Get the App
For Doctors
Login/Sign-up
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Dementia In Parkinson's Disease Tips
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Ageing is inevitable, and as much as we want to escape, there is no way out. All organs, whether obvious or not, undergo gradual degeneration and deterioration. The brain is no exception, and memory being one of its main function also begins to decline with age. There are various factors which determine how quickly this ageing sets in and how rapidly it progresses. These are dictated by a person s lifestyle, activity levels, and overall body changes. Dementia also has a strong family history, an...more
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
Chronic respiratory diseases like bronchial asthma, bronchiectasis, copd, sarcoidosis and interstitial lung disease are vulnerable to repeated infections and multiple hospital visits or admission.
The main reasons for the increased susceptibility is altered lung defence, use of steroids in various respiratory conditions and multiple comorbidities like diabetes and coronary disease.
Patients should ideally be vaccinated for pneumococcal and influenza disease routinely.
The main reasons for the increased susceptibility is altered lung defence, use of steroids in various respiratory conditions and multiple comorbidities like diabetes and coronary disease.
Patients should ideally be vaccinated for pneumococcal and influenza disease routinely.
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
We occasionally take our lungs for granted. They keep us healthy and well, and we don't have to ponder about them much. This is why it is critical and advised to prioritize your lung health.
Our body has a built-in defensive mechanism intended to keep dirt and bacteria out of your lungs. However, there are several critical steps you may take to reduce your chance of lung illness. Scroll down and look at some useful tips to take care of your lungs in a better and healthier way...more
Our body has a built-in defensive mechanism intended to keep dirt and bacteria out of your lungs. However, there are several critical steps you may take to reduce your chance of lung illness. Scroll down and look at some useful tips to take care of your lungs in a better and healthier way...more
1317 people found this helpful
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Brain tumor refers to the development of unusual cells in the brain or around the nearby tissues and structures. Pediatric Brain Tumor means the development of these unusual cells in the brain of children. There are two types of brain tumors: Benign or non-cancerous and malignant or Cancerous. Tumors like ependymoma and medulloblastoma are quite common among children. The treatment of the tumor is determined by its severity, type, location, age, and overall health of the child. The treatment of ...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
The pituitary gland is located in the brain, behind the bridge of your nose. It is a very important gland that regulates the activities of the other endocrinal glands. Benign tumours can sometimes develop in the pituitary gland.
Adenomas result in a disruption in the secretion of pituitary hormones. And this can have a severe fallout on the body.
What are Non-Functional Pituitary Tumours?
30% of all pituitary tumours are non-functional tumours. These tumours do not allow the pit...more
Adenomas result in a disruption in the secretion of pituitary hormones. And this can have a severe fallout on the body.
What are Non-Functional Pituitary Tumours?
30% of all pituitary tumours are non-functional tumours. These tumours do not allow the pit...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Interstitial lung disease is an umbrella term that includes a number of conditions that causes scarring of the tissues of the lungs. This scarring can hamper your breathing and therefore cause less oxygen to be present in your blood.
When you are exposed to hazardous materials like asbestos for long periods, you can get interstitial lung disease. Even autoimmune conditions like rheumatoid arthritis can result in this condition.
Once the tissues of your lungs are scarred, chanc...more
When you are exposed to hazardous materials like asbestos for long periods, you can get interstitial lung disease. Even autoimmune conditions like rheumatoid arthritis can result in this condition.
Once the tissues of your lungs are scarred, chanc...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Peripheral Artery Disease (PAD) is a disease of blood vessels that are located outside the heart and brain. The condition develops due to fatty deposits in the arteries and veins that stops the blood flow to the heart and mind as the case may be. It narrows the artery and restricts the blood flow, which causes problems to other organs of the body such as kidney, liver, and stomach.
Symptoms of Peripheral Artery Disease-
Peripheral Artery Disease is the most common type of condi...more
Symptoms of Peripheral Artery Disease-
Peripheral Artery Disease is the most common type of condi...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
A tumor may be defined as an abnormal unwanted growth of tissue in any part of the body. This word need not immediately cause panic because the tumor may or may not cause a health threat. There are three types of tumors:
Benign tumor: This is a noncancerous type of tumor. In our body, new cells are formed while the old ones called dead ones are disposed by our immune system. When this disposal of cells does not occur, the remaining dead cells form a lump, which is called a benign tumor....more
Benign tumor: This is a noncancerous type of tumor. In our body, new cells are formed while the old ones called dead ones are disposed by our immune system. When this disposal of cells does not occur, the remaining dead cells form a lump, which is called a benign tumor....more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
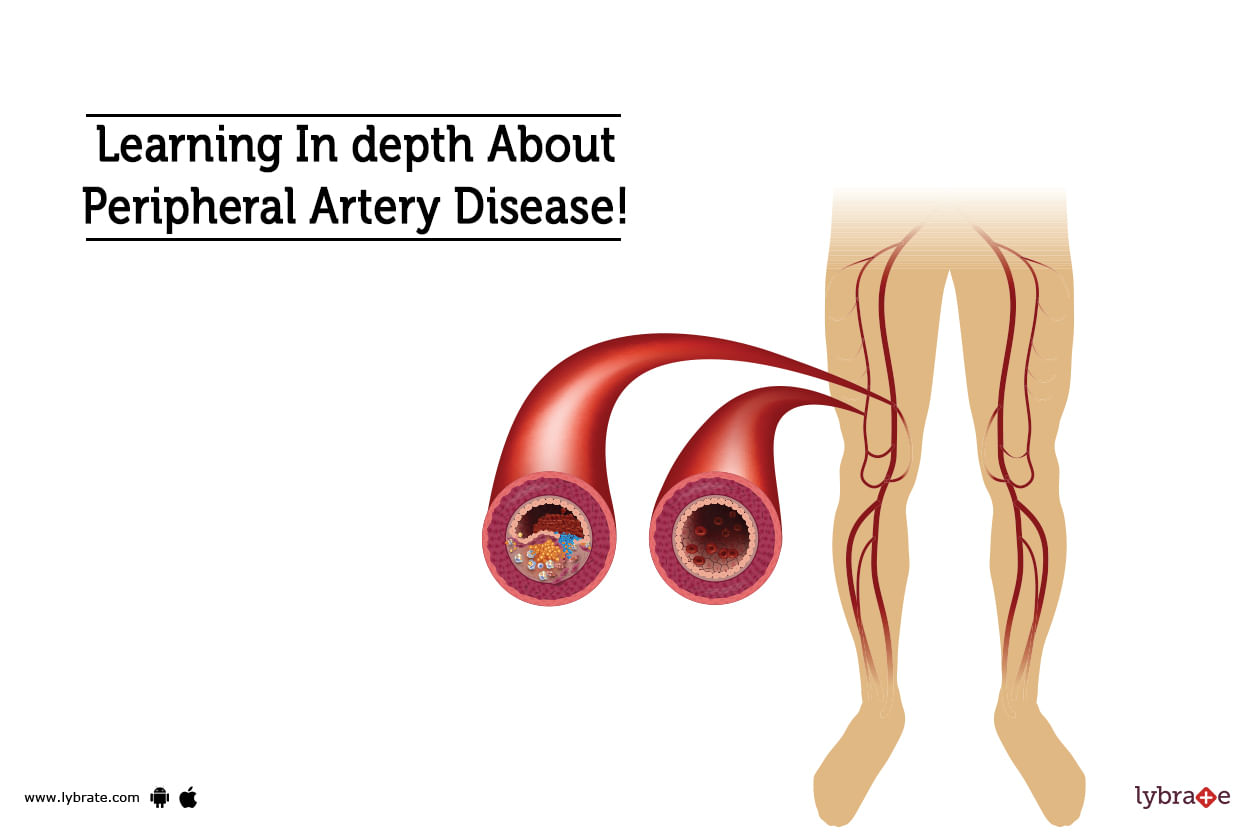
MBBS Bachelor of Medicine and Bachelor o...read more
Pulmonologist•Faridabad
Pulmonary Function Tests or PFTs are a set of tests that are used to determine, measure or observe the functioning of the lungs. The most common pulmonary function tests used are spirometry, gas diffusion, and lung plethysmography.
Highlights of pulmonary function tests
A spirometry test is used to measure the amount of air inhaled and exhaled. It also measures the amount of time taken to complete a respiration cycle.
Lung plethysmography measures the amount of air in the l...more
Highlights of pulmonary function tests
A spirometry test is used to measure the amount of air inhaled and exhaled. It also measures the amount of time taken to complete a respiration cycle.
Lung plethysmography measures the amount of air in the l...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
A brain tumor can occur at any age and it generally occurs in people in the age group of 40-60 years. The common types of brain tumor are termed as meningioma and gliomas. These supratentorial brain tumors generally occur above the covering of the cerebellum tissue. In children, brain tumors occur at the age of 1-12 years and the most common tumors are ependymomas, astrocytoma and meduloblastomas. Brain tumor is the common cause of death even in children.
Tips for Detecting a Brain Tumo...more
Tips for Detecting a Brain Tumo...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
If you are experiencing difficulty in breathing or rapid breathing, shortness of breath and low blood pressure, you might have been affected with acute respiratory distress syndrome or ARDS. This is a fatal lung condition in which the supply of oxygen to the lungs and into the blood gets prevented. The symptoms of this syndrome develop within two days of the illness.
Here are 10 important facts about ARDS you should know about:
Because of the low level of oxygen in the blood, ...more
Here are 10 important facts about ARDS you should know about:
Because of the low level of oxygen in the blood, ...more
Book appointment with top doctors for Dementia In Parkinson's Disease treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously