Get the App
For Doctors
Login/Sign-up
About
Health Feed
Find Doctors
Health Packages
AllQ&AsTipsQuizzes
Acute Infection Tips
Last Updated: 4 years ago• Featured Tip
Share
Bookmark
Report
As we go about life and routine activities, we may be exposed to a lot of different types of environments. We may have to travel in heavy traffic and may be exposed to vehicular pollution, there may be times when we are at places that allow smoking and that may expose us to smoke from cigarettes. Our nature of work today requires us to be constantly in a situation where we take in industrial fumes and exhausts. Being in any of these conditions temporarily may not be a big matter of worry, but wh...more
Last Updated: 4 years ago• Featured Tip
Share
Bookmark
Report
Infection is generally understood as the invasion into the body tissues of an organism by certain foreign bodies such as bacteria, parasite, and virus. They are transmissible diseases and can be transmitted from one person to the other via sneezing, coughing or physical contact. They can be mild, moderate or severe.
* They can be acute, that is, can last for a short time, or chronic that lasts for a long time, or a latent infection that may not cause any symptoms at first but reactivate...more
* They can be acute, that is, can last for a short time, or chronic that lasts for a long time, or a latent infection that may not cause any symptoms at first but reactivate...more
Last Updated: 4 years ago• Featured Tip
Share
Bookmark
Report
As we go about life and routine activities, we may be exposed to a lot of different types of environments. We may have to travel in heavy traffic and may be exposed to vehicular pollution, there may be times when we are at places that allow smoking and that may expose us to smoke from cigarettes. Our nature of work today requires us to be constantly in a situation where we take in industrial fumes and exhausts. Being in any of these conditions temporarily may not be a big matter of worry, but wh...more
Last Updated: 4 years ago• Featured Tip
Share
Bookmark
Report
As we go about life and routine activities, we may be exposed to a lot of different types of environments. We may have to travel in heavy traffic and may be exposed to vehicular pollution, there may be times when we are at places that allow smoking and that may expose us to smoke from cigarettes. Our nature of work today requires us to be constantly in a situation where we take in industrial fumes and exhausts. Being in any of these conditions temporarily may not be a big matter of worry, but wh...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
The infection of the bone of the ear is Mastoiditis. This may be an acute infection needing hospitalisation and injectable drugs or may be in the form of slow bone eroding processes like cholesteatoma.
Let us learn more about this condition and its treatment:
Understanding the mastoid bone:
The mastoid bone is made up of air sacs and it looks a lot like a sponge. In this sense, it is different from the other bones that can be found in the human body. In order to functi...more
Let us learn more about this condition and its treatment:
Understanding the mastoid bone:
The mastoid bone is made up of air sacs and it looks a lot like a sponge. In this sense, it is different from the other bones that can be found in the human body. In order to functi...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
We are bombarded with advertisements of how 'good mothers' never fail to have their children use antibacterial soap as a habit. But does it really work? There have been several reports of potentially harmful ingredients being used in these antibacterial soaps and yet their sale continues unhindered. Let's dive in to get the dope behind these soaps
What are antibacterial soaps?
A drug called 'triclosan' was originally used strictly in hospital environments. In the 1990s the comm...more
What are antibacterial soaps?
A drug called 'triclosan' was originally used strictly in hospital environments. In the 1990s the comm...more
Last Updated: 5 years ago• Featured Tip
Share
Bookmark
Report
A hot summer s day may just be the perfect excuse to turn the air conditioning at full blast, and gorge on junk food like a plate of Golgapas and samosas, followed by a bottle of chilled soft drink.
Hold that thought! The number of people seeking treatment for various gastrointestinal (GI) infections, i.e stomach infection, rise by approximately 40% during the peak summer. One of the major reasons attributed to GI infections is excessive consumption of junk and contaminated food. Add de...more
Hold that thought! The number of people seeking treatment for various gastrointestinal (GI) infections, i.e stomach infection, rise by approximately 40% during the peak summer. One of the major reasons attributed to GI infections is excessive consumption of junk and contaminated food. Add de...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
The infection of the bone of the ear is Mastoiditis. This may be an acute infection needing hospitalisation and injectable drugs or may be in the form of slow bone eroding processes like cholesteatoma.
Let us learn more about this condition and its treatment
Understanding the mastoid bone: The mastoid bone is made up of air sacs and it looks a lot like a sponge. In this sense, it is different from the other bones that can be found in the human body. In order to function properl...more
Let us learn more about this condition and its treatment
Understanding the mastoid bone: The mastoid bone is made up of air sacs and it looks a lot like a sponge. In this sense, it is different from the other bones that can be found in the human body. In order to function properl...more
Last Updated: 7 years ago• Featured Tip
Share
Bookmark
Report
Infection is generally understood as the invasion into the body tissues by certain foreign bodies, such as bacteria, parasite and virus. They are transmissible diseases and can be transmitted from one person to the other via sneezing, coughing or physical contact. They can be mild, moderate or severe.
1. They can be acute that is can last for a short time or chronic that lasts for a long time or a latent infection that may not cause any symptoms at first but reactivates and resurfaces o...more
1. They can be acute that is can last for a short time or chronic that lasts for a long time or a latent infection that may not cause any symptoms at first but reactivates and resurfaces o...more
Last Updated: 10 months ago• Featured Tip
Share
Bookmark
Report
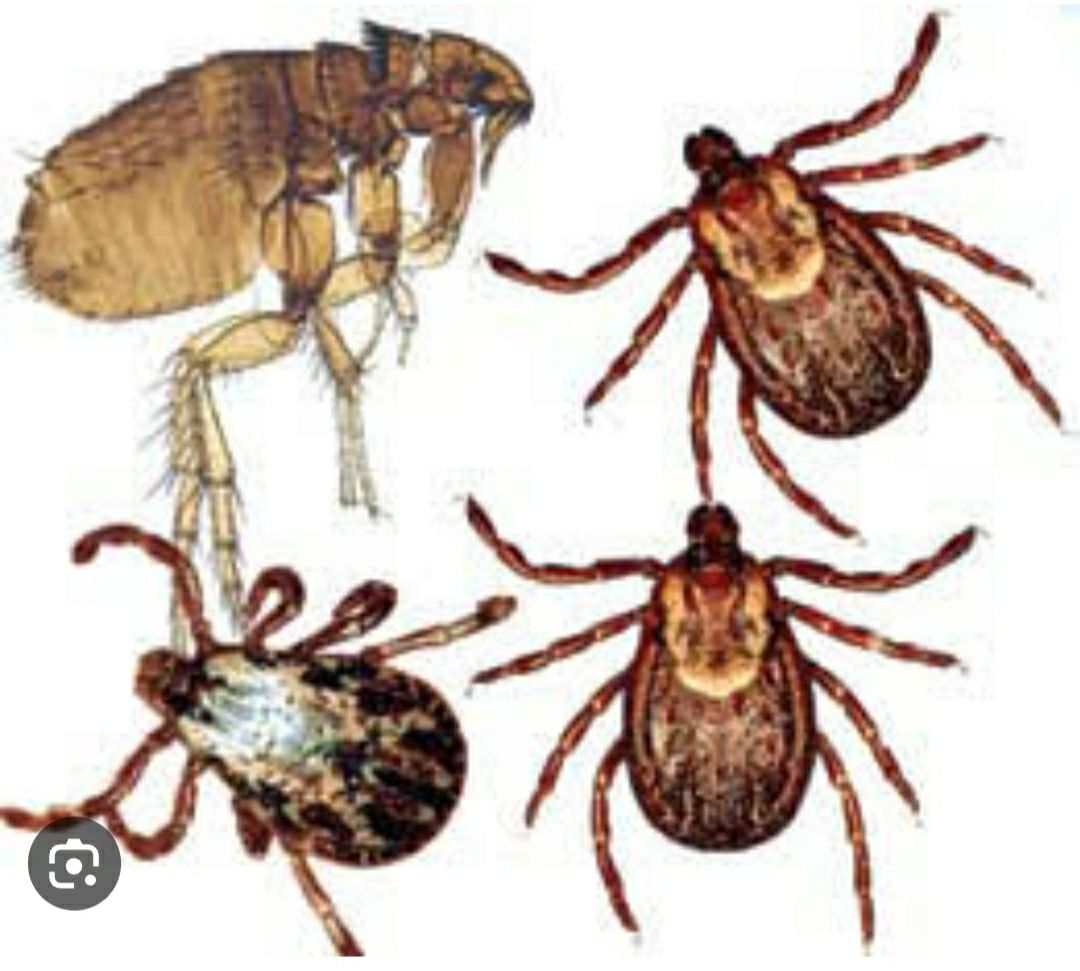
There are several ectoparasites that can pose a life-threatening risk to dogs if left untreated. Here are three significant examples:
Fleas (ctenocephalides spp.): while fleas are common and often considered a nuisance, a severe infestation can lead to life-threatening conditions. Fleas can cause anemia, especially in young or small dogs, due to excessive blood loss. Some dogs may develop an allergic reaction to flea bites, leading to a condition called flea allergy dermatitis (fad...more
Last Updated: 10 months ago• Featured Tip
Share
Bookmark
Report
Monitoring for signs of illness in your dog is crucial for detecting health issues early and seeking appropriate veterinary care. Here are some key areas to focus on when monitoring your dog's health:
Changes in appetite: monitor your dog's eating habits. Significant changes in appetite, such as a sudden loss of interest in food or excessive hunger, could indicate an underlying health problem.
Water intake: notice if your dog is drinking more or less water than usual. Increased...more
Changes in appetite: monitor your dog's eating habits. Significant changes in appetite, such as a sudden loss of interest in food or excessive hunger, could indicate an underlying health problem.
Water intake: notice if your dog is drinking more or less water than usual. Increased...more
Last Updated: 10 months ago• Featured Tip
Share
Bookmark
Report
Chronic respiratory diseases like bronchial asthma, bronchiectasis, copd, sarcoidosis and interstitial lung disease are vulnerable to repeated infections and multiple hospital visits or admission.
The main reasons for the increased susceptibility is altered lung defence, use of steroids in various respiratory conditions and multiple comorbidities like diabetes and coronary disease.
Patients should ideally be vaccinated for pneumococcal and influenza disease routinely.
The main reasons for the increased susceptibility is altered lung defence, use of steroids in various respiratory conditions and multiple comorbidities like diabetes and coronary disease.
Patients should ideally be vaccinated for pneumococcal and influenza disease routinely.
Last Updated: 1 year ago• Featured Tip
Share
Bookmark
Report
What is upper respiratory tract infection?
Upper respiratory tract infection (uri) is a contagious infection of the nose, throat, and airways.
Uris are caused by viruses the vast majority of the time; however, bacteria are also capable of becoming the offender in some situations.
Types of upper respiratory tract infection:
Sinusiti: sinusitis is a form of infection of the upper respiratory system that affects the sinuses. It is caused by ...more
41 people found this helpful
Last Updated: 1 year ago• Featured Tip
Share
Bookmark
Report
शरीर में कई तरह के भीतरी अंग होते हैं जो हमारे शरीर को सुचारु रूप से चलाने में मदद करते हैं। शरीर में मौजूद इन अंगों का अपना एक अलग कार्य होता है। शरीर में ऐसा ही एक अंग होता है मूत्राशय, जो शरीर के विषाक्त पदार्थों या अपशिष्ट को शरीर से बाहर निकालने में सहयोग करता है। व्यक्ति के लिए मूत्राशय को स्वस्थ रखना बहुत जरूरी होता है।
तो चलिए आज आपको कुछ ऐसे तरीके बताते हैं, जो आपको मूत्राशय को स्वस्थ रखने में आपकी काफी सहायता करते हैं। हालांकि इसके पहले आप यह जान लीजिये कि यह मूत्राशय होता क्य...more
तो चलिए आज आपको कुछ ऐसे तरीके बताते हैं, जो आपको मूत्राशय को स्वस्थ रखने में आपकी काफी सहायता करते हैं। हालांकि इसके पहले आप यह जान लीजिये कि यह मूत्राशय होता क्य...more
38 people found this helpful
Last Updated: 1 year ago• Featured Tip
Share
Bookmark
Report
What is ear, nose, and throat disorders?
Ear, nose, and throat (ent) disorders are a group of conditions that affect the areas of the head and neck. Examples of common ent disorders include chronic sinusitis, ear infections, dizziness, allergies, hearing loss, hoarseness or voice problems, neck masses, throat infection or pain and tonsil swelling. ;
Many of these conditions can cause significant discomfort and impair your quality of life. Treatment can somet...more
Last Updated: 1 year ago• Featured Tip
Share
Bookmark
Report
जब किसी भी तरह की बीमारी के इलाज की बात आती है तो दवाइयों और इंजेक्शन का जिक्र होना स्वाभाविक है। दरअसल, कई बार जब हम बीमारी का इलाज कराने के लिए डॉक्टर के पास जाते हैं तो डॉक्टर कई तरह की दवाइयों और इजेक्शन लेने की सलाह देता है और हम इन इंजेक्शन को लेकर लगवाते भी हैं।
क्या आपको मालूम है कि इंजेक्शन लगाने के अलग-अलग तरीके भी होते हैं। ऐसा ही एक तरीका है सबक्यूटेनियस इंजेक्शन। तो चलिए आज हम इस सबक्यूटेनियस इंजेक्शन के विषय में विस्तार से बात करते हैं।
क्या है सबक्यूटेनियस इंजेक्...more
क्या आपको मालूम है कि इंजेक्शन लगाने के अलग-अलग तरीके भी होते हैं। ऐसा ही एक तरीका है सबक्यूटेनियस इंजेक्शन। तो चलिए आज हम इस सबक्यूटेनियस इंजेक्शन के विषय में विस्तार से बात करते हैं।
क्या है सबक्यूटेनियस इंजेक्...more
Last Updated: 1 year ago• Featured Tip
Share
Bookmark
Report
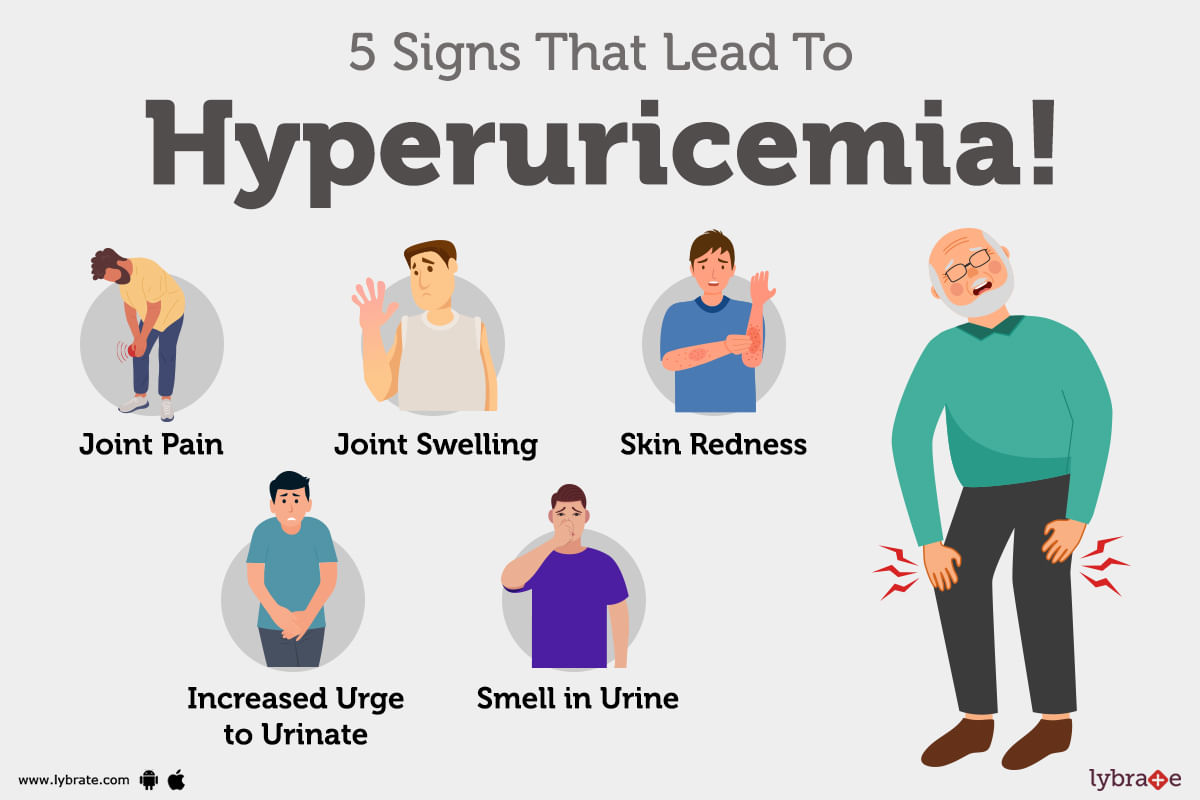
When there are high levels of uric acid in the blood a condition occurs called hyperuricemia. When there are high levels of uric acid in the blood it can lead to many diseases like highly painful arthritis disease called gout.
High uric acid can lead to many more health problems like kidney diseases, heart diseases and a few more. ;
Purines are nucleic acid ring structure bases. When these purines break down in the body uric acids are formed. Thes...more
Last Updated: 1 year ago• Featured Tip
Share
Bookmark
Report
As a pregnant woman, maintaining good hygiene is crucial for the health and well-being of both you and your baby. Taking care of your intimate area is an important part of this. From increased vaginal discharge to the risk of infections, pregnancy can bring about many changes to your body. That's why we've put together this guide on how to clean your private parts during pregnancy. Follow these tips to keep your intimate area clean, healthy, and comfortable throughout your pr...more
Last Updated: 1 year ago• Featured Tip
Share
Bookmark
Report
Dermatologist•Kolkata
1. Dr. Anusree gangopadhyay
Https://www. Lybrate. Com/kolkata/doctor/dr-anusree-gangopadhyay-dermatologist
Mbbs, md - dermatology, specialty certificate, dermatology (uk)
14 years experience 600 - 990 at clinic
Dr. Anusree gangopadhyay is a renowned dermatologist who possesses a dermatology specialty certificate from the royal college of physicians and surgeons of the united kingdom. She earned a gold medal in medicine during her mbbs ...more
Book appointment with top doctors for Acute Infection treatment
View fees, clinic timings and reviews
Ask a free question
Get FREE multiple opinions from Doctors
posted anonymously