr-priya-mani-endocrinologist
Mbbs, fellowship in diabetology ;
21 years experience 600 at clinic
She is a well regarded physician who has successfully helped a lot of people with intricate problems during her career. Both as an endocrinologist and a diabetologist, she is well qualified. She completed her illustrious mbbs programme at kims chennai. Her fellowship in diabete...more
126 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
1. Dr. Monashis sahu ;
Https://www. Lybrate. Com/delhi/doctor/dr-monashis-sahu-endocrinologist
Dm - endocrinology, md - medicine, mbbs
21 years experience 1200 at clinic
He is a well-respected doctor who is a specialist in endocrinology having a number of patients treated with hormonal issues. He has extensive experience in treating thyroid-related problems which usually have various types of symptoms such as obesity, under...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
1. Dr. Anantharaman ramakrishnan
Https://www. Lybrate. Com/bangalore/doctor/dr-anantharaman-ramakrishnan-endocrinologist
Mbbs, md - general medicine, d. M. - endocrinology
;
Dr. Anantharaman ramakrishnan is widely regarded as one of the most qualified endocrinologists in the b. T. M. Layout area of bangalore. He has nineteen years of experience working as an endocrinologist. He received his education and his d. M. In endocrinology, mbbs, and m. D. ...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Endocrinologist•
There is an effect named the'butterfly effect. This effect generally talks about how everything is connected to each other and a very small change caused in the starting point will create some serious issues at the end. The same effect can be observed in the case of our thyroid gland. Thyroid gland of our body is considered as the master of our metabolism. The activities (crucial body functions) controlled by the production of hormones from this gland are regulation of temper...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
थायरायड की बीमारी आजकल इतनी आम हो चुकी है कि हर दूसरा व्यक्ति इस रोग से ग्रसित है। किसी को हायपो थायरॉयड है या हाइपर थायरायड से जूझ रहा है।दरअसल थायरायड की ग्रंथि शरीर के बेहद मह्तवपूर्ण समन्वय को बनाए रखने के लिए काम करती है। कई ऐसे कारण होते हैं जो इस समन्वय को बिगाड़ सकते हैं। जब थायरॉयड ग्रंथि कम मात्रा में थायराइड हार्मोन का उत्पादन करती है, तो इसे हाइपोथायरायडिज्म के रूप में जाना जाता है। थायराइड हार्मोन कम होने से व्यक्ति सुस्त महसूस करता है, इसका वजन बढञने लगता है,शरी...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Dermatologist•Delhi
Hypertension is a killer disease whose symptoms develop late when the damage is in advanced stages. Hypertensive Retinopathy is one such disease.
It damages the retina of eyes. Since retina is responsible for vision formation, Hypertensive Retinopathy can result in loss of vision. It is of grave concern that in most cases, Hypertensive Retinopathy is diagnosed later.
This is due to the fact that there are often no symptoms in the early stages of the disease. In some cases, wher...more
It damages the retina of eyes. Since retina is responsible for vision formation, Hypertensive Retinopathy can result in loss of vision. It is of grave concern that in most cases, Hypertensive Retinopathy is diagnosed later.
This is due to the fact that there are often no symptoms in the early stages of the disease. In some cases, wher...more
Book appointment with top doctors for Interventional Diagnostic treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously