Get the App
For Doctors
Login/Sign-up
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Ectodermal Dysplasia-syndactyly Syndrome Tips
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
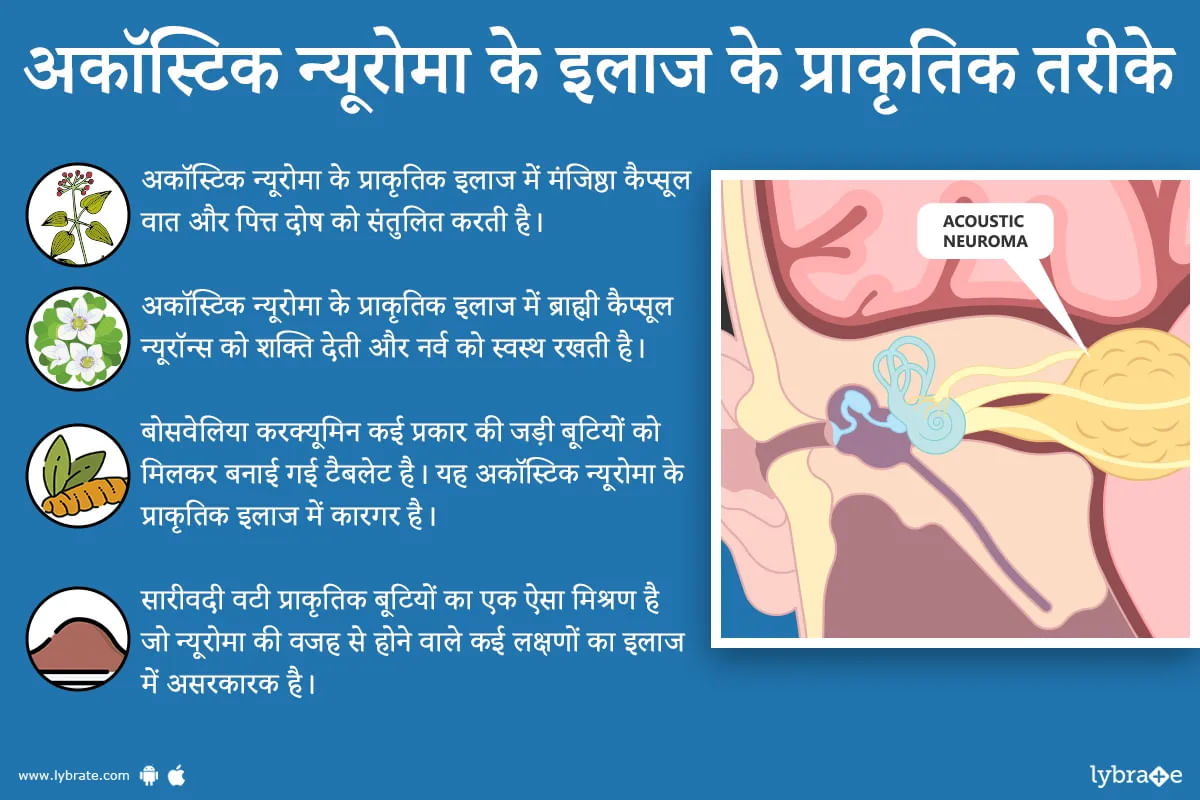
अकॉस्टिक न्यूरोमा या वेस्टिबुलर श्वानोमा एक बेनाइंग ट्यूमर है जो जो आपके आंतरिक कान को मस्तिष्क से जोड़ने वाली तंत्रिका पर विकसित होता है। यह आमतौर पर एक धीमी गति से बढ़ने वाला ट्यूमर है, हालांकि गैर-आक्रामक, और कैंसर वाला ट्यूमर पर है पर यह यदि यह नियंत्रण से बाहर हो जाए तो मस्तिष्क में विभिन्न संरचनाओं पर दबाव डाल सकता है। इससे सबसे अधिक सामान्य रूप से सुनना, शरीर का संतुलन और चेहरे के भाव प्रभावित होते हैं।
यह ट्यूमर बहुत ज्यादा सामान्य नहीं माना जाता है और यह बहुत कम लोगों को हो...more
यह ट्यूमर बहुत ज्यादा सामान्य नहीं माना जाता है और यह बहुत कम लोगों को हो...more
1156 people found this helpful
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
1. Dr. Madu sridhar
Https://www. Lybrate. Com/chennai/doctor/dr-madu-sridhar-orthopedist
Ms in orthopaedics, m. Ch trauma & ortho, diploma in orthopaedics (d. Ortho),
14 years experience 250 at clinic 300 online
He is regarded as a senior clinician with expertise as an orthopaedic doctor. He is a kind hearted experienced physician with extensive experience as an orthopaedic surgeon, paediatric orthopedist, joint replacement surgeon, as wel...more
Https://www. Lybrate. Com/chennai/doctor/dr-madu-sridhar-orthopedist
Ms in orthopaedics, m. Ch trauma & ortho, diploma in orthopaedics (d. Ortho),
14 years experience 250 at clinic 300 online
He is regarded as a senior clinician with expertise as an orthopaedic doctor. He is a kind hearted experienced physician with extensive experience as an orthopaedic surgeon, paediatric orthopedist, joint replacement surgeon, as wel...more
29 people found this helpful
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
Dr. Girish Gadre
MBBS, DM - Neurology
21 Years Experience 500 - 600 at clinic
As a neurologist and a general physician who specialises in medicine, he has made a name for himself via the work that he has done. He obtained his MBBS from Maulana Azad Medical College in 2001, and he received his DM in Neurology from NIMHANS Bangalore in 2007. Both degrees are in the field of medicine.
Neurosurgeon Dr. Girish Gadre has been practicing in the Malleswaram neighborhood of Bang...more
MBBS, DM - Neurology
21 Years Experience 500 - 600 at clinic
As a neurologist and a general physician who specialises in medicine, he has made a name for himself via the work that he has done. He obtained his MBBS from Maulana Azad Medical College in 2001, and he received his DM in Neurology from NIMHANS Bangalore in 2007. Both degrees are in the field of medicine.
Neurosurgeon Dr. Girish Gadre has been practicing in the Malleswaram neighborhood of Bang...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
If you are suffering from neuromuscular disorders and require an effective, natural cure, you should opt for Ayurveda. Neuromuscular disorders are conditions in which certain areas of your central nervous system may get affected. It leads to the dysfunction and degeneration of your musculature, and also disables the functioning of certain organs at times. According to the Ayurvedic principles, most neuromuscular disorders occur because of beeja dosha, deranged vata and due to certain defects or ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The heart is a vital organ that pumps blood throughout the body, thereby supplying the body with the essential nutrients and oxygen while removing the harmful toxins and wastes. Certain conditions may interfere with the ability of the heart to pump blood (there could be clogging in one of the artery or arteries). Devoid of blood and the essential nutrients, the other vital organs soon start to falter. In fact, reduced supply of oxygen and blood to the brain can prove to be fatal, triggering loss...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Definition: Osteoarthritis is the degenerative joint disease, involving weight-bearing joints. It usually occurs after 40 years of age. Articular cartilage, which provides a remarkably smooth surface during movement is gradually evaded.
Causes:
Obesity
excess or improper use of joint
poor nutrition
improper posture
use of unwholesome footwear
Feature :
Pain ( usually increased by activity and relieved by rest)
swelling (by increased bony pr...more
Causes:
Obesity
excess or improper use of joint
poor nutrition
improper posture
use of unwholesome footwear
Feature :
Pain ( usually increased by activity and relieved by rest)
swelling (by increased bony pr...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The pituitary gland is a small, pea-sized attached to the base of the brain. It controls growth, functioning and development of other hormonal glands. Deficit of one or more pituitary hormones is a state of Hypopituitarism. This clinical term is used by endocrinologists to mean that one or more pituitary glands are deficient. In hypopituitarism, the pituitary gland does not produce the normal amounts of hormones.
Causes-
Hypopituitarism has the following causes
Brain ...more
Causes-
Hypopituitarism has the following causes
Brain ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The hip is a ball-and-socket joint in the human body. Normally, the ball located at the upper part of the thighbone (femur) firmly fits into the socket, which is a part of the pelvis bone. In people, especially children and babies, who have Developmental Dysplasia of Hips (DDH), the ball does not fit the socket perfectly. Therefore, the hip joint is not formed completely and is likely to dislocate easily.
DDH is a congenital disorder, meaning the condition is present at birth. However, ...more
DDH is a congenital disorder, meaning the condition is present at birth. However, ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The medical term spina bifida or spinal bifida refers to a congenital defect in the spine. In simpler terms, spina bifida is a defect in the neural tube. Based on the severity of this disease, spina bifida can be divided into three different types:
Myelomeningocele
Meningocele
Occulta
The symptoms of spina bifida vary depending on each of these three types. Let's take a closer look at its symptoms here:
Myelomeningocele
Myelomeningocele is the most severe...more
Myelomeningocele
Meningocele
Occulta
The symptoms of spina bifida vary depending on each of these three types. Let's take a closer look at its symptoms here:
Myelomeningocele
Myelomeningocele is the most severe...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
What Is Kyphosis Disease?
Kyphosis is an exaggerated, forward rounding of the back. It can occur at any age but is most common in older women.
Age-related kyphosis is often due to weakness in the spinal bones that causes them to compress or crack. Other types of kyphosis can appear in infants or teens due to malformation of the spine or wedging of the spinal bones over time.
Mild kyphosis causes few problems. Severe kyphosis can cause pain and be disfiguring. Treatment for kyphosis d...more
Kyphosis is an exaggerated, forward rounding of the back. It can occur at any age but is most common in older women.
Age-related kyphosis is often due to weakness in the spinal bones that causes them to compress or crack. Other types of kyphosis can appear in infants or teens due to malformation of the spine or wedging of the spinal bones over time.
Mild kyphosis causes few problems. Severe kyphosis can cause pain and be disfiguring. Treatment for kyphosis d...more
Book appointment with top doctors for Ectodermal Dysplasia-syndactyly Syndrome treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously