Get the App
For Doctors
Login/Sign-up
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Heart Disease By Birth Tips
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
MBBS, MD - Paediatrics, FNB Pediatric Ca...read more
Pediatric Cardiologist•Delhi
If a child is suffering from a congenital heart defect, it means that the child is born with a heart defect. Some of the heart problems are simple and don t need treatment, while some are very complex and may need multiple surgeries depending on the prevailing heart condition.
Symptoms of Heart Defects-
The symptoms in children with serious heart defects depend on the type of congenital heart disease. Symptoms that a child can show are:
Breathing problem while feedi...more
Symptoms of Heart Defects-
The symptoms in children with serious heart defects depend on the type of congenital heart disease. Symptoms that a child can show are:
Breathing problem while feedi...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Ever wondered why you needed to share your family s health history at a doctor s clinic? Specific questions regarding health issues of your immediate family or close blood relatives give your doctor an insight into various health risks you might have now or in future. Those are medical conditions inherited by parents or grandparents through genes. Genes are passed from parents to children in DNA of eggs or sperms. Even a single mutation (fault) in gene can influence body systems and may lead to ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
MBBS, MD - Paediatrics, FNB Pediatric Ca...read more
Pediatric Cardiologist•Delhi
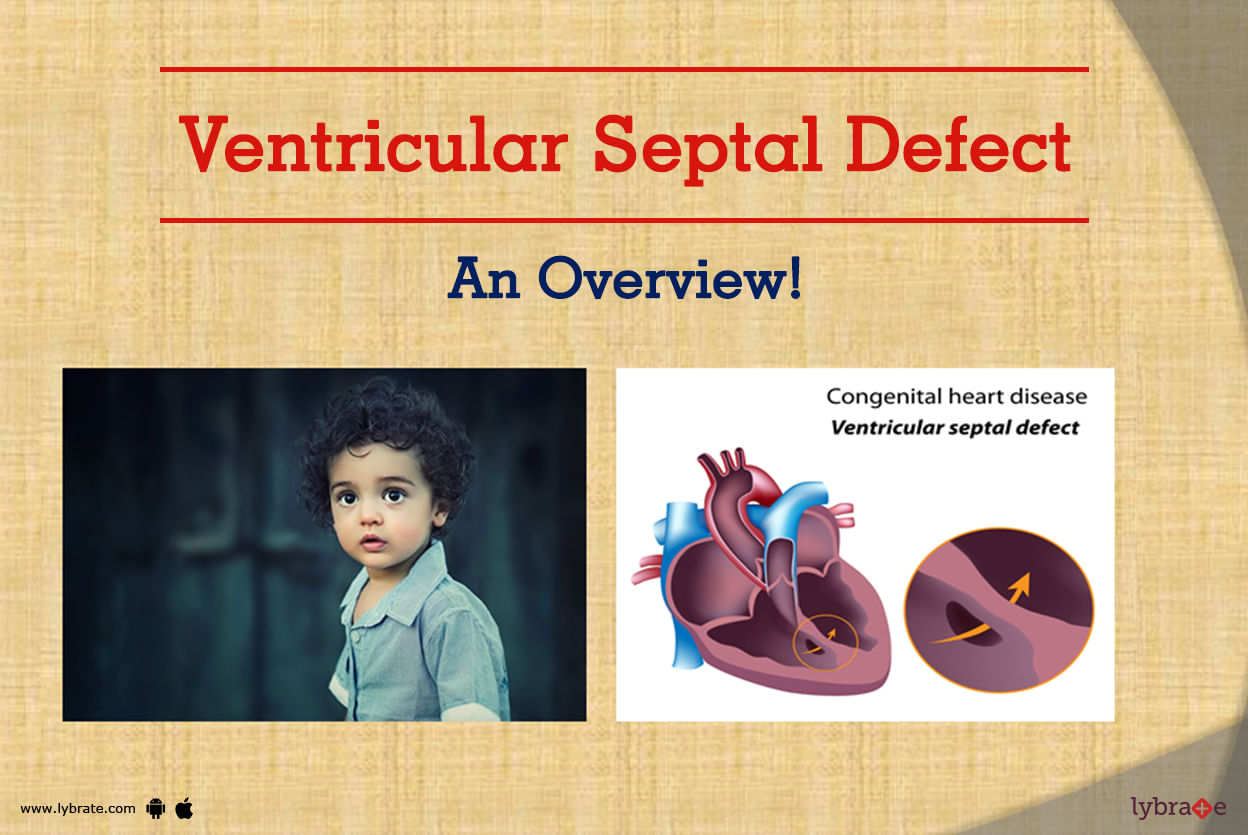
VSD (a hole in the heart) refers to a congenital heart disease where a hole is formed in the ventricle septum i.e. wall between two lower chambers of the heart. As a result of this, blood from the left portion of the heart (left ventricle) crosses this hole and goes to right-sided heart that results in blood overflow to lungs.
VSD is one of the commonest child heart diseases that is seen at birth, but adults too may suffer from it following an acute heart attack.
What are the causes...more
VSD is one of the commonest child heart diseases that is seen at birth, but adults too may suffer from it following an acute heart attack.
What are the causes...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
While you may be worried about being affected with coronary diseases just because your forefathers suffered from it, there are various factors that are absolutely in your sole control. With a little change in lifestyle and following a well-regulated routine, you can easily keep your hereditary cardiac diseases at bay.
Take a Healthy Diet Regularly: Increase the amount of green leafy vegetables and colourful fruits in your regular diet as they are rich in phytonutrients and other anti-ox...more
Take a Healthy Diet Regularly: Increase the amount of green leafy vegetables and colourful fruits in your regular diet as they are rich in phytonutrients and other anti-ox...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
MBBS, MD - Paediatrics, FNB Pediatric Ca...read more
Pediatric Cardiologist•Delhi
While every parent wants their children to be born healthy, some infants have a range of disorders present at the time of birth.
Patent Ductus Arteriosus or PDA is one such condition that manifests in children when they are born.
Here is all you need to know about Patent Ductus Arteriosus (PDA).
What is PDA?
PDA is the opening between the two major blood vessels leaving from the human heart. The ductus arteriosus is an essential part of a child s circulatory system befo...more
Patent Ductus Arteriosus or PDA is one such condition that manifests in children when they are born.
Here is all you need to know about Patent Ductus Arteriosus (PDA).
What is PDA?
PDA is the opening between the two major blood vessels leaving from the human heart. The ductus arteriosus is an essential part of a child s circulatory system befo...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
MBBS, MD - Paediatrics, FNB Pediatric Ca...read more
Pediatric Cardiologist•Delhi
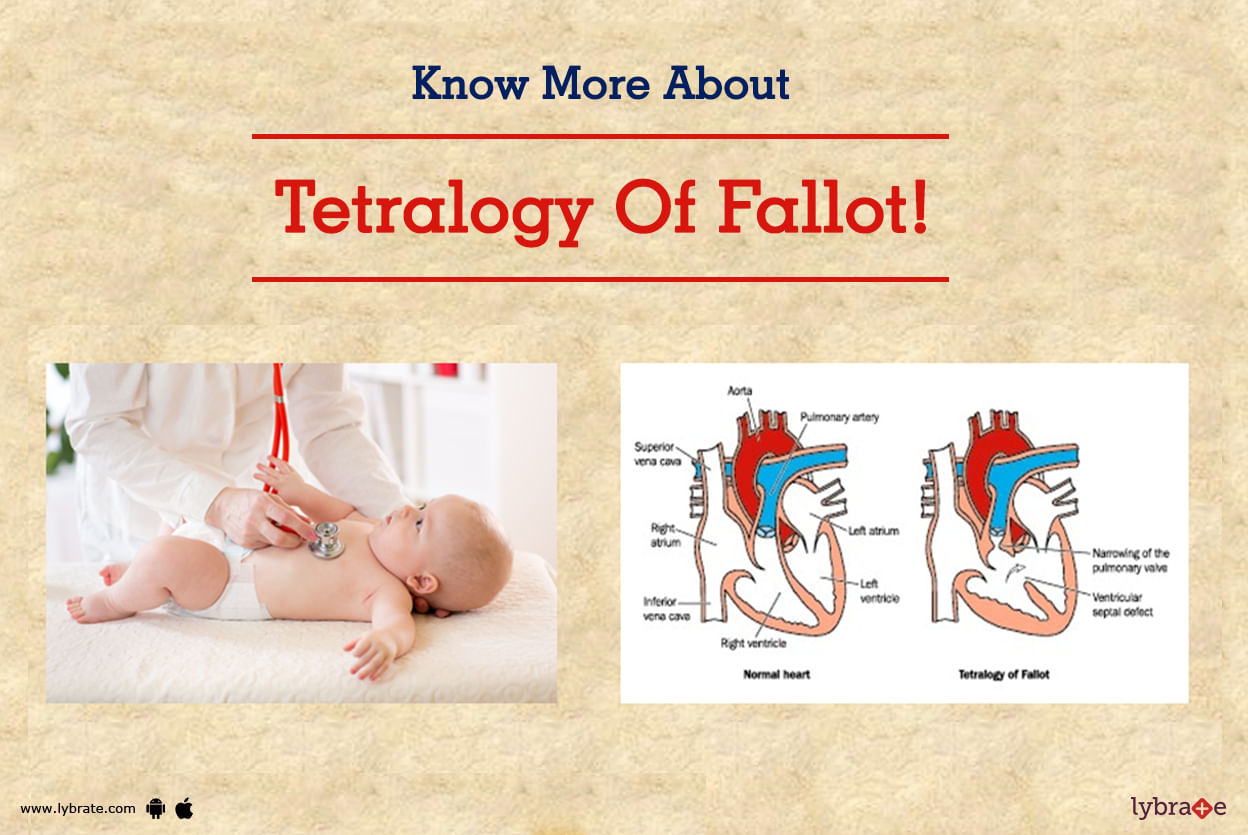
Tetralogy of Fallot (TOF) is a commonest congenital cyanotic heart disease.
TOF is having a combination of large VSD with severe obstruction of blood flow to the lungs that result in bluish-black discoloration of lips and fingers due to flow of oxygen-deficit blood to the body parts.
The four defects that commonly associated with Tetralogy of Fallot (TOF) are
Ventricular Septal Defect (VSD) a hole formed in ventricular septum that is situated between two lower chambers of hea...more
TOF is having a combination of large VSD with severe obstruction of blood flow to the lungs that result in bluish-black discoloration of lips and fingers due to flow of oxygen-deficit blood to the body parts.
The four defects that commonly associated with Tetralogy of Fallot (TOF) are
Ventricular Septal Defect (VSD) a hole formed in ventricular septum that is situated between two lower chambers of hea...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Heart disease is definitely something, which is serious. In most cases, it is the result of a person s lack of prudence when it comes to staying fit and moderating what food items feature in the diet. But is this always the case? Well, not at all. Genetic or hereditary heart diseases, such as hypertrophic cardiomyopathy, long QT syndrome, very high cholesterol levels running in the family and many others, provide enough reason as to why not.
This is because a person cannot be blamed for...more
This is because a person cannot be blamed for...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Ever wondered why you needed to share your family s health history at a doctor s clinic? Specific questions regarding health issues of your immediate family or close blood relatives give your doctor an insight into various health risks you might have now or in future. Those are medical conditions inherited by parents or grandparents through genes. Genes are passed from parents to children in DNA of eggs or sperms. Even a single mutation (fault) in gene can influence body systems and may lead to ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
M.Ch - Cardio Thoracic Surgery, MBBS, MS...read more
Cardiothoracic Vascular Surgery•Pune
It is not just the skin or eye color that you inherit through your genes, it is also the chances of you having a heart attack. It has been proven beyond doubt that if heart diseases run in your family, then you are very likely to develop them too. Another worrying factor is that there are a whole lot of heart diseases which are hereditary, not just an isolated condition.
Whether it is congenital heart disease(which is present at birth) to atherosclerotic (which is usually associated wit...more
Whether it is congenital heart disease(which is present at birth) to atherosclerotic (which is usually associated wit...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Bachelor of Ayurveda, Medicine and Surge...read more
Ayurvedic Doctor•Lakhimpur Kheri
Cardiac problems are increasing in today s world, because of stress, poor lifestyle, increased obesity and lack of physical activity. A cardiologist expertise in the field of cardiology and can identify early warning signs of any cardiac problems which we may not be able to get hold of. They are specialized in performing simple checks like blood pressure, pulse rate and diagnostic tests such as an ECG, a blood test or an X-ray.
Consult these best cardiologist in Kolkata today to check y...more
Consult these best cardiologist in Kolkata today to check y...more
Book appointment with top doctors for Heart Disease By Birth treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously