Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Gestational Trophoblastic Neoplasia Tips
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Gestational trophoblastic disease is a rare condition. It only happens when trophoblast cells abnormally grow inside the uterus. Also, this only happens after conception. These cells surround the egg which has been fertilized in the uterus. It is also worth note that the trophoblast cells usually connect the fertilized eggs to the uterus' walls and also form a part of the placenta. It is only when there is a tumor that this disease is diagnosed. There are many forms of gestational trophoblastic ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Gestational trophoblastic disease is a rare condition. It only happens when trophoblast cells abnormally grow inside the uterus. Also, this only happens after conception. These cells surround the egg which has been fertilized in the uterus. It is also worth note that the trophoblast cells usually connect the fertilized eggs to the uterus' walls and also form a part of the placenta. It is only when there is a tumor that this disease is diagnosed. There are many forms of gestational trophobla...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Gestational trophoblastic disease is a rare condition. It only happens when trophoblast cells abnormally grow inside the uterus. Also, this only happens after conception. These cells surround the egg which has been fertilized in the uterus. It is also worth note that the trophoblast cells usually connect the fertilized eggs to the uterus' walls and also form a part of the placenta. It is only when there is a tumor that this disease is diagnosed. There are many forms of gestational trophoblastic ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Gestational trophoblastic disease is when there are trophoblastic cells which are growing abnormally inside the uterus. It is a pretty rare disease. Gestational trophoblastic disease mostly occurs after conception. The trophoblastic cells are a sort of tumorous cells which surround the fertilized egg in the uterus. It is a very serious and painful condition which can even become cancerous.
Here are the treatments for gestational trophoblastic disease.
Hysterectomy: A hysterecto...more
Here are the treatments for gestational trophoblastic disease.
Hysterectomy: A hysterecto...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Gynaecologist•Navi Mumbai
Gestational trophoblastic disease is a rare condition. It only happens when trophoblast cells abnormally grow inside the uterus. Also, this only happens after conception. These cells surround the egg which has been fertilized in the uterus. It is also worth note that the trophoblast cells usually connect the fertilized eggs to the uterus' walls and also form a part of the placenta. It is only when there is a tumor that this disease is diagnosed. There are many forms of gestational trophoblastic ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Gestational trophoblastic disease is a rare condition. It only happens when trophoblast cells abnormally grow inside the uterus. Also, this only happens after conception. These cells surround the egg which has been fertilized in the uterus. It is also worth note that the trophoblast cells usually connect the fertilized eggs to the uterus' walls and also form a part of the placenta. It is only when there is a tumor that this disease is diagnosed. There are many forms of gestational trophoblastic ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Gestational trophoblastic disease is a rare condition. It only happens when trophoblast cells abnormally grow inside the uterus. Also, this only happens after conception. These cells surround the egg which has been fertilized in the uterus. It is also worth note that the trophoblast cells usually connect the fertilized eggs to the uterus' walls and also form a part of the placenta. It is only when there is a tumor that this disease is diagnosed. There are many forms of gestational trophoblastic ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Gestational trophoblastic disease is a rare condition. It only happens when trophoblast cells abnormally grow inside the uterus. Also, this only happens after conception. These cells surround the egg which has been fertilized in the uterus. It is also worth note that the trophoblast cells usually connect the fertilized eggs to the uterus' walls and also form a part of the placenta. It is only when there is a tumor that this disease is diagnosed. There are many forms of the gestational trophoblas...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Gestational trophoblastic disease is a rare condition. It only happens when trophoblast cells abnormally grow inside the uterus. Also, this only happens after conception. These cells surround the egg which has been fertilized in the uterus. It is also worth note that the trophoblast cells usually connect the fertilized eggs to the uterus' walls and also form a part of the placenta. It is only when there is a tumor that this disease is diagnosed. There are many forms of the gestational trophoblas...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
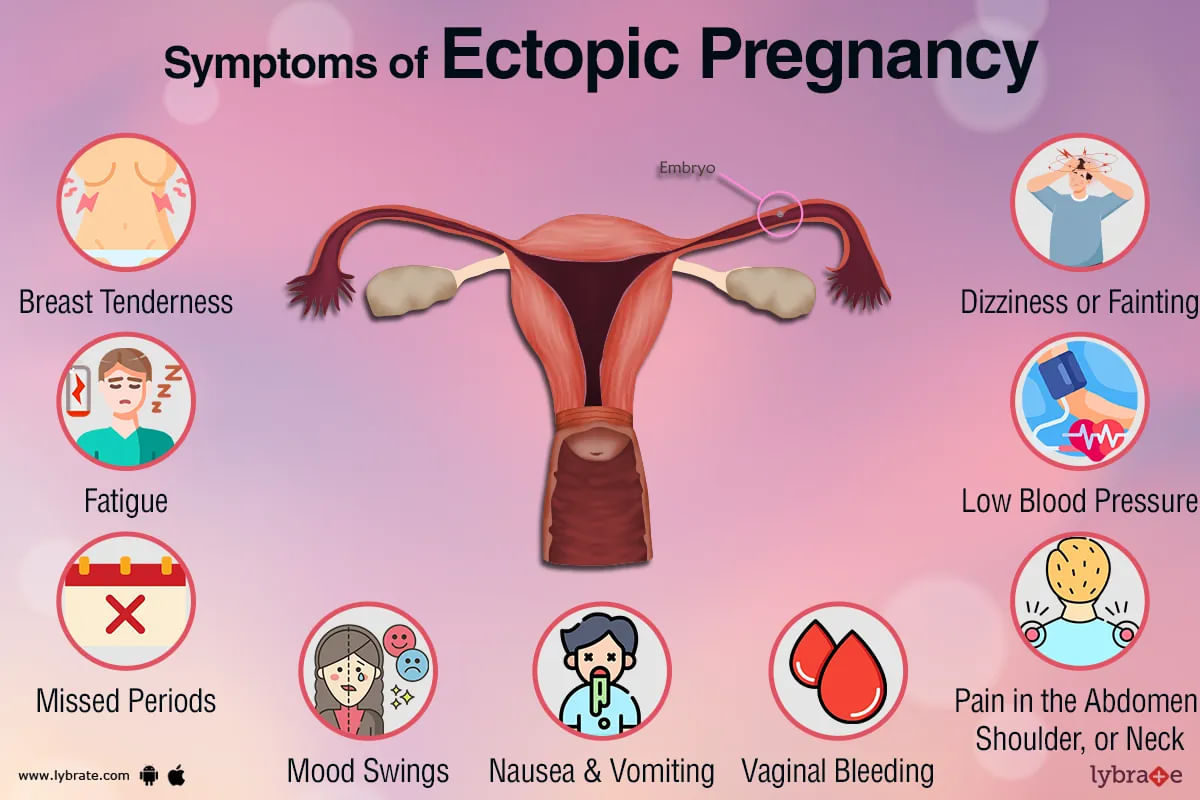
An ectopic pregnancy, often referred to as a tubal pregnancy, is when a fertilized egg implants outside of the uterus, usually in the fallopian tube. The pregnant person may be in a life-threatening situation as a result, and rapid medical care is necessary. The chance of an ectopic pregnancy can be decreased in a number of ways, while it cannot always be eliminated.
What is ectopic pregnancy?
;
In a typical pregnancy, the fertilized egg passes thr...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
MBBS Bachelor of Medicine and Bachelor o...read more
Gynaecologist•Muzaffarpur
क्या होता है एक्टोपिक प्रेग्नेंसी
गर्भावस्था यानी कि प्रेग्नेंसी का समय महिलाओं के जीवन में मुश्किलों से भरा लेकिन खूबसूरत अनुभव देने वाला होता है। इस दौरान महिलाओं को कई तरह की मुश्किलों का सामना भी करना पड़ता है। ऐसी ही एक समस्या है एक्टोपिक प्रेग्नेंसी। आज अपने इस लेख के माध्यम से हम आपको एक्टोपिक प्रेग्नेंसी के बारे में कुछ महत्वपूर्ण बातें बताएंगे। लेकिन इसके पहले आपको बताते हैं कि आखिर एक्टोपिक प्रेग्नेंसी क्या होता है।
जब गर्भ अपने स्थायी जगह यानी कि गर्भाशय को छोड़कर कहीं और स...more
गर्भावस्था यानी कि प्रेग्नेंसी का समय महिलाओं के जीवन में मुश्किलों से भरा लेकिन खूबसूरत अनुभव देने वाला होता है। इस दौरान महिलाओं को कई तरह की मुश्किलों का सामना भी करना पड़ता है। ऐसी ही एक समस्या है एक्टोपिक प्रेग्नेंसी। आज अपने इस लेख के माध्यम से हम आपको एक्टोपिक प्रेग्नेंसी के बारे में कुछ महत्वपूर्ण बातें बताएंगे। लेकिन इसके पहले आपको बताते हैं कि आखिर एक्टोपिक प्रेग्नेंसी क्या होता है।
जब गर्भ अपने स्थायी जगह यानी कि गर्भाशय को छोड़कर कहीं और स...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
वैसे तो प्रेग्नेंसी यानी कि गर्भावस्था के दौरान गर्भ में पल रहे शिशु के लिंग की जांच (ling ki jaanch) कराना असंवैधानिक है और ऐसा करने पर सजा का प्रावधान है, हालांकि समाज में कुछ ऐसी मिथ्याएं भी मौजूद हैं जो बिना भ्रूण के जांच के घर में ही गर्भवती महिला के कोख में पल रहे बच्चे के जेंडर का पता करने का दावा करती हैं। हम आपको अपने इस लेख के माध्यम से कुछ ऐसी ही मिथ्याओं की जानकारी देते हैं, लेकिन इसके पहले यह जानना बेहद जरूरी है कि आखिर प्रेग्नेंसी क्या है।
प्रेग्नेंसी क्या है
किसी भी म...more
प्रेग्नेंसी क्या है
किसी भी म...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
मासिक धर्म हर महिला के लिए आवश्यक होते हैं। नियमित रूप से सामान्य पीरियड्स होना ये दर्शाता है कि आपके स्वास्थ्य संबंधी समस्या नहीं है। पर अगर आपको दो मासिक धर्म के बीच रक्तस्राव होता है, पीरियड्स के दौरान बहुत अधिक ब्लीडिंग होती है या फिर आपके पीरियड्स सामान्य से ज्यादा दिनों तक चलते रहते हैं तो ये चिंता की बात हो सकती है। ऐसे में अगर दवाएं असर नहीं कर रही हैं तो आपको एंडोमिट्रियल एब्लेशन की ज़रूरत हो सकती है।इसकी मदद से रक्तस्राव को कम किया जा सकता है या फिर इसे पूरी तरह से रोका जा सकता है।
more
more
557 people found this helpful
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Gestational diabetes, as the name suggests, occurs during gestation or pregnancy when the blood sugar levels exceed the normal level. Gestational diabetes, like other form of diabetes, affects how your body cells use glucose or sugar during pregnancy, and usually disappears after you ve given birth.
Causes and symptoms to look out for!
During gestation, the placenta produces hormones that lead to the accumulation of blood glucose. Under normal condition, the pancreas forms enou...more
Causes and symptoms to look out for!
During gestation, the placenta produces hormones that lead to the accumulation of blood glucose. Under normal condition, the pancreas forms enou...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Gestational diabetes is diabetes that arises during the pregnancy and disappears after giving birth. It is usually diagnosed in the second stage by screening or blood test. It mostly occurs in the women who previously have some traits of diabetes. Gestational diabetes affects your pregnancy and your newborn baby health, but risk can be reduced if detected before and manage well.
Gestational diabetes is caused due to an excessive amount of blood sugar level, as at the time of pregnancy p...more
Gestational diabetes is caused due to an excessive amount of blood sugar level, as at the time of pregnancy p...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Gestational diabetes is a condition characterized by higher than normal blood sugar levels during pregnancy. The symptoms of this disorder are mild and a blood test has to be conducted as a part of the diagnosis. In all cases, the women should be administered treatment to avoid medical complications associated with it and to be on the safer side. Proper diagnosis is absolutely essential in the case of women with prediabetes or those women who had diabetes prior to pregnancy.
When the in...more
When the in...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Preeclampsia is a serious condition that can develop in pregnant women, especially after 20 weeks. Also called toxemia, it is characterized by high blood pressure, even in women who ve never had high BP.
Eclampsia is a rare but severe complication of preeclampsia which causes seizures and convulsions in pregnant women. It can even cause the death of the woman and/or her baby. This serious condition is prevalent in about 1 in every 200 women with preeclampsia.
Common symptoms of...more
Eclampsia is a rare but severe complication of preeclampsia which causes seizures and convulsions in pregnant women. It can even cause the death of the woman and/or her baby. This serious condition is prevalent in about 1 in every 200 women with preeclampsia.
Common symptoms of...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
In ordinary pregnancy, the egg released from the ovary becomes fertilized when it meets the sperm and travels through the fallopian tubes to the uterus where it grows in the following nine months. In an ectopic pregnancy, the fertilized egg never makes it to the uterus instead it stays in one of the fallopian tubes; this is also known as tubal pregnancy. In very rare cases, the egg also attaches itself to one of the two ovaries making your pregnancy difficult and putting your health in danger.more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Slight discomfort and pain is normally associated with every woman's monthly menstrual cycle. However, for some women, this discomfort can restrict their normal activities and put them in a lot of pain. This is often accompanied by heavy menstrual bleeding. Medication is usually the first line of treatment for heavy periods, but if this is not effective surgical options may need to be looked at. Amongst the surgical ways to deal with painful menstruation and heavy bleeding is a procedure known a...more
Book appointment with top doctors for Gestational Trophoblastic Neoplasia treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously