Get the App
For Doctors
Login/Sign-up
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Implant Rehabilitation Tips
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Cochlear Implant is an electronic device replaced with the inner ear (cochlea) of the patients who are unable to send sound waves to the brain.
The surgery is performed on the patients who have the problem of hearing loss due to the damaged hair cells in the inner ears. The implant helps the patient to hear which are not responding to other hearing aids.
Conditions for Cochlear Implant:
Cochlear implants help people to hear with clarity. They are not like hearing aids,...more
The surgery is performed on the patients who have the problem of hearing loss due to the damaged hair cells in the inner ears. The implant helps the patient to hear which are not responding to other hearing aids.
Conditions for Cochlear Implant:
Cochlear implants help people to hear with clarity. They are not like hearing aids,...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
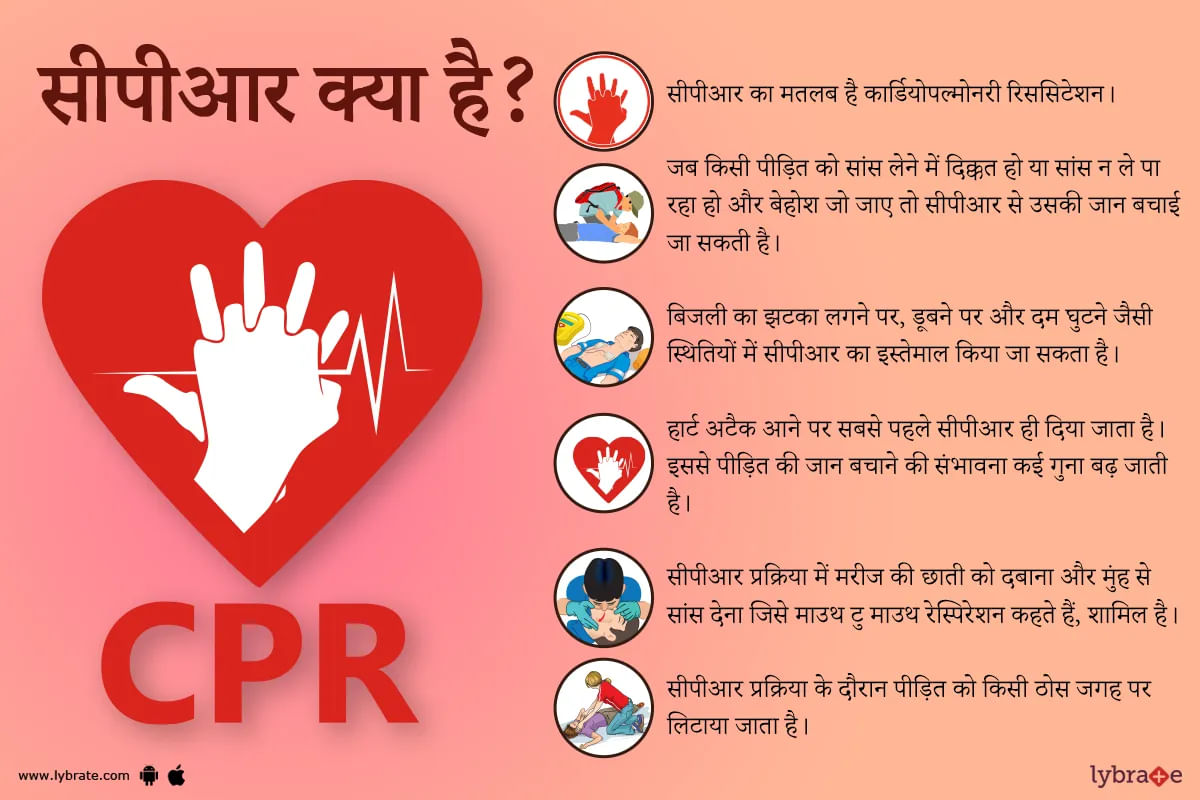
सीपीआर का मतलब है कार्डियोपल्मोनरी रिससिटेशन। यह भी एक तरह की प्राथमिक चिकित्सा यानी फर्स्ट एड है। जब किसी पीड़ित को सांस लेने में दिक्कत हो या फिर वो सांस न ले पा रहा हो और बेहोश जो जाए तो सीपीआर से उसकी जान बचाई जा सकती है। बिजली का झटका लगने पर, पानी में डूबने पर और दम घुटने पर सीपीआर से पीड़ित को आराम पहुंचाया जा सकता है। हार्ट अटैक यानी दिल का दौरा पड़ने पर तो सबसे पहले और समय पर सीपीआर दे दिया जाय तो पीड़ित की जान बचाने की संभावना कई गुना बढ़ जाती है।
अगर किसी...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
General Surgeon•
1. Dr. Muthuraju k r
Https://www. Lybrate. Com/bangalore/doctor/dr-muthuraju-k-r-general-surgeon
;
Mbbs, ms, gastro-intestinal, bariatric and metabolic surgery
21 years experience 0 at clinic
As an experienced and skilled surgeon, he has assisted a great number of patients and is currently working with vulnerable patients who have suffered from myocardial infarction, systemic hypertension, and illnesses such as arteriosclerosis and oth...more
Https://www. Lybrate. Com/bangalore/doctor/dr-muthuraju-k-r-general-surgeon
;
Mbbs, ms, gastro-intestinal, bariatric and metabolic surgery
21 years experience 0 at clinic
As an experienced and skilled surgeon, he has assisted a great number of patients and is currently working with vulnerable patients who have suffered from myocardial infarction, systemic hypertension, and illnesses such as arteriosclerosis and oth...more
12 people found this helpful
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Hair loss is a very common cause of the problem for both men and women. One in four women suffers from some degree of hair loss or thinning hair. In men, balding can begin as early as the age of 21 and by the age of 35, 30% of men will already be experiencing noticeable balding.
All of us suffer from hair fall daily, but only when it becomes an area of concern is when it starts resulting in baldness and thinning of hair. In such cases, the patient becomes increasingly concerned about th...more
All of us suffer from hair fall daily, but only when it becomes an area of concern is when it starts resulting in baldness and thinning of hair. In such cases, the patient becomes increasingly concerned about th...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Our endocrine glands work overtime to keep us healthy by secreting hormones which reach each and every cell in our body through the blood. These hormones evoke life-changing responses in other cells to keep us alive and healthy. Endocrine surgery is a term for an operation in any one or more endocrine glands in your body.
Types of endocrine glands-
1. Thyroid gland: This is the most important endocrine gland in your body and it secretes thyroid hormone, which regulates metabol...more
Types of endocrine glands-
1. Thyroid gland: This is the most important endocrine gland in your body and it secretes thyroid hormone, which regulates metabol...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Multi Speciality•Gorakhpur
Weight loss surgery or bariatric surgery is an effective treatment procedure for people, who are morbidly obese, i.e. a person weighing 100 pounds over his/her ideal body weight or having BMI (body mass index) higher than 40. One of the major reasons for the increasing trend of obesity is overconsumption of unhealthy food. This combined with lack of physical activity and a sedentary lifestyle leads to the accumulation of excess calories in the body.
Who Needs Bariatric Surgery?
more
Who Needs Bariatric Surgery?
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Pelvic Inflammatory Disease is a common infection in the female reproductive organs like the ovaries, the uterus and the fallopian tubes and also the inside of the pelvis. If left untreated for a long time, PID can lead to severe problems like pregnancy complications, infertility and cancer.
Causes
Sexually Transmitted Diseases (STD) like chlamydia and gonorrhea produce vaginal bacteria which travel to the interior organs and cause PID. Having unprotected sexual contact with so...more
Causes
Sexually Transmitted Diseases (STD) like chlamydia and gonorrhea produce vaginal bacteria which travel to the interior organs and cause PID. Having unprotected sexual contact with so...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Obesity surgery is more commonly referred to as bariatric surgery. It is a surgery done on the stomach and/or intestines of a person with morbid obesity so that he or she loses weight. It is believed that as of now, bariatric surgery is the only option that almost always works to help overly obese people lose a lot of weight, which automatically makes the associated chronic conditions vanish.
How does this surgery work? Bariatric surgery works by changing the anatomy of the stomach and ...more
How does this surgery work? Bariatric surgery works by changing the anatomy of the stomach and ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The word acute coronary syndrome refers to a group of symptoms that are caused by blockage of the blood flow to the heart muscles. The most common result of this is myocardial infarction or heart attack as it is popularly called. Reduced blood flow leads to death of some portion of the heart muscle wall. While the word heart attack sounds almost fatal, it need not be the case. Knowing how to identify an attack and being aware of some simple measures can help save lives.
Symptoms: The...more
Symptoms: The...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Coronary artery disease is one of the major killer diseases of modern society. It is not a solitary problem but brings with it a multitude of issues including obesity, diabetes, stroke, and other metabolic disorders. A thorough understanding of what causes it and how to manage it can help save thousands of lives.
Causes: The circulatory system is mainly made up of the heart and a complex network of arteries and veins. The inner walls of these are lined with smooth muscles, allowing for ...more
Causes: The circulatory system is mainly made up of the heart and a complex network of arteries and veins. The inner walls of these are lined with smooth muscles, allowing for ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The Breast implants, be it the saline or the silicone implants comes as a blessing for people who have struggled for ages with a small breast. From lifting your self-confidence to enhancing the overall appearance, the benefits of breast implants are immense. However, there are some myths associated with the breast implants that should be busted for people to understand the procedure better.
Myth: The breast implants produce the same results in all individuals.
Fact: This myth is as ...more
Myth: The breast implants produce the same results in all individuals.
Fact: This myth is as ...more
Book appointment with top doctors for Implant Rehabilitation treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously