Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Bypass Surgery Tips
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
General Surgeon•
1. Dr. Muthuraju k r
Https://www. Lybrate. Com/bangalore/doctor/dr-muthuraju-k-r-general-surgeon
;
Mbbs, ms, gastro-intestinal, bariatric and metabolic surgery
21 years experience 0 at clinic
As an experienced and skilled surgeon, he has assisted a great number of patients and is currently working with vulnerable patients who have suffered from myocardial infarction, systemic hypertension, and illnesses such as arteriosclerosis and oth...more
Https://www. Lybrate. Com/bangalore/doctor/dr-muthuraju-k-r-general-surgeon
;
Mbbs, ms, gastro-intestinal, bariatric and metabolic surgery
21 years experience 0 at clinic
As an experienced and skilled surgeon, he has assisted a great number of patients and is currently working with vulnerable patients who have suffered from myocardial infarction, systemic hypertension, and illnesses such as arteriosclerosis and oth...more
12 people found this helpful
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Multi Speciality•Gorakhpur
Weight loss surgery or bariatric surgery is an effective treatment procedure for people, who are morbidly obese, i.e. a person weighing 100 pounds over his/her ideal body weight or having BMI (body mass index) higher than 40. One of the major reasons for the increasing trend of obesity is overconsumption of unhealthy food. This combined with lack of physical activity and a sedentary lifestyle leads to the accumulation of excess calories in the body.
Who Needs Bariatric Surgery?
more
Who Needs Bariatric Surgery?
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Obesity surgery is more commonly referred to as bariatric surgery. It is a surgery done on the stomach and/or intestines of a person with morbid obesity so that he or she loses weight. It is believed that as of now, bariatric surgery is the only option that almost always works to help overly obese people lose a lot of weight, which automatically makes the associated chronic conditions vanish.
How does this surgery work? Bariatric surgery works by changing the anatomy of the stomach and ...more
How does this surgery work? Bariatric surgery works by changing the anatomy of the stomach and ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The word acute coronary syndrome refers to a group of symptoms that are caused by blockage of the blood flow to the heart muscles. The most common result of this is myocardial infarction or heart attack as it is popularly called. Reduced blood flow leads to death of some portion of the heart muscle wall. While the word heart attack sounds almost fatal, it need not be the case. Knowing how to identify an attack and being aware of some simple measures can help save lives.
Symptoms: The...more
Symptoms: The...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Coronary artery disease is one of the major killer diseases of modern society. It is not a solitary problem but brings with it a multitude of issues including obesity, diabetes, stroke, and other metabolic disorders. A thorough understanding of what causes it and how to manage it can help save thousands of lives.
Causes: The circulatory system is mainly made up of the heart and a complex network of arteries and veins. The inner walls of these are lined with smooth muscles, allowing for ...more
Causes: The circulatory system is mainly made up of the heart and a complex network of arteries and veins. The inner walls of these are lined with smooth muscles, allowing for ...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
One of the crucial types of surgery is the heart surgery, which is commonly known as the bypass. It is a type of surgery in which the chest is cut, and surgery is done on valves, muscles, and heart arteries. As per the National Heart, Lung, and Blood Institute, it is one of the most common types of surgeries, which is performed on adults. During this surgery, the prime focus is to remove the blockage from the heart so that fresh blood can easily flow into the heart. No doubt that this process is...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The word acute coronary syndrome refers to a group of symptoms that are caused by blockage of the blood flow to the heart muscles. The most common result of this is myocardial infarction or heart attack as it is popularly called. Reduced blood flow leads to death of some portion of the heart muscle wall. While the word heart attack sounds almost fatal, it need not be the case. Knowing how to identify an attack and being aware of some simple measures can help save lives.
Symptoms:
more
Symptoms:
more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
The Mini-Gastric Bypass or in other words, Single Anastomosis Gastric Bypass is an extremely effective and a well-established procedure that combines some of the properties of two other bariatric surgeries:
A Gastric Sleeve
A Standard Gastric Bypass
The upper half of the stomach gets divided into a tube, quite similar to the top three-quarters of a sleeve and then it gets joined to a loop of intestine. This Mini-Gastric Bypass can be made use of as one of the most primary proce...more
A Gastric Sleeve
A Standard Gastric Bypass
The upper half of the stomach gets divided into a tube, quite similar to the top three-quarters of a sleeve and then it gets joined to a loop of intestine. This Mini-Gastric Bypass can be made use of as one of the most primary proce...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Obesity can make life miserable. From unhealthy eating habits to unhealthy lifestyles and medical conditions, obesity can be an amalgamation of many factors. Obese people are at a greater risk of suffering from many serious health complications like type-2 diabetes, mood swings, and depression, cardiac problems, high blood pressure and high cholesterol, to name a few. It does not stop there. More alarming is the fact that obese people are at increased risk of suffering from different types of ca...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
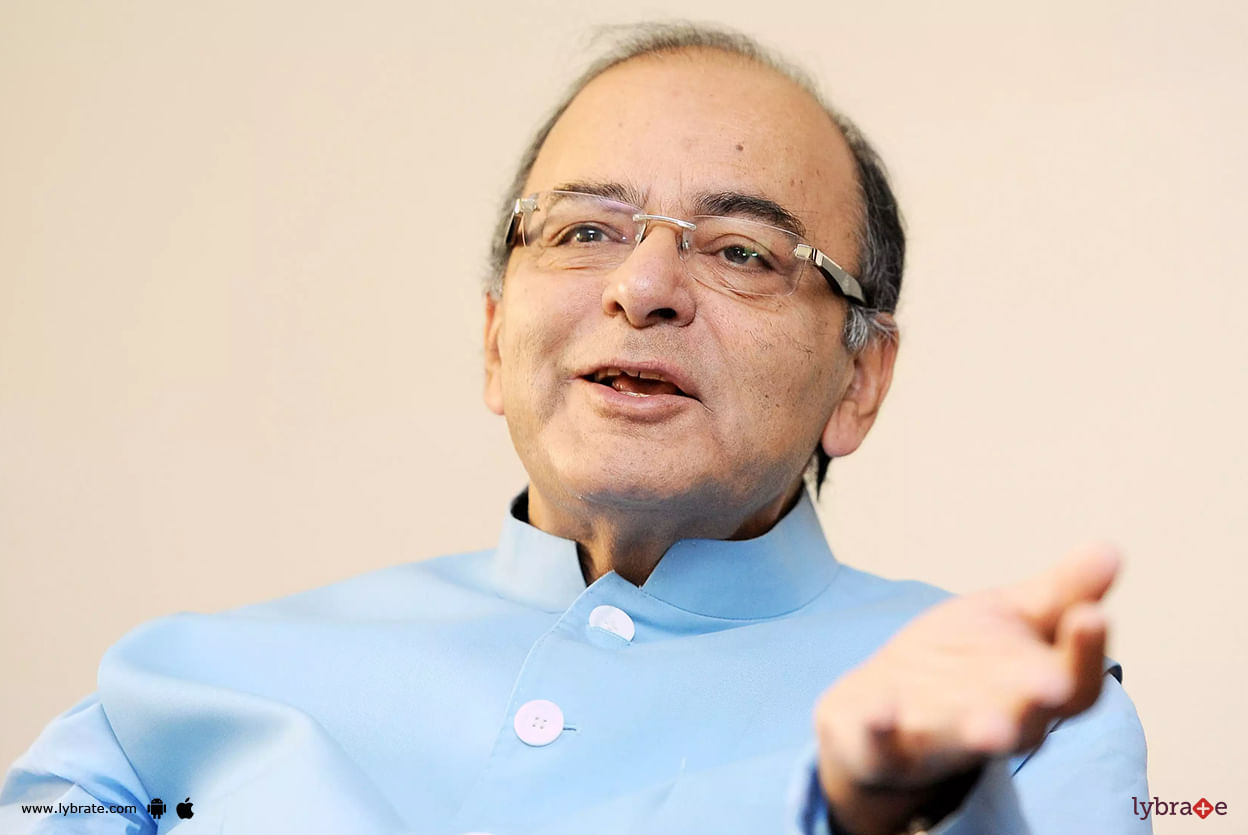
Arun Jaitley, 66 the former finance minister and a stalwart of the Bharatiya Janata Party, died on 24th August 2019, Saturday, at 12:07 pm.
Arun Jaitley got admitted in AIIMS, New Delhi in August 2019 when he suffered from severe uneasiness and breathlessness. On 17 August, it was reported that Jaitley was on life-support. By 23 August, his health had deteriorated leading to his demise.
Jaitley had been unwell for a large part of the last two years when his condition took a ...more
Arun Jaitley got admitted in AIIMS, New Delhi in August 2019 when he suffered from severe uneasiness and breathlessness. On 17 August, it was reported that Jaitley was on life-support. By 23 August, his health had deteriorated leading to his demise.
Jaitley had been unwell for a large part of the last two years when his condition took a ...more
Book appointment with top doctors for Bypass Surgery treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously