Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Foot Infection Tips
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
People with diabetes are at risk of foot problems due to high blood glucose levels. The two most common problems are peripheral vascular disease and diabetic neuropathy. Both conditions can lead to a number of serious complications. One such complication is diabetic foot infection an infection of the bones or soft tissues below the malleoli.
What causes diabetic foot infections?
Over time, excess blood glucose levels can damage blood vessels, skin, and the nerves in your feet...more
What causes diabetic foot infections?
Over time, excess blood glucose levels can damage blood vessels, skin, and the nerves in your feet...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
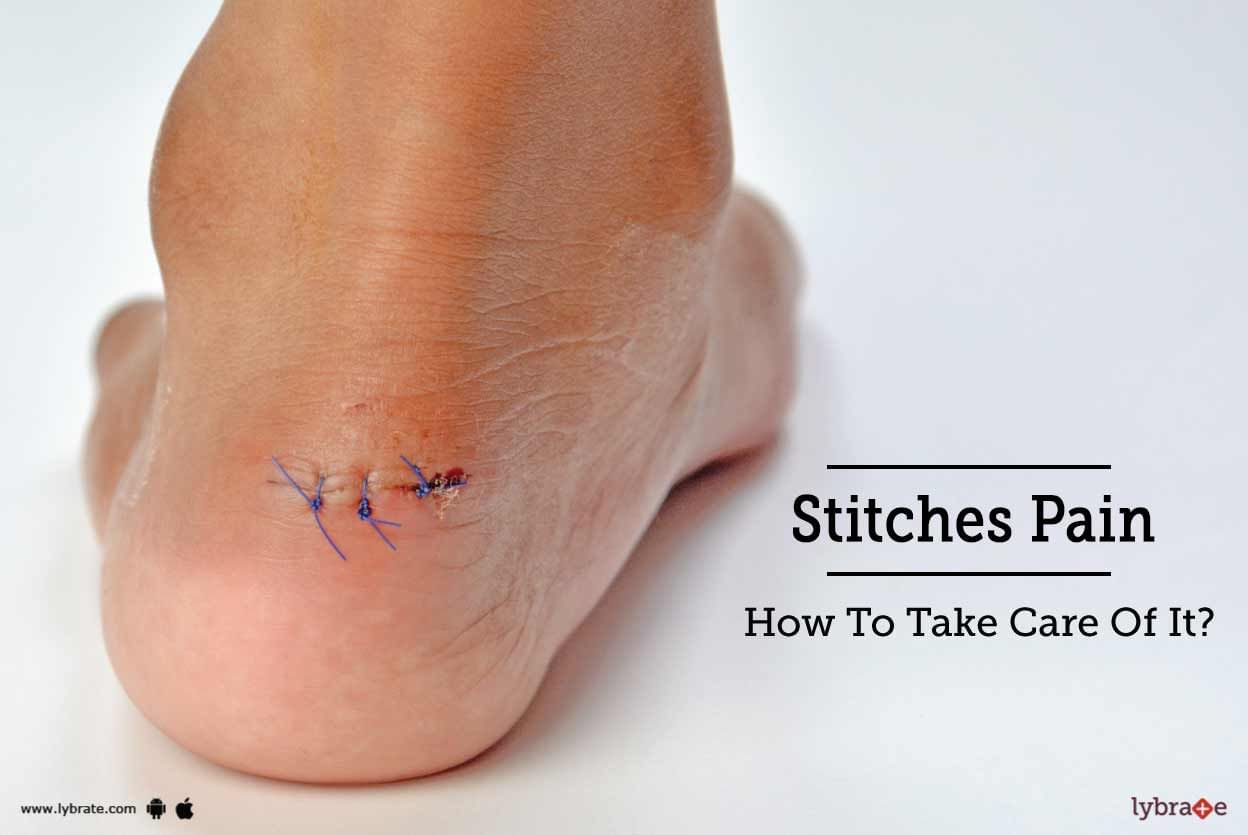
Stitches or sutures act as a closure for either surface wounds or deep wounds. Procedure to close a deep wound comprises of sewing the two edges and applying stitches under the skin surface.
Categories of sutures
Non-absorbable stitches are applied in case of skin wounds or internal wounds. Such stitches heal quickly and are easy to remove. Non-absorbable stitches are made of natural fibres or synthetic threads like nylon polypropylene. As the name suggests, these stitches are ...more
Categories of sutures
Non-absorbable stitches are applied in case of skin wounds or internal wounds. Such stitches heal quickly and are easy to remove. Non-absorbable stitches are made of natural fibres or synthetic threads like nylon polypropylene. As the name suggests, these stitches are ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Charcot foot is a rare complication of diabetes. It usually affects diabetics with peripheral neuropathy. Charcot affects the joints, bones and soft tissues of the ankle or foot. This causes the bones to become brittle and fragile, and the joints to become dislocated. Over time, the foot joints collapse and become deformed.
What causes Charcot foot?
The following conditions/factors may cause Charcot foot to develop in individuals
Spinal cord injury/disease
A...more
What causes Charcot foot?
The following conditions/factors may cause Charcot foot to develop in individuals
Spinal cord injury/disease
A...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
About 7% of the population of the world is suffering from some form of diabetes and the number is set to rise by a significant margin by 2030. However, what is really disturbing about this figure is that people suffering from diabetes are at a very high risk of necrosis and infection in their feet. This infection can lead to amputation of the foot. The International Diabetes Federation has observed that people suffering from diabetes are 25 times susceptible to the feet problems like infection a...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
When you are suffering from Diabetes, you need to take extra care of your feet and eyes. Both these parts of the body are heavily affected during this disease. In fact, your diet should also be taken in such a way that it maintains good eye sight and proper foot care. Apart from drinking lots of water and controlling your diet, you need to take special care of your eyes and feet. Here are a few tips that might help you to take good care of these two parts of your body.
Foot Care:
more
Foot Care:
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
There are many problems that come along with Diabetes. Such problems are associated with the foot. These foot problems may be infectious which makes it difficult for a person to walk.
Let s know some of the common foot problems associated with Diabetes.
Diabetic Neuropathy -
When the diabetes is not being managed successfully by medication it can affect the nerves. Damaged nerves in the feet or legs result in diabetic neuropathy. When there is no sensation of pain, he...more
Let s know some of the common foot problems associated with Diabetes.
Diabetic Neuropathy -
When the diabetes is not being managed successfully by medication it can affect the nerves. Damaged nerves in the feet or legs result in diabetic neuropathy. When there is no sensation of pain, he...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
You get diabetes when your body does not produce sufficient amount of insulin or because your body becomes immune to it. Diabetes is a killer disease because it makes the individual vulnerable to a host of ailments. One of its most damaging complications is the diabetic foot.
What is diabetic foot?
This ailment develops when blood sugar level remains high for a prolonged period of time, ulcers grow either because of either neuropathy (nerve damage) or peripheral arterial diseas...more
What is diabetic foot?
This ailment develops when blood sugar level remains high for a prolonged period of time, ulcers grow either because of either neuropathy (nerve damage) or peripheral arterial diseas...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Surgery is an art and surgeons are artists. It is a gruelling process and requires extreme dexterity and quite a bit of courage. It is a process where specialized tools are used to remove unwanted tissues, infections or treat an injury or to reshape the human body.
A surgeon is a person who executes the process of surgery. A surgery team is made for these operations which is highly delicate and life-risking task. Surgeon s have their own assistants who assists or helps with the surgical...more
A surgeon is a person who executes the process of surgery. A surgery team is made for these operations which is highly delicate and life-risking task. Surgeon s have their own assistants who assists or helps with the surgical...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Diabetes is a deadly disease that is triggered when the body cannot produce enough insulin or becomes resistant to insulin. Diabetes makes an individual prone to a host of ailments, one of which is a diabetic foot.
What is diabetic foot?
When blood sugar remains high for protracted periods, it affects the feet in a number of ways and leads to a condition called a diabetic foot. There are two types of diabetic foot-
Diabetic neuropathy: Diabetes dulls or even damages ...more
What is diabetic foot?
When blood sugar remains high for protracted periods, it affects the feet in a number of ways and leads to a condition called a diabetic foot. There are two types of diabetic foot-
Diabetic neuropathy: Diabetes dulls or even damages ...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
Why do feet stink?
Smelly feet can be a cause of great embarrassment and discomfort for anyone. Also known as bromodosis, the primary cause of smelly feet is the sweat glands in your feet. This part of the human body has more sweat glands than anywhere else in the body. Additionally, compared to sweat glands in the other parts of the body that secrete to control your body temperature when exposed to hot weather or while exercising, the sweat glands in your feet produce perspiration all ...more
Smelly feet can be a cause of great embarrassment and discomfort for anyone. Also known as bromodosis, the primary cause of smelly feet is the sweat glands in your feet. This part of the human body has more sweat glands than anywhere else in the body. Additionally, compared to sweat glands in the other parts of the body that secrete to control your body temperature when exposed to hot weather or while exercising, the sweat glands in your feet produce perspiration all ...more
Book appointment with top doctors for Foot Infection treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously