Get the App
For Doctors
Login/Sign-up
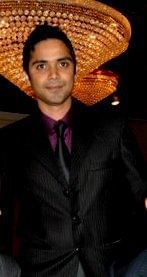
Dr. Mayank Jain
Physiotherapist20 Years Exp.
MS in Exercise physiology, BPTh/BPT
Mumbai
₹ 700 at clinic
Stride Fitness and Mobility Clinic
113, E-Square, Above State Bank Of India, Subhash Road, Vile Parle ( E)
Consultation Fee: ₹ 700
View All Slots
Personal Statement
In my 9 years of academic and clinical experience in India and USA , most I learned is from my patients . College and work taught me good clinical skill but my patients nurtured me with the real meaning of life...read more
Doctor Information
Speciality
- Physiotherapist
Other treatment areas
- Homecare Physiotherapist
- Orthopedic Physiotherapist
- Sports and Musculoskeletal Physiotherapist
Education
- MS in Exercise physiology , University of Texas at Arlington, USA , 2009
- BPTh/BPT , Devi Ahilya University , Indore , 2006
Languages spoken
- English
- Hindi
Clinic Location
113, E-Square, Above State Bank Of India, Subhash Road, Vile Parle ( E)
Clinic of Dr. Mayank Jain
| Clinic's Name | Fees |
|---|---|
| Stride Fitness and Mobility Clinic | ₹ 700 |
Get Help
Services
Book Clinic Appointment with Dr. Mayank Jain
Stride Fitness and Mobility Clinic
113, E-Square, Above State Bank Of India, Subhash Road, Vile Parle ( E)
₹ 700 at clinic
Unavailable today