Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Heart Failure Tips
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Cardiac arrest is reported to be the number one cause of sudden death for people over the age of 40. As it strikes fast and without prior warning, it usually leaves no time for getting help to the patient. Many lives can be saved if the necessary first aid is given immediately by people who know what to do in case of a cardiac arrest.
So first let us know about the signs of a cardiac arrest:
Loss of consciousness: A person may feel dizzy, sweat, faint or collapse suddenly. You ...more
So first let us know about the signs of a cardiac arrest:
Loss of consciousness: A person may feel dizzy, sweat, faint or collapse suddenly. You ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
You must have heard this very often that drinking alcohol can lead to heart problems or even a heart attack, but you might not be sure how this is exactly explained. There is no doubt that consuming anything in excess can lead to serious health issues. Interestingly experts invariably mention that a drink or two every day keeps your heart healthy and can even prevent a stroke from occurring. So how does this gel with the conclusion that alcohol is not good for your heart?
It starts wit...more
It starts wit...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
All healthy individuals will always have some amount of urea in the blood. Yet, when the urea level in the blood becomes too high, that means there is a malfunction in some part of the body due to which the body is not being able to remove this excess urea successfully. This urea can be formed in the liver when there is a process in terms of the protein metabolism's chemical balance. This urea is then transported to various parts of the body until the kidney cleans it out as urine. But when this...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Congestive heart failure is a chronic progressive condition that affects the pumping power of your heart muscles. Simply referred to as heart failure, congestive heart failure can be life-threatening. It does not mean that the heart has stopped working. Rather, it means that the heart pumping power is weaker than normal. As a result, the heart cannot pump enough oxygen and nutrients to meet the body s needs. Over a period of time, the reduced ability of the heart causes the organs to receive les...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The heart is a vital organ that pumps blood throughout the body, thereby supplying the body with the essential nutrients and oxygen while removing the harmful toxins and wastes. Certain conditions may interfere with the ability of the heart to pump blood (there could be clogging in one of the artery or arteries). Devoid of blood and the essential nutrients, the other vital organs soon start to falter. In fact, reduced supply of oxygen and blood to the brain can prove to be fatal, triggering loss...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Multi Speciality•Nagpur
Heart failure, which is also known as congestive heart failure, occurs when the heart muscle fails to pump sufficient blood as well as it should. The narrowed arteries in one s heart or high blood pressure make the heart too weak to pump sufficient blood into the system. Heart failure can be prevented if people are aware of how to keep a check on the conditions which cause failure of the heart, like high blood pressure, diabetes, obesity.
Symptoms
Heart failure can be of two ty...more
Symptoms
Heart failure can be of two ty...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Blockage in heart is a common term used for narrowing of coronary arteries. Coronary arteries are vessels, which supply blood and thus oxygen and food to continuously working heart muscles. Heart muscles, which are not tired working from the birth till death, however, cannot sustain long without blood supply.
A reduction in blood supply gives rise to ischemia of heart muscles commonly manifested as chest discomfort or angina. A sudden complete shutdown of blood supply leads to heart att...more
A reduction in blood supply gives rise to ischemia of heart muscles commonly manifested as chest discomfort or angina. A sudden complete shutdown of blood supply leads to heart att...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Cardiac arrest is reported to be the number one cause of sudden death for people over the age of 40. As it strikes fast and without prior warning, it usually leaves no time for getting help to the patient. Many lives can be saved if the necessary first aid is given immediately by people who know what to do in case of a cardiac arrest.
So first let us know about the signs of a cardiac arrest:
Loss of consciousness: A person may feel dizzy, sweat, faint or collapse suddenly. You ...more
So first let us know about the signs of a cardiac arrest:
Loss of consciousness: A person may feel dizzy, sweat, faint or collapse suddenly. You ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
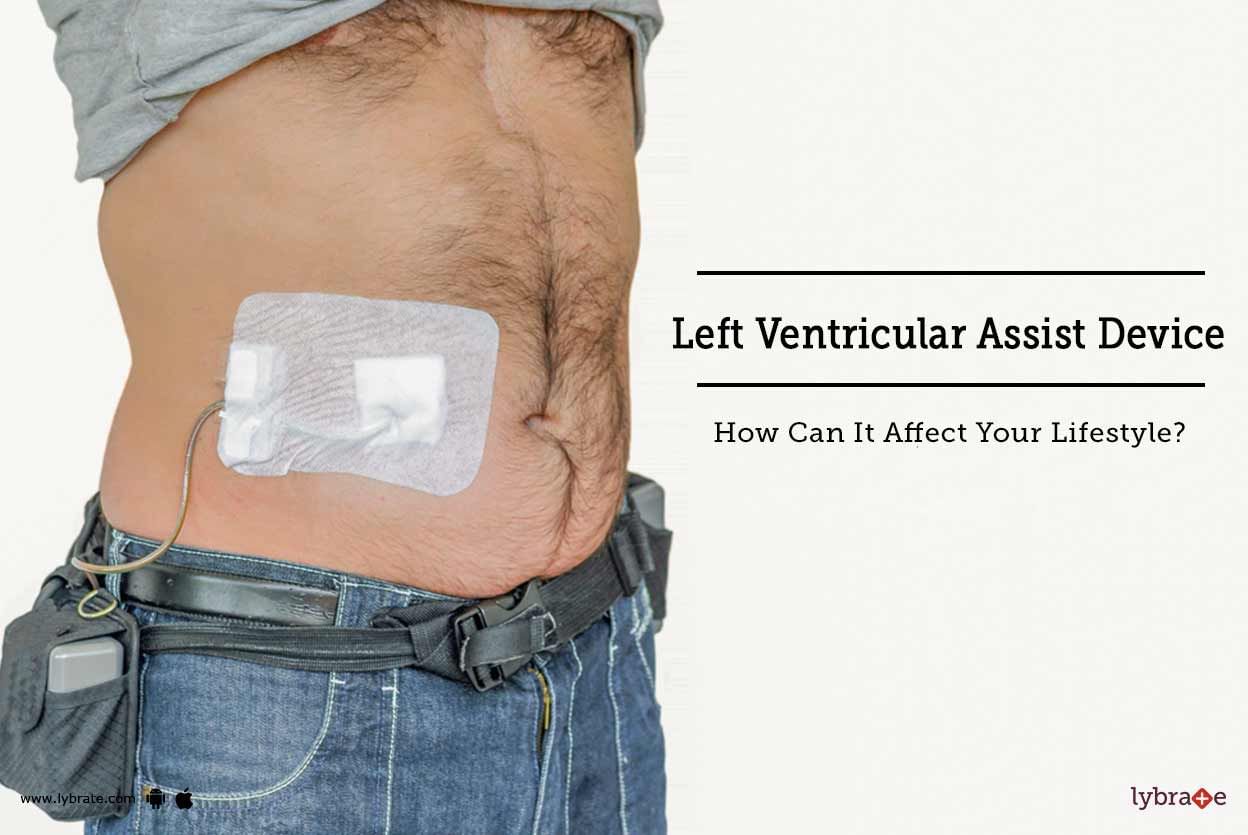
A left ventricular assist device is an electromechanical device used in cases of advanced heart failure. In later stages of heart failure when the heart is weakened and no longer able to pump the necessary amount of blood, a left ventricular assist device can be surgically implanted to assist the heart s functions.
A left ventricular assist device is often used as a short term solution and is different from a pacemaker, which is a long term cardiac assist device. The cases in which a le...more
A left ventricular assist device is often used as a short term solution and is different from a pacemaker, which is a long term cardiac assist device. The cases in which a le...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Our survival is solely reliant on the working of the heart. It is this that makes the prospect of a heart failure so fatal and so terrifying. Notwithstanding what the heart evokes, a heart failure is not indicative of a defunct heart; but only a situation when the heart pumps weaker than what is generally deemed as natural. Consequently, the blood flows at a slower rate to the heart and the body that in turn increases pressure in the heart. The oxygen that is produced by the heart in such a scen...more
Book appointment with top doctors for Heart Failure treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously