Get the App
For Doctors
Login/Sign-up
Dr. K Sharath Kumar Shetty
Radiologist
Bangalore
₹ at clinic
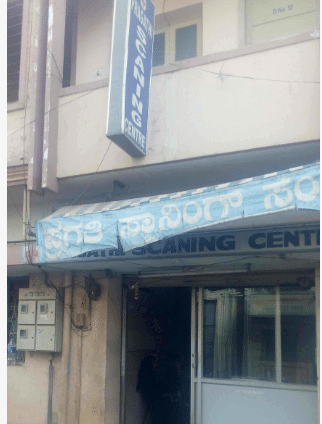
Pragathi Scanning Centre
#1303, Y M Gopalappa Building, Santhe Circle, BB Road, Yelahanka. Landmark: Near Corporation Bank ATM
View All Slots
Personal Statement
I believe in health care that is based on a personal commitment to meet patient needs with compassion and care...read more
Doctor Information
Speciality
- Radiologist
Other treatment areas
- Implantologist
Languages spoken
- English
Clinic Location
#1303, Y M Gopalappa Building, Santhe Circle, BB Road, Yelahanka. Landmark: Near Corporation Bank ATM
Clinic of Dr. K Sharath Kumar Shetty
| Clinic's Name | Fees |
|---|---|
| Pragathi Scanning Centre | - |
Get Help
Services
Book Clinic Appointment with Dr. K Sharath Kumar Shetty
Pragathi Scanning Centre
#1303, Y M Gopalappa Building, Santhe Circle, BB Road, Yelahanka. Landmark: Near Corporation Bank ATM
See all timings