Get the App
For Doctors
Login/Sign-up
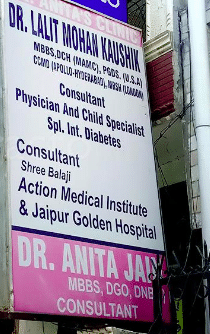
Dr. Anita Kaushik
Gynaecologist27 Years Exp.
MBBS DGO DNB
Delhi
₹ 600 at clinic
₹ 800 online
Dr. Anita's Mother And Child Clinic
#A-3/309, Ground Floor, Pashchim Vihar. Landmark: Near Shiv Modern School
Consultation Fee: ₹ 600
View All Slots
Personal Statement
I believe in health care that is based on a personal commitment to meet patient needs with compassion and care...read more
Doctor Information
Speciality
- Gynaecologist
Other treatment areas
- Gynaecologist
Education
- MBBS DGO DNB , Punjab University , 1999
Languages spoken
- English
- Hindi
Professional Memberships
- Delhi Medical Council
- Association of Obstetricians & Gynaecologists of Delhi (AOGD)
- Controversies in Obstetrics
- Gynecology and Infertility (COGI)
Clinic Location
#A-3/309, Ground Floor, Pashchim Vihar. Landmark: Near Shiv Modern School
Clinic of Dr. Anita Kaushik
| Clinic's Name | Fees |
|---|---|
| Dr. Anita's Mother And Child Clinic | ₹ 600 |
Get Help
Reviews
Services
Book Clinic Appointment with Dr. Anita Kaushik
Dr. Anita's Mother And Child Clinic
#A-3/309, Ground Floor, Pashchim Vihar. Landmark: Near Shiv Modern School
₹ 600 at clinic
See all timings