Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
HIV AIDS Tips
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
DM INFECTIOUS DISEASE, MD, MBBS Bachelor...read more
Infectious Disease Physician•Delhi
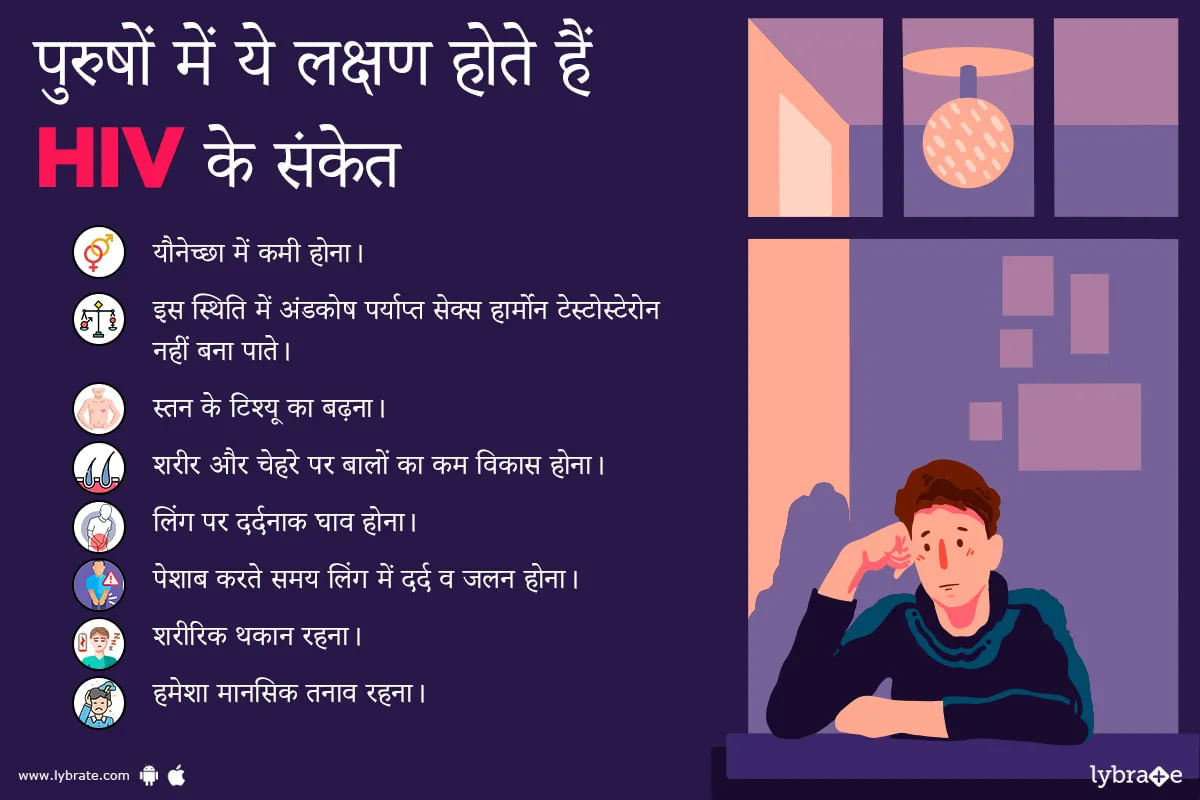
एचआईवी यानी ह्युमन इम्युनोडेफिशिएंसी वायरस एक ऐसा वायरस है जो मनुष्य की प्रतिरक्षा प्रणाली को प्रभावित करता है। चूंकि यह वायरस प्रतिरक्षा प्रणाली पर ही हमला करता है इसलिए हमारी प्रतिरक्षा प्रणाली इस वायरस के खिलाफ रक्षात्मक प्रतिक्रिया करने में सक्षम नहीं है। इसका यह अर्थ है कि एचआईवी से पीड़ित व्यक्ति अन्य संक्रमणों और बीमारियों के प्रति अधिक संवेदनशील होता है।
एचआईवी एक संक्रमित व्यक्ति से दूसरे व्यक्ति में रक्त, वीर्य, या योनि के तरल पदार्थ के संपर्क में आने से फै...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
The acronym for 'Acquired Immune Deficiency Syndrome' is AIDS. In fact, it must be understood that AIDS is not a singular disease, but a syndrome, or rather a set of diseases. People suffering from AIDS suffer from an immensely compromised immune system that makes them vulnerable to a number of diseases. Once infected with HIV, it may take anywhere between 5-10 years to develop AIDS.
Some of the major symptoms of AIDS are:
Lethargy and fatigue
Skin irritation
Drastic lo...more
Some of the major symptoms of AIDS are:
Lethargy and fatigue
Skin irritation
Drastic lo...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
What aids in best results after your hip replacement?
Practising these recovery tips will help you to have a smooth and successful recovery.
1-get in a healthy exercise routine
Most hip replacement patients are able to walk within the same day or next day of surgery; most can resume normal routine activities within the first 3 to 6 weeks of their total hip replacement recovery.
Once light activity becomes possible, it's important to incorporate healthy exercise in...more
Practising these recovery tips will help you to have a smooth and successful recovery.
1-get in a healthy exercise routine
Most hip replacement patients are able to walk within the same day or next day of surgery; most can resume normal routine activities within the first 3 to 6 weeks of their total hip replacement recovery.
Once light activity becomes possible, it's important to incorporate healthy exercise in...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
MD - Internal Medicine, MBBS, Nephrology...read more
General Physician•Roorkee
HIV and tuberculosis (TB) are two life-threatening and common diseases in the world. The two diseases are very closely connected so much so that their occurrence is normally labelled as a co-epidemic. In most cases tuberculosis is found to be the most transmissible contagion in HIV-Immunocompromised victims, proving to be the cause of their death.
What is HIV?
Human Immunodeficiency Virus, more commonly known by its abbreviation HIV, is a virus that attacks the immune system, which ...more
What is HIV?
Human Immunodeficiency Virus, more commonly known by its abbreviation HIV, is a virus that attacks the immune system, which ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Oral sex is a form of sexual activity, which involves the arousal of one's genitalia by his/her partner using the mouth (tongue, lips and throat). It is also called Cunnilingus (performed on a female) and fellatio (performed on a male). It is done before intercourse and during foreplay for sexual arousal. It is safe as compared to vaginal or anal sex, the rate of getting a sexually transmitted disease or HIV is comparatively lower.
Oral sex can spice up your life and can also make your...more
Oral sex can spice up your life and can also make your...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The general acceptance is that, when someone suffers from Sexually Transmitted Disease or STD, the risk of getting affected by HIV increases for that particular person. This is true for both biological as well as for behavioral reasons.
HIV is one of the diseases which are caused as a result of sexual transmission. Before knowing the exact link between HIV and STD, understanding what the two concepts exactly are, would be beneficial.
Let us now look at the two concepts in detai...more
HIV is one of the diseases which are caused as a result of sexual transmission. Before knowing the exact link between HIV and STD, understanding what the two concepts exactly are, would be beneficial.
Let us now look at the two concepts in detai...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
A healthy immune system and optimum physical strength is maintained by an adequate nutritional status of the body. Unexpected loss of weight, loss of appetite, low dietary intake due to ulcers in the mouth and an altered rate of metabolism are common in HIV infected individuals. It is essential to regain the lost weight and the muscle mass in the early stages of the infection since the correction of nutritional status becomes difficult with the progression of the disease.
Certain measur...more
Certain measur...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Dentist•Mumbai
HIV is a systemic disease which affects all parts of the body. The oral cavity also has some tell-tale symptoms which indicate HIV / AIDS. A careful examination and detailed history of symptoms is essential. In some cases, the oral manifestations could be the area where HIV is suspected. This can help in reducing morbidity and improves prognosis. The oral lesions that occur in HIV patients can vary and differ significantly in children and adults. While there are a variety of oral lesions in HIV-...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The human immunodeficiency virus (HIV) is a subgroup of retrovirus (lentivirus) that causes HIV infection. After a period of time, this infection leads to what is called acquired immunodeficiency syndrome (AIDS).
Epidemiology
According to the Centers for Disease Control and Prevention (CDC), from 2010-2015, the estimated rate of HIV infection in all 50 US states decreased from 14.2 per 100,000 population in 2010 to 12.3 per 100,000 population in 2015. In 2015, 39,513 individual...more
Epidemiology
According to the Centers for Disease Control and Prevention (CDC), from 2010-2015, the estimated rate of HIV infection in all 50 US states decreased from 14.2 per 100,000 population in 2010 to 12.3 per 100,000 population in 2015. In 2015, 39,513 individual...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
MBBS, DNB (Orthopedics), Diploma in Orth...read more
Orthopedic Doctor•Hyderabad
Old age or certain medical conditions may cause osteoporosis. In such conditions, one needs to be cautious as even the smallest of falls can cause fractures which may render the patient bed-ridden. Here are a few tips to how you can prevent hip fracture.
Read on to find out more about the prevention of hip fracture.
Preventing falls: People over the age of 65 have a higher risk of falling due to various causes. To reduce such risks one should take the help of walking aids such ...more
Read on to find out more about the prevention of hip fracture.
Preventing falls: People over the age of 65 have a higher risk of falling due to various causes. To reduce such risks one should take the help of walking aids such ...more
Book appointment with top doctors for HIV AIDS treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously