Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTips
Empyema Thoracis Tips
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
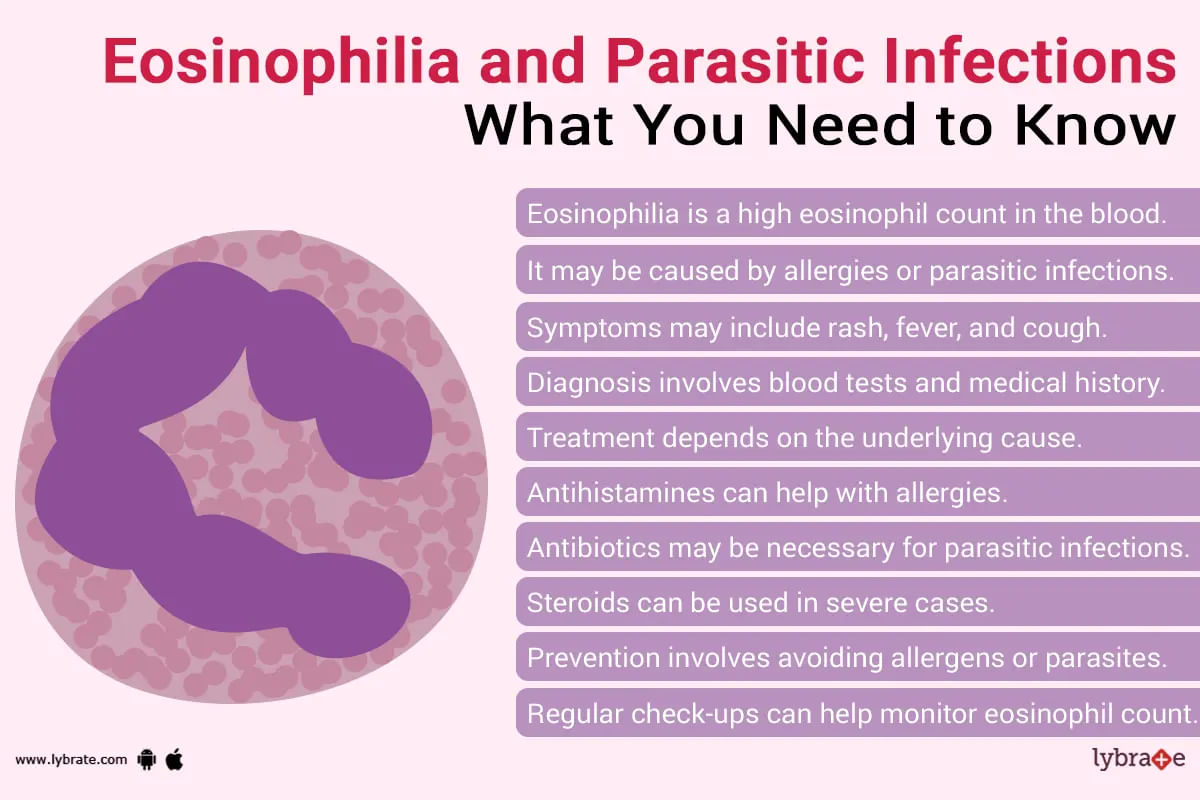
Eosinophilia is when the level of eosinophils is higher than normal level in blood. Eosinophils are a type of WBC (white blood cells). These cells are the immune system of our body which helps to fight diseases. When there is parasitic infection, bacterial infection or any type of allergic reaction, these cells help us to fight it. It is also useful in defeating cancer.
If there is an attack of foreign substance/lives there is an increase at levels of eosinophils in blood or if attack i...more
If there is an attack of foreign substance/lives there is an increase at levels of eosinophils in blood or if attack i...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
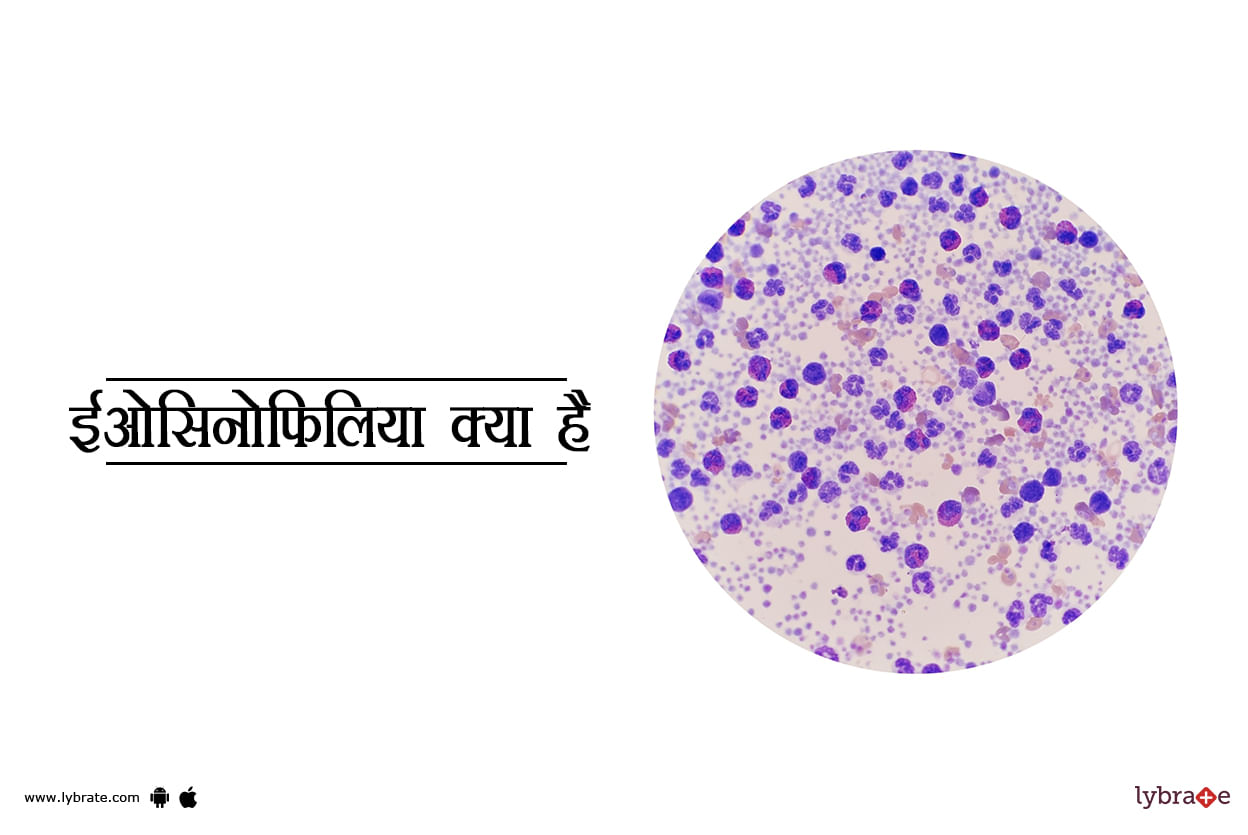
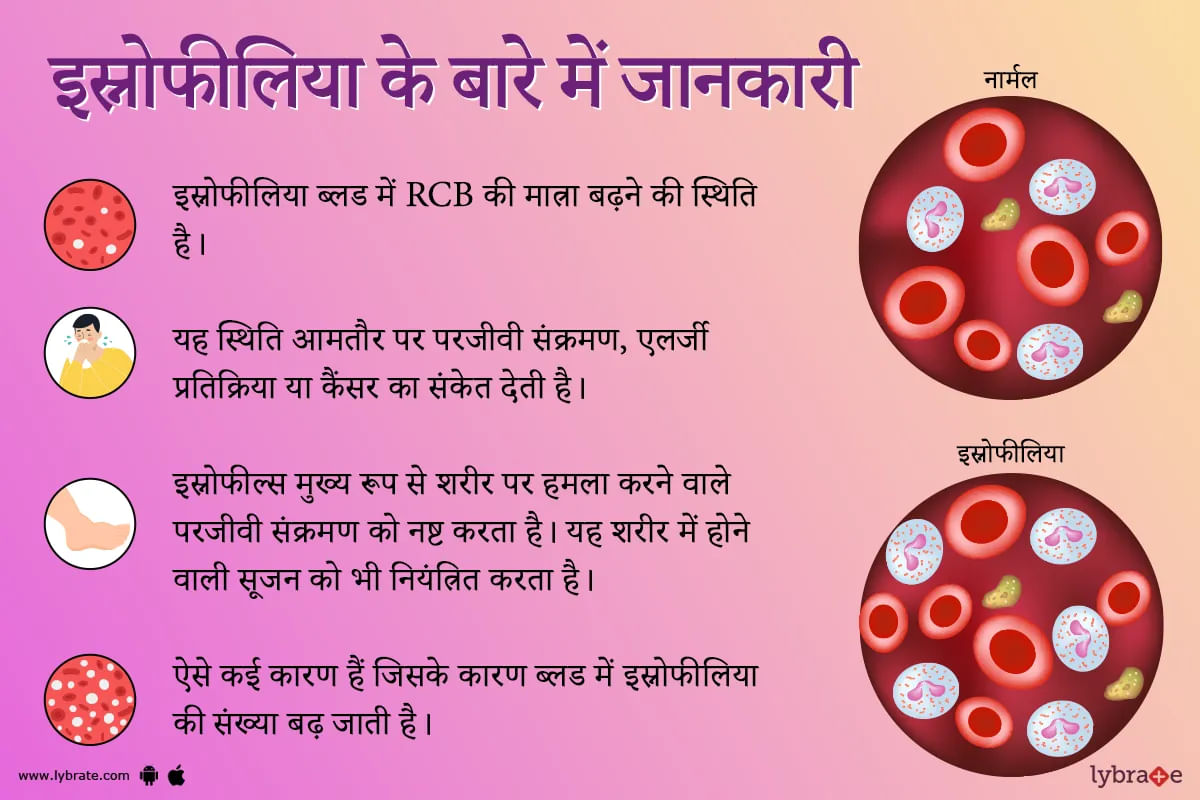
ईओसिनोफिलिया तब होता है जब आपका शरीर असामान्य रूप से ईओसिनोफिल पैदा करता है। ईओसिनोफिल कई श्वेत रक्त कोशिकाओं में से एक हैं जो आपकी प्रतिरक्षा प्रणाली का सहयोग करती हैं।
कभी-कभी, कुछ चिकित्सीय स्थितियां और दवाएं ईओसिनोफिल के उच्च स्तर का कारण बनती हैं।
ईओसिनोफिलिया क्या है?
ईओसिनोफिल श्वेत रक्त कोशिकाओं में से एक हैं जो आपकी प्रतिरक्षा प्रणाली को सपोर्ट करती हैं। वे एलर्जी के खिलाफ आपके शरीर की रक्षा प्रणाली का हिस्सा हैं और आपके शरीर को फंगल और परजीवी संक्रमण से बचाने में ...more
कभी-कभी, कुछ चिकित्सीय स्थितियां और दवाएं ईओसिनोफिल के उच्च स्तर का कारण बनती हैं।
ईओसिनोफिलिया क्या है?
ईओसिनोफिल श्वेत रक्त कोशिकाओं में से एक हैं जो आपकी प्रतिरक्षा प्रणाली को सपोर्ट करती हैं। वे एलर्जी के खिलाफ आपके शरीर की रक्षा प्रणाली का हिस्सा हैं और आपके शरीर को फंगल और परजीवी संक्रमण से बचाने में ...more
79 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
1. Dr. Kavitha v. Reddy ;
Https://www. Lybrate. Com/bangalore/doctor/dr-kavitha-v-reddy-general-physician
Dgo, mbbs
21 years experience 450 at clinic ;
She is a highly recognized general physician who has successfully helped several people with intricate issues. Headaches can range from mild to severe in intensity and frequency from person to person, for which the physician has a lot of experience dealing with a countless n...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
1. Dr. Rashid akhtar
Https://www. Lybrate. Com/noida/doctor/dr-rashid-akhtar-homeopath
Md - homeopathy, bhms
21 years experience 500 at clinic 300 online
He is a well regarded physician who has successfully helped a variety of people deal with intricate problems. His areas of specialty include blood diseases, disorders of the ear, nose, and throat; diabetes; high blood pressure; skin illnesses; psychological problems; and a great deal more. He...more
123 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
इओसिनोफिलिया एक ऐसी स्थिति है जब आपके रक्त में इओसिनोफिल के सामान्य स्तर से अधिक पाया जाता है। इओसिनोफिल्स एक प्रकार की बीमारी से लड़ने वाली श्वेत रक्त कोशिका हैं। इसे कई बार सामान्य भाषा में स्नोफीलिया कहा जाता है। यह स्थिति अक्सर परजीवी संक्रमण, एलर्जी प्रतिक्रिया या कैंसर का संकेत देती है।
आपके रक्त में उच्च स्तर के इओसिनोफिल्स कई जगहों पर पाए जा सकते हैं खून में (रक्त इओसिनोफिलिया) या संक्रमण या सूजन (ऊतक इओसिनोफिलिया) के स्थान पर ऊतकों में भी हो सकते हैं।
ऊतक इओसिनोफिलिया ...more
आपके रक्त में उच्च स्तर के इओसिनोफिल्स कई जगहों पर पाए जा सकते हैं खून में (रक्त इओसिनोफिलिया) या संक्रमण या सूजन (ऊतक इओसिनोफिलिया) के स्थान पर ऊतकों में भी हो सकते हैं।
ऊतक इओसिनोफिलिया ...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
1. Dr. Sanket gupta
Https://www. Lybrate. Com/delhi/doctor/dr-sanket-gupta-homeopath
Bhms, md-homeopathy, pgpc - preventive cardiology
13 years experience 500 at clinic 250 online
He is an adept practitioner who works at health care facilities as a pain management and obesity specialist, where he treats patients who suffer from a variety of ailments brought on by their lifestyle choices. He also addresses cardiovascular problems. ;
As a dermato...more
Https://www. Lybrate. Com/delhi/doctor/dr-sanket-gupta-homeopath
Bhms, md-homeopathy, pgpc - preventive cardiology
13 years experience 500 at clinic 250 online
He is an adept practitioner who works at health care facilities as a pain management and obesity specialist, where he treats patients who suffer from a variety of ailments brought on by their lifestyle choices. He also addresses cardiovascular problems. ;
As a dermato...more
9 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
1. Dr. Chaithanya k s
Https://www. Lybrate. Com/bangalore/doctor/dr-chaithanya-ks-ayurveda-1
Bachelor of ayurveda, medicine and surgery (bams), ms
19 years experience 500 at clinic 500 online
;
Being recognised as a reputed physician especially as an ayurvedic doctor.
He is a well known physician who specialises in ayurveda. He got his bachelor of ayurveda medicine and surgery (bams) from kvgamc in 2003 and Ms. From kv university in 2...more
Https://www. Lybrate. Com/bangalore/doctor/dr-chaithanya-ks-ayurveda-1
Bachelor of ayurveda, medicine and surgery (bams), ms
19 years experience 500 at clinic 500 online
;
Being recognised as a reputed physician especially as an ayurvedic doctor.
He is a well known physician who specialises in ayurveda. He got his bachelor of ayurveda medicine and surgery (bams) from kvgamc in 2003 and Ms. From kv university in 2...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Ayurveda is a holistic system of medicine that focuses on improving your overall well-being, rather than just focusing on the symptoms of the disease. Being a complete natural based method, it has no side effects. Ayurvedic remedies for kidney stones emphasize on improving your lifestyle and diet to keep the energy balance in your body.
The causes of kidney stones range from factors such as an imbalanced diet, sedentary lifestyle and spicy food. Less water consumption is also a major ca...more
The causes of kidney stones range from factors such as an imbalanced diet, sedentary lifestyle and spicy food. Less water consumption is also a major ca...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
According to Ayurveda, Panchakarma therapy aims at detoxifying the human body. Pancha means five and karma means treatment. This comprises of 5 methods that are used to address the troublesome doshas in the body. The excess doshas would be expelled and the ama (toxins produced in the body) would be eliminated from the system through the body's own organs elimination channels (urinary tract, colon, sweat organs, digestive tract and the lungs).
The features of Panchakarma inclu...more
The features of Panchakarma inclu...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Ayurveda is an ancient Indian field of medicine that has been in existence since time immemorial. Many people swear by its efficacy and it is also a proper field of study for people who want to practice this form of medicine as doctors. Ayurveda makes use of a variety of herbs and lifestyle changes including diet, rest and massages in order to create a healthier body. Ayurveda combines Yogic postures with these herbs to create various kinds of treatment for varied conditions.
Panchakarm...more
Panchakarm...more
Book appointment with top doctors for Empyema Thoracis treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously