Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Bleeding Tips
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Gynaecologist•Mumbai
Heavy bleeding or menorrhagia is a condition that is characterized by an abnormally heavy or prolonged bleeding that requires a woman to change her sanitary pads every one to two hours during her menstruation cycle. Due to the condition a woman can lose a lot of blood in the form of huge blood clots, resulting in anemia, fatigue, weakness, breathlessness, mood swing and other health problems if continued for a longer period of time. ;
Menorrhagia can be a ...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
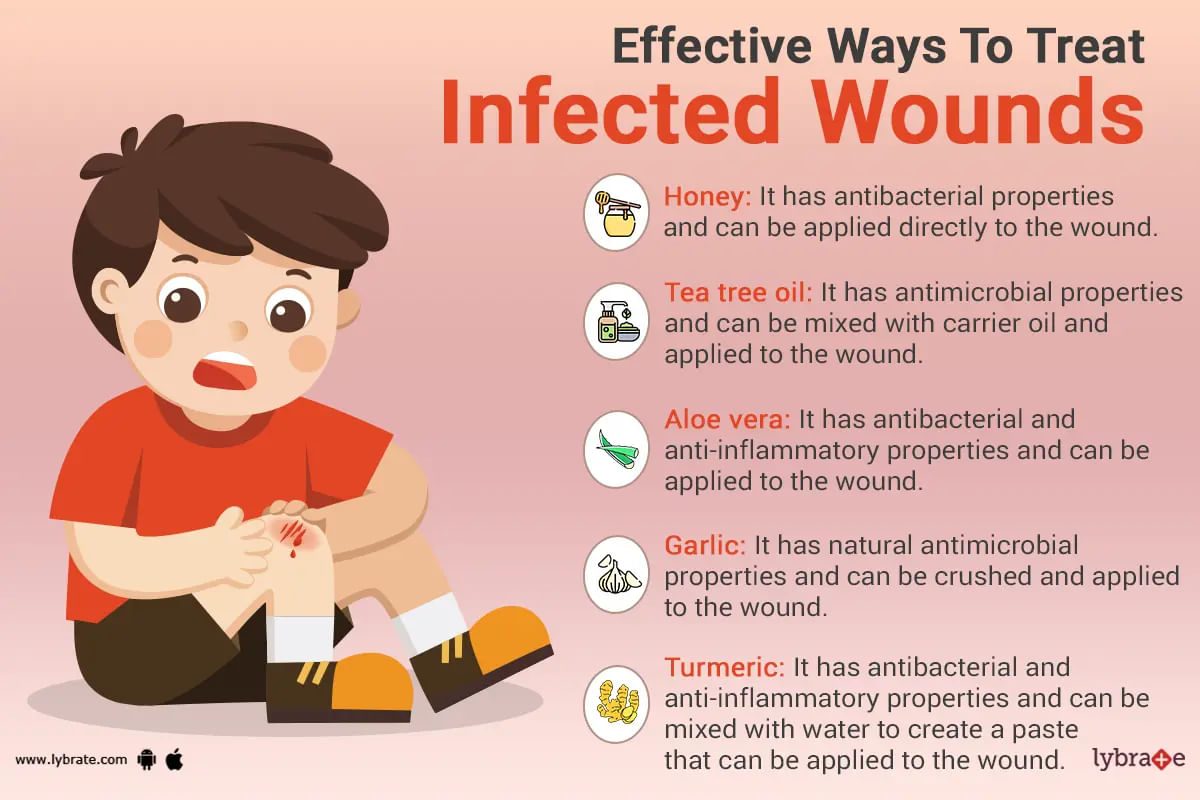
Minor cuts and wounds are inevitable and bound to come about every now and then. However, it is important to clean them immediately with lukewarm water and soap to prevent infection. If a wound still gets infected by any means, however, soap and water will no longer suffice; it may be time to seek medical attention or try some effective natural remedies.
Some signs that warrant medical treatment include a large amount of pus in the wound, the fact that the wound does...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Overall oral health consists of the health of both the soft and the hard tissues in the mouth. While teeth are the hard tissues, the soft tissues include the lips, tongue, cheek, palate, and most importantly the gums. The gums or the periodontium (peri - around, dont - tooth) surrounds the tooth and provides nutritional support and structural support with its connective tissue. The gums are the unsung heroes in maintaining a healthy set of teeth.
It is the common observation that denta...more
It is the common observation that denta...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
Gum bleeding is a severe kind of oral trouble and it needs to be resolved as soon as possible otherwise it might get converted into a serious issue. There are some simple ways by means of which bleeding gums can be stopped.
5 ways to prevent bleeding of gums
Have a healthy diet: Oral health can only be preserved well by maintaining a healthy diet, and this can also prevent bleeding gums. Fruits and veggies are included in this kind of diet. These foods offer necessary nutrients...more
5 ways to prevent bleeding of gums
Have a healthy diet: Oral health can only be preserved well by maintaining a healthy diet, and this can also prevent bleeding gums. Fruits and veggies are included in this kind of diet. These foods offer necessary nutrients...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
It is gastrointestinal bleeding in the upper gastrointestinal tract, commonly defined as bleeding arising from the esophagus, stomach, or duodenum. Blood is often observed in vomit (hematemesis) or in the stool (melena). Upper gastrointestinal bleeding denotes a medical emergency and typically requires hospital care for primary diagnosis and treatment. The incidence of upper gastrointestinal bleeding is 50-150 individuals per 100,000 annually. Depending on its severity, it carries an estimated m...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
1. Upper GI bleeding: Vomiting of blood, coffee-coloured vomitus, or the passing of black stools is called Hematemesis. It is a medical emergency and requires urgent admission to hospital and evaluation by a gastroenterologist. Medical stabilisation by medicines to stop bleeding and blood transfusion are required initially. Gastroscopy is required for finding the cause of bleeding as well as treatment. Gastric ulcer or duodenal ulcer requires injection adrenaline or hemoclips. Esophageal varices...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
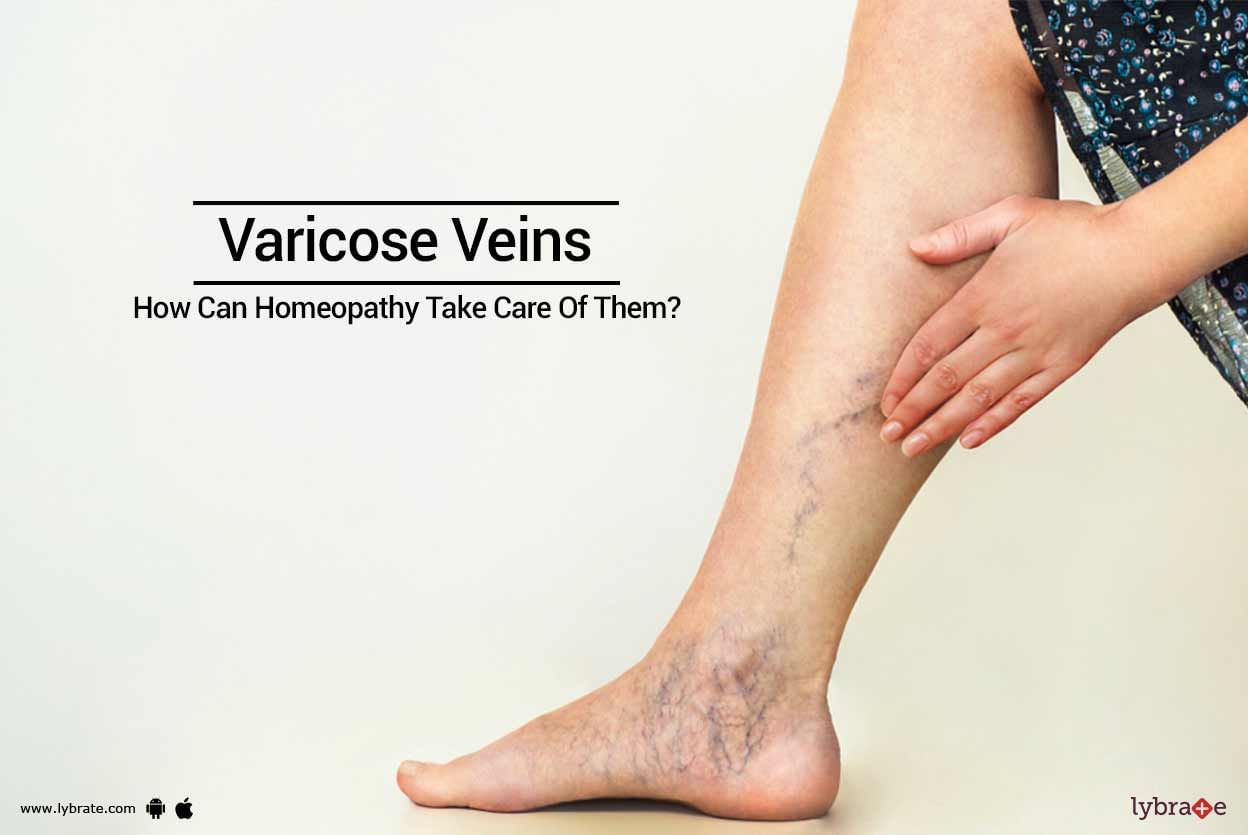
Blood vessels are normally hidden under the skin, but a common complaint of people who stand for long durations of time is the appearance of bluish veins on their legs. In most cases, these veins appear twisted and enlarged. This condition is known as varicose veins. Pregnant women also often suffer from this condition.
Causes of Varicose Veins:
Occupational: Standing long hours
Genetic tendency
Deep vein thrombosis: A condition which affects the valves of vei...more
Causes of Varicose Veins:
Occupational: Standing long hours
Genetic tendency
Deep vein thrombosis: A condition which affects the valves of vei...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Do you know about the ill effects and various serious consequences that are associated with endometriosis?
In this disorder, there is a presence of endometrium (lining of uterus) outside uterus. It is likely to spread to ovaries and other nearby areas. It can involve any other part of the body also. Endometriosis, at times, causes great pain and may result in infertility.
Causes
The exact cause of endometriosis is not known.
It may occur because of a process, k...more
In this disorder, there is a presence of endometrium (lining of uterus) outside uterus. It is likely to spread to ovaries and other nearby areas. It can involve any other part of the body also. Endometriosis, at times, causes great pain and may result in infertility.
Causes
The exact cause of endometriosis is not known.
It may occur because of a process, k...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
Presently human dentition plays a major role in enhancing the facial aesthetics and overall personality of an individual.
Good dentition not only helps a person to chew food efficiently but also maintains the facial value and phonetics.
Nowadays I see patients coming up with a common complaint of bad breath, swollen gums, bleeding gums, food impaction between teeth, blackening and staining of teeth, sensitivity on intake of hot and cold beverages even after brushing efficiently...more
Good dentition not only helps a person to chew food efficiently but also maintains the facial value and phonetics.
Nowadays I see patients coming up with a common complaint of bad breath, swollen gums, bleeding gums, food impaction between teeth, blackening and staining of teeth, sensitivity on intake of hot and cold beverages even after brushing efficiently...more
Last Updated: 6 years ago• Featured Tip
Share
Bookmark
Report
MBBS (Gold Medalist), MS- General Surge...read more
Surgical Gastroenterologist•Kolkata
If you notice blood in the stool or the toilet bowl, it could be a case of rectal bleeding. There are many reasons why rectal bleeding can occur, the most common one being haemorrhoids. If the rectal bleeding is not significant then it is not a cause for concern. But if you lose a lot of blood then it can be a major problem.
What are the signs?
The most obvious one, in this case, is the presence of blood in your stool. But it's not just the presence of blood that is important h...more
What are the signs?
The most obvious one, in this case, is the presence of blood in your stool. But it's not just the presence of blood that is important h...more
Book appointment with top doctors for Bleeding treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously