Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Heart Tips
Last Updated: 2 years ago• Featured Tip
Share
Bookmark
Report
All cardio type exercises come in aerobic exercise for example brisk walking, swimming, running, cycling. Aerobic means activities with oxygen. These exercises increase the breathing and heart rate which in turn keep your heart, lungs, and circulatory system active and healthy. These exercises also prevent us from many heart and lung diseases.
There is anaerobic exercise which differs from aerobic. In anaerobic weight lifting, sprinting, running are the exercises. Th...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
क्या होती है पल्स रेट
आपकी हृदय गति, या पल्स रेट, आपके दिल की प्रति मिनट धड़कन की संख्या है। सामान्य पल्स रेट एक व्यक्ति से दूसरे व्यक्ति में भिन्न हो सकती है। अपने को जानना एक महत्वपूर्ण ह्रदय-स्वास्थ्य का संकेत हो सकता है। यह जरुरी नहीं है पल्स रेट का पता तभी लगाया जाय जब आप एथलीट हों।
यहां तक कि अगर आप एथलीट नहीं हैं, तो आपकी हृदय गति के बारे में ज्ञान आपको अपने फिटनेस स्तर पर नजर रखने में मदद कर सकता है। यह आपको स्वास्थ्य समस्याओं के बारे में समझ को विकसित करने ...more
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Ayurvedic Doctor•Lucknow
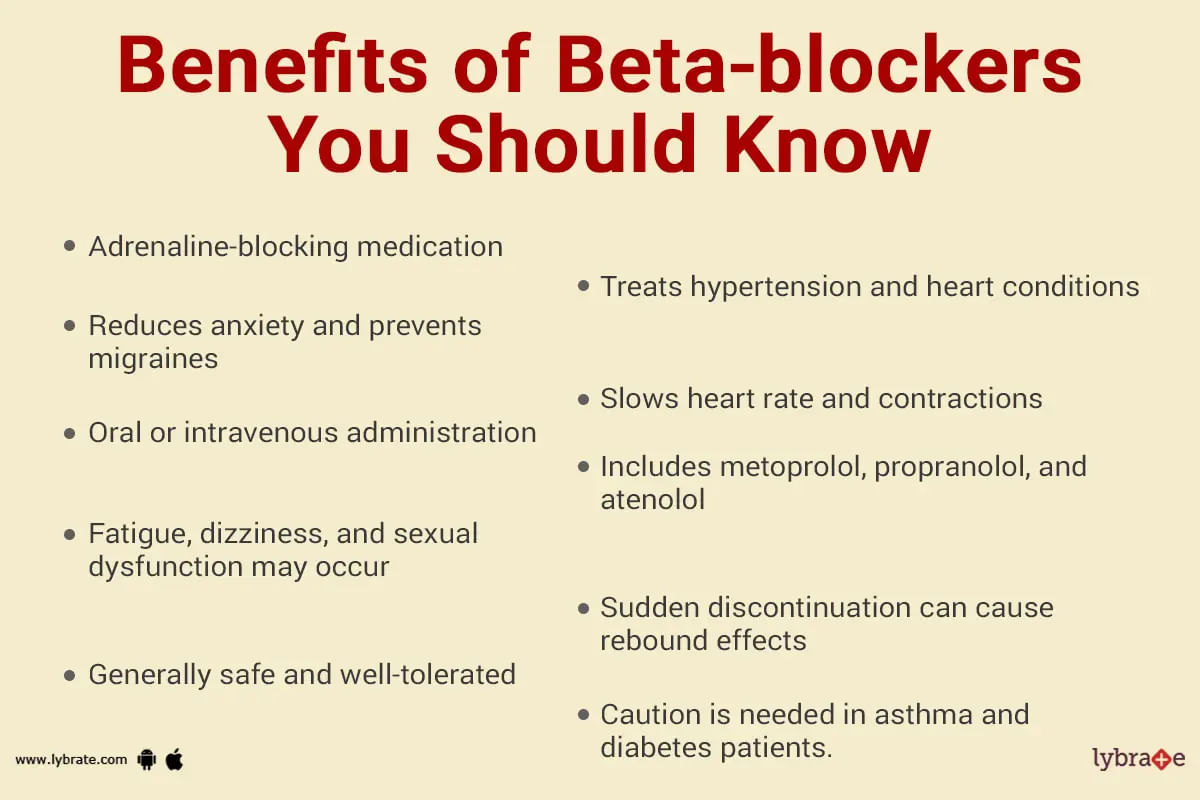
Beta-blockers are basically a category of drugs that are predominantly used to reduce stress and strain on the heart. They work by blocking the effects of adrenaline, which simply means that a person's heart does not have to work as hard (as earlier) to pump blood around the body. This can be helpful for people who have certain heart conditions or who are experiencing some other related health issues, such as anxiety and stress.
In other words, beta blockers are a cl...more
1133 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
1. Dr. Rajiv bajaj
Https://wwaw. Lybrate. Com/delhi/doctor/dr-rajiv-bajaj-cardiologist-1
Mbbs, md - internal medicine, dm - cardiology, fellowship in ep
42 years experience 700 - 1600 at clinic 500 online
He is known for his knowledge as an expert in cardiovascular disorders and is a respected doctor in the field of atrial and vascular diseases. For many years, he has also been providing cardiac electrophysiology services to patients. As an experienced ...more
Https://wwaw. Lybrate. Com/delhi/doctor/dr-rajiv-bajaj-cardiologist-1
Mbbs, md - internal medicine, dm - cardiology, fellowship in ep
42 years experience 700 - 1600 at clinic 500 online
He is known for his knowledge as an expert in cardiovascular disorders and is a respected doctor in the field of atrial and vascular diseases. For many years, he has also been providing cardiac electrophysiology services to patients. As an experienced ...more
18 people found this helpful
Last Updated: 3 years ago• Featured Tip
Share
Bookmark
Report
Cardiologist•Bangalore
Choosing the appropriate heart specialist is crucial for you since, as you are aware, heart illnesses cannot be handled lightly because your life is at risk.
Dr. Kumar B
DM - Cardiology, MD - General Medicine, MBBS
52 Years Experience 500 at clinic 300 online
The most renowned cardiologist in Bangalore with more than 52 years of expertise is Dr. Kumar B. He earned his DM in cardiology in 1987, making him a superspecialist in the subject. His academic background comp...more
Dr. Kumar B
DM - Cardiology, MD - General Medicine, MBBS
52 Years Experience 500 at clinic 300 online
The most renowned cardiologist in Bangalore with more than 52 years of expertise is Dr. Kumar B. He earned his DM in cardiology in 1987, making him a superspecialist in the subject. His academic background comp...more
14 people found this helpful
Last Updated: 4 years ago• Featured Tip
Share
Bookmark
Report
Inherited cardiac ;conditions refer to those cardiac conditions that you inherit from your parents. These are also referred to as inherited heart conditions or genetic heart disorders. Inherited cardiac conditions are often life-threatening and can affect anyone at any age.
Genetics play a vital role in influencing the risk of cardiac diseases in more than one way. From the robustness of the blood vessels to the way the cells in your heart communicate the genes control every aspect of...more
Genetics play a vital role in influencing the risk of cardiac diseases in more than one way. From the robustness of the blood vessels to the way the cells in your heart communicate the genes control every aspect of...more
44 people found this helpful
Last Updated: 4 years ago• Featured Tip
Share
Bookmark
Report
Your heart is responsible for pumping blood throughout your body and supplying nutrients and oxygen to the tissues. For the proper functioning of your body, it is essential to keep your heart healthy. However, over time, a number of underlying causes and conditions affect your heart health.
Here are a few factors that impact your heart in one way or the other
Cholesterol the first thing you need to know about cholesterol is that it is of two types good and bad...more
Here are a few factors that impact your heart in one way or the other
Cholesterol the first thing you need to know about cholesterol is that it is of two types good and bad...more
5 people found this helpful
Last Updated: 4 years ago• Featured Tip
Share
Bookmark
Report
A healthy heart beats 60-100 times per minute. Normally, every muscle contraction of the heart is controlled by electrical signals that travel from the heart s upper chambers to the lower ones. A heart blockage disrupts the flow of electrical signals of the heart.
Heart blockage is partial when the electrical impulses are stopped or delayed, preventing the heart from beating regularly. A complete blockage, on the other hand, occurs when the electrical signals come to a halt completely. ...more
Heart blockage is partial when the electrical impulses are stopped or delayed, preventing the heart from beating regularly. A complete blockage, on the other hand, occurs when the electrical signals come to a halt completely. ...more
Last Updated: 4 years ago• Featured Tip
Share
Bookmark
Report
A low heart rate, known as bradycardia, is common in adults. As you age, the electrical system of the heart undergoes wear-and-tear, and the normal rhythm of your heart slows down. In most cases, it does not seem like a serious condition. However, if your heart rate slows down considerably, you might want to check up with your doctor at the earliest.
How slow is too slow?
A normal heart rate ranges from 60 to 100 beats every minute, while awake. People with bradycardia experien...more
How slow is too slow?
A normal heart rate ranges from 60 to 100 beats every minute, while awake. People with bradycardia experien...more
9 people found this helpful
Last Updated: 4 years ago• Featured Tip
Share
Bookmark
Report
A heart attack can be devastating, even fatal in the absence of immediate medical attention. Keeping your heart healthy is important if you are looking to enjoy a long and peaceful life. However, in order to maintain a healthy heart, you need to know some common triggers for your cardiac muscles.
A heart attack may be caused due to one of the following three reasons-
Atherosclerosis - Atherosclerosis is the condition where the artery carrying blood to the heart is blocked due t...more
A heart attack may be caused due to one of the following three reasons-
Atherosclerosis - Atherosclerosis is the condition where the artery carrying blood to the heart is blocked due t...more
Book appointment with top doctors for Heart treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously